Beth’s Relapsed Refractory Multiple Myeloma Story
Diagnosis: Multiple myeloma, relapsed/refractory
Subtype: Non-secretory (1-5% of myelomas)
1st Symptoms: Extreme pain between shoulder blades, sternum, head, burning sensation
1st Line Treatment: VAD chemo, radiation, stem cell transplant
RR Treatment: 8 chemo regimens, successful combo→selinexor+bortezomib+dexamethasone

Beth’s Relapsed Refractory Multiple Myeloma Story

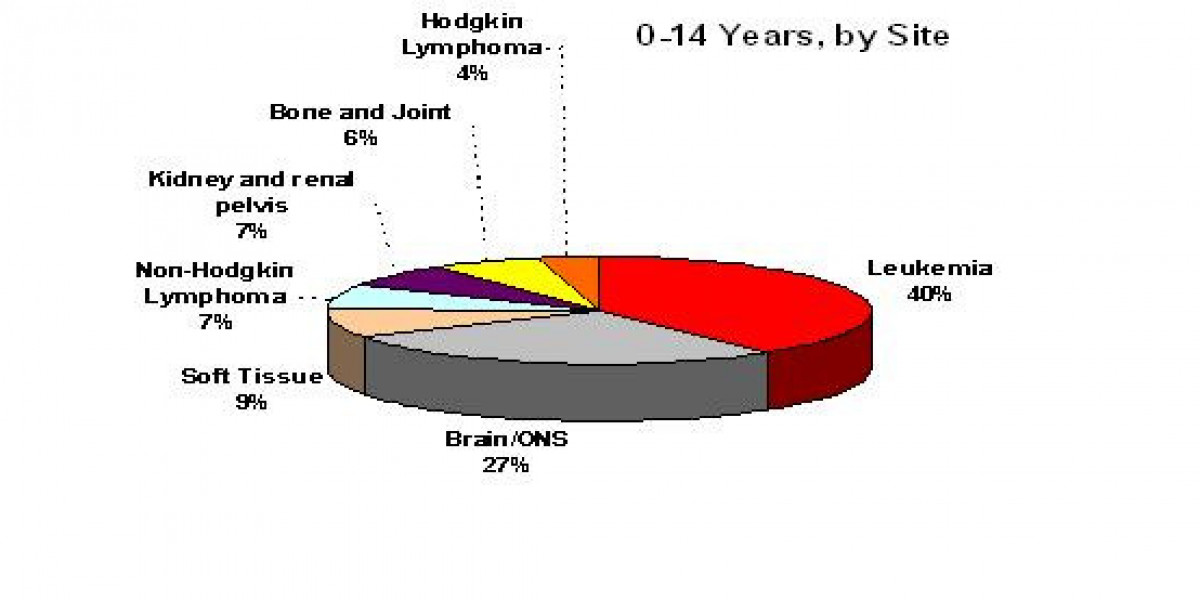
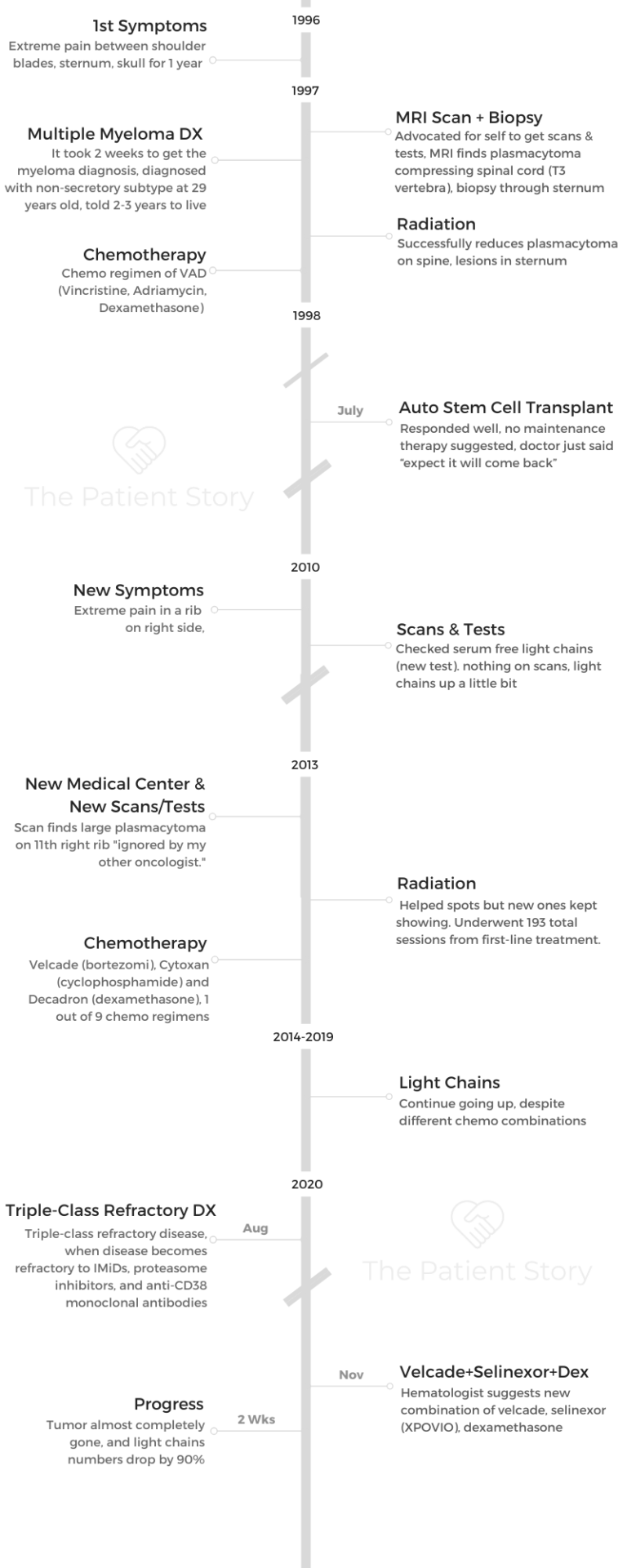
Beth was just 29 years old and the mother of 2 young kids when she was diagnosed with multiple myeloma. She describes how she got through first-line treatment of radiation, chemotherapy and a successful stem cell transplant.
For 12 years, Beth lived her life with no sign of myeloma. When her pain returned, she didn’t think much of it after a doctor concluded it was unrelated to the myeloma. But just a couple years later, an oncologist said the myeloma was back — the cancer had relapsed.
Beth dives into her over-2-decades-long myeloma experience, including how the myeloma became triple-refractory (it didn’t respond anymore to the usual drugs), the new drugs that worked and didn’t work, and how she has managed to live her fullest life with the disease.
Explore her incredible 5-part story series below. Thank you so much for sharing, Beth!
- Name: Beth Ayen
- Diagnosis (DX)
- Multiple myeloma
- Relapsed/refractory multiple myeloma
- 1st Diagnosis:
- Age: 29 years old
- Symptoms: Extreme pain between shoulder blades, sternum, head for 1 year
- Burning sensation that radiated out
- Tests for DX:
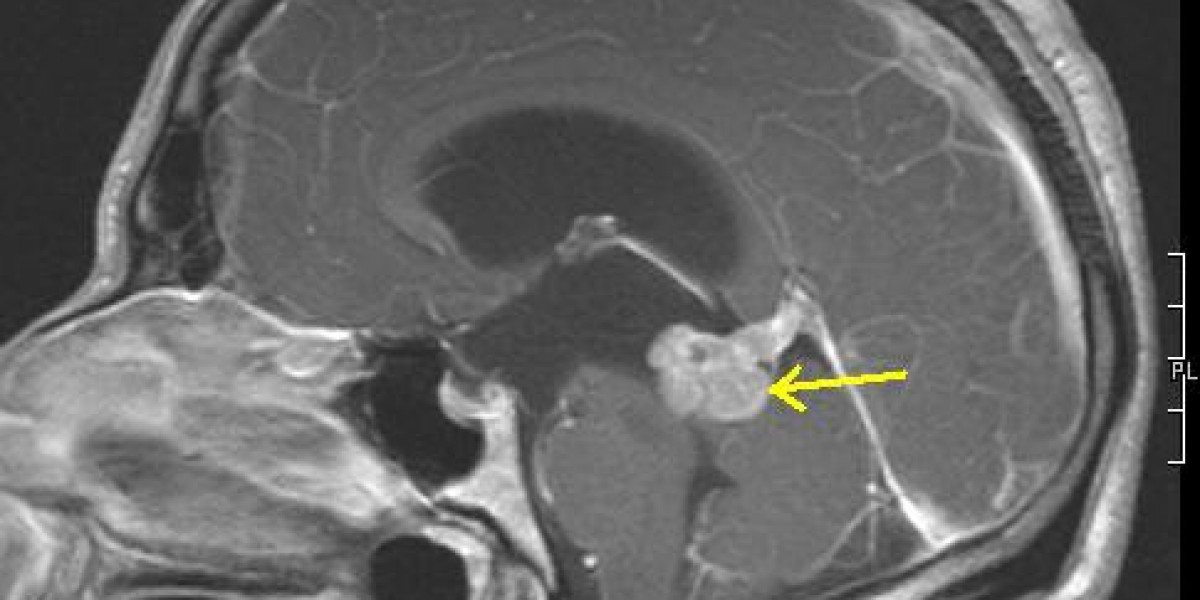
- MRI found a plasmacytoma compressing spinal cord
- Treatment
- Radiation therapy
- Chemotherapy
- VAD (Vincristine, Adriamycin, dexamethasone)
- Autologous stem cell transplant (SCT)
- Relapse:
- Age: 45 years old
- Symptoms:
- Extreme pain in ribs and head
- Light chain #s up
- Treatment:
- Radiation (193 sessions total over 7 years)
- Chemotherapy (9 regimens since beginning), mainly:
- Velcade (bortezomib), Cytoxan (cyclophosphamide) and Decadron (dexamethasone)
- Different drug combinations
- Elotuzumab (Empliciti)
- Belantamab mafodotin (Blenrep)
- Selinexor (Xpovio)+ bortezomib (Velcade) + dexamethasone
- VIDEO: Early Symptoms of Multiple Myeloma
- 1st Symptoms of Multiple Myeloma
- The Multiple Myeloma Diagnosis
- Processing the Diagnosis
- Getting your prognosis
- Dealing with the possibility of a “terminal” diagnosis
- How did you break the news of the myeloma diagnosis?
- What support was most helpful from other people during this time?
- How did you handle the cancer diagnosis with young children?
- A silver lining to the shifting household roles
- "Let people help you"
- VIDEO: Finding Treatment in a Small Town
- VIDEO: Multiple Myeloma Relapse
- VIDEO: Relapsed Refractory Multiple Myeloma Treatment
- CAR T-Cell Therapy
- Belantamab mafodotin (Blenrep)
- Selinexor (Xpovio) + Bortezomib (Velcade)+ Dexamethasone Combination (SVd)
- How did you learn of this treatment option?
- What was the status of your myeloma?
- Describe the selinexor + Velcade + dexamethasone (SVd) regimen
- Describe the selinexor, bortezomib and dexamethasone combination side effects
- What has helped you manage the side effects?
- What’s the real impact of finding a new treatment that finally works for you?
- VIDEO: Living Life with Multiple Myeloma
- Multiple Myeloma Stories
Thank you to Karyopharm for its support of our educational program. The Patient Story has full editorial control of our content. The interview has been edited only for clarity.
This is not medical advice. Please consult with your healthcare provider for treatment decisions.
VIDEO: Early Symptoms of Multiple Myeloma

1st Symptoms of Multiple Myeloma
Introduction: Tell us about yourself
I live in Casper, Wyoming, and my husband is an engineer. He works for the highway department. I have 2 children. My daughter, Becca, lives in Colorado Springs, and she has 2 kids. I have 2 grandkids, and their names are Isaac and Piper.
They’re really fun, and I’m really excited that I got to see grandchildren in my life. It’s so exciting. I have a son and daughter-in-law, who live in Houghton, Michigan. They are pregnant. They’re going to have a baby in September, so that’s really exciting!
They’re far away. Hopefully, we’ll get to know our little baby pretty well. I’m a retired third-grade teacher. I worked as a teacher for about 8 years.
Then just with health issues and the myeloma, I’ve just decided that I needed to retire and take some time off and focus on my health.
Other than that, we love to travel Wyoming and visit all the incredible places that there are here. I love to crochet, and I love to read. I’ve been having trouble with my vision. When I can, I love to read. We love to go see movies and those kinds of things, so that’s what we do.

What finally got you to go to the doctor’s office?
It was just becoming so consistent. It had started between my shoulder blades, and then the same kind of pain was happening in my sternum and in my skull.
It was like a burning pain. It started out as a pinpoint, and then it would radiate farther out, farther out, and then into the other bones. I just thought, “This is not right. This is not muscular pain.”
I saw several doctors in my little town that we were living in, Rock Springs, Wyoming. They would just say, “Oh, everybody has pain. Just do these exercises. Everybody has back pain.”
I finally just was talking to a lot of people and just sharing with them how I was in all this pain and someone said, “There’s an orthopedic surgeon in Salt Lake City who will see people without a referral.”
We decided to go ahead and go see him. He was able to do an MRI on my spine without a referral. That was really great. He was the one who found the issues that were happening in there.

How did you advocate for yourself as a patient?
I think part of it is you really have to remember that you know your body when other doctors are telling you these things, and you just know that it’s just not right.
My first bachelor’s degree is in exercise and sports science. I just knew that these exercises that they were giving me were not the right things to do. They were causing more pain.
I just thought this is not right. I’ve got to go somewhere where someone will actually take me seriously. Really, I’m one that never goes to the doctor for pain.
My doctors now are like, “You need to tell us when you are in pain.” I’m always way far along in the process because I wait so long. I knew that because of that personality trait, that there was something serious and that I was really feeling like I needed to see a doctor who could help me.
We just pushed and pushed and pushed and researched and looked and asked people.
I think that was an important thing for us to do, because I don’t know how long I would’ve gone. I would’ve had a lot more issues, I think, if we hadn’t gone then.
»MORE: How to be a self-advocate as a patient
When did you first think of cancer?
Beth went to a Salt Lake City doctor, who finally gave an MRI and found a plasmacytoma that was compressing her spinal cord where her T3 vertebra used to be.
What the doctor told me was, “We’re going to do a biopsy.” They decided to do a biopsy through my sternum because they didn’t want to do it through my spine. It was too dangerous. They did a biopsy through my sternum. This was the week before Thanksgiving in 1997. He told me, “Just wait. We’ll call you with the results of the biopsy.”

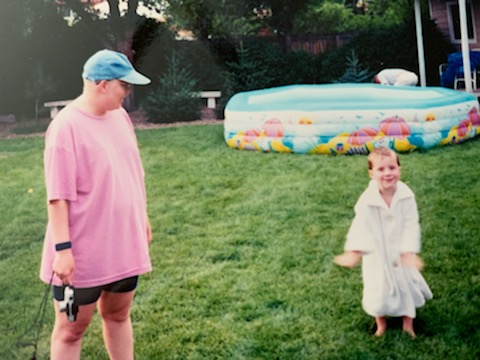
Of course, when you hear the word ‘biopsy,’ you think ‘cancer’ for sure. That was really difficult. I had 2 kids. I had a 5-year-old and a 3-year-old at the time, which made it really, really hard to think about the cancer diagnosis.
We lived 3 hours away from Salt Lake City. That’s how far Rock Springs is from Salt Lake. It just all made it very difficult. I went home, and I sat by the phone. I was cleaning my house. I was getting ready for Thanksgiving.
The Multiple Myeloma Diagnosis
Getting “The Call”
I was doing all the things that you do for that and just working and feeling pretty normal, except for the pain in those places. I got a call on Wednesday, the day before Thanksgiving, and it was the orthopedic surgeon.
He said, “I’m going to hang up this phone in about 2 minutes, and the phone’s going to ring. It’s going to be an oncologist, and she’s going to tell you what she needs you to do.”
I put the phone down. Literally, when I put the phone down, it rang. This was back when we had phones that hung up. Anyway, I picked up the phone, and it was this oncologist. She said, “Beth, you need to get to Salt Lake right now.”
I said, ‘Do you realize it’s 3 hours away? I have 2 small children that I need to figure out what to do with.’
She said, “I don’t care. You need to get here immediately. They’re going to hold the admissions office open for you because they’re waiting for you.”
I was like, “Okay, well, we’ll get there as soon as we can.”
We threw stuff in a suitcase. We dropped our kids off. We had lived in Evanston, Wyoming, for a while, so that’s on the way to Salt Lake. We dropped our kids off there with some friends, and then we drove the longest drive that we ever drove from Salt Lake City. It’s about an 80-mile drive. We just sat there and just did not talk.
We knew that now we’re seeing an oncologist. We knew this was cancer now, but we had no idea what this meant.

We showed up at the hospital. Of course, as soon as I walked into the admissions office, they’re like, “Are you Mrs. Ayen? Are you Mrs. Ayen?”
“Yes, I’m Mrs. Ayen.”
“Okay, we’re going to take you up to the oncology floor.” They took us up there. The nurse at the desk said, “Your room isn’t quite ready, so can you just sit in the waiting room for a minute?”
I said, “Sure.”
Then this doctor walked in a few minutes later, and she said to the nurse, “Well, where’s Mrs. Ayen?”
The nurse said, “Well, she’s right there.”
The doctor said, “No, that can’t be her.”
The nurse was like, “What do you mean?”
She’s like, “Because she shouldn’t be able to walk. She shouldn’t be moving.” She came over to me and she goes, “Can you walk?”
I said, “Oh yes, I’ve been cleaning my house. I’ve been making beds. I’ve been cooking turkeys.”
I said, “Yes, I’m doing fine,” and she said, “Oh, my goodness. Please don’t move an inch. We’re going to take you to your room. I want you to lay in bed, and you’re only allowed to get up to use the restroom.”
At that point, another oncologist came in and they told me that they suspected that I had multiple myeloma. They saw myeloma cells in my biopsy, and I had a plasmacytoma where my T3 vertebra used to be. It had eaten completely away, and it had completely compressed my spinal cord.
They were worried that any movement could cause complete paralysis. They wanted to do 10 days of radiation to get that tumor down so that my spinal cord would come back, and I wouldn’t be in such danger of severing that spinal cord with that plasmacytoma.

It took longer to diagnosis because I didn’t fit the “myeloma profile”
They were just really surprised, and they couldn’t believe it could be multiple myeloma, so it took a while for them to diagnose it because
I was only 29, I was a White female, and this is just very not typical of myeloma, especially in 1997.
They weren’t seeing that very often, and they actually had never seen it — at this hospital and several hospitals that I had been at — that young.
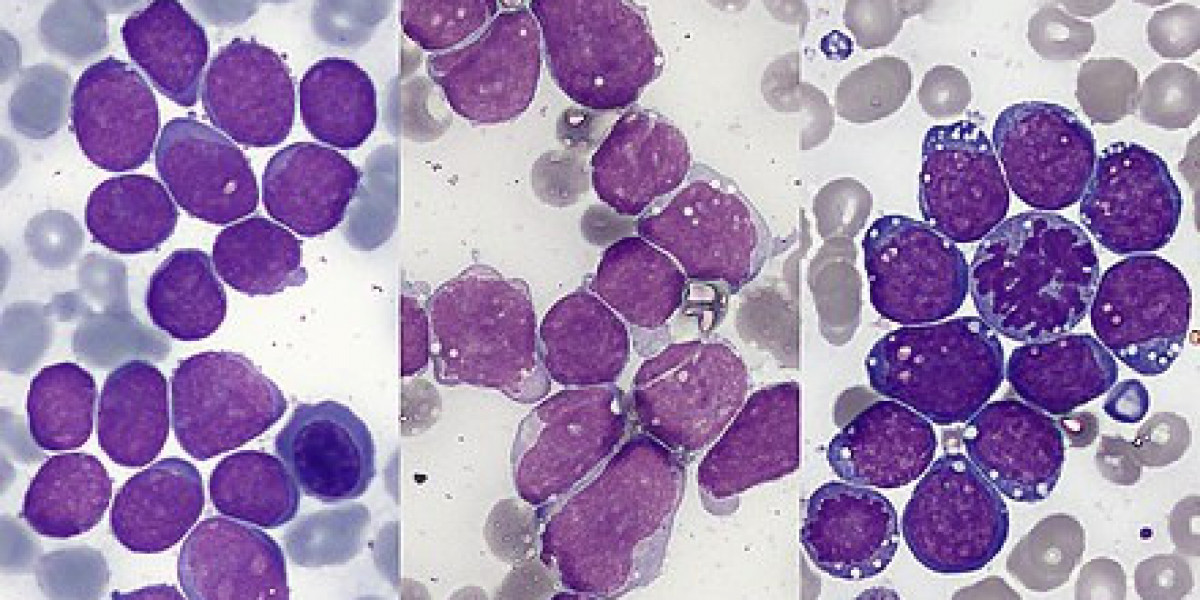
They took a while to diagnose it to make sure that they were correct, but they took it to the tumor board at University of Utah. The other thing about it was I didn’t show the M protein, which is very indicative then of myeloma, and so I didn’t show that. I was considered non-secretory, so that is a more rare side of the multiple myeloma, and it was more difficult to diagnose because of that.
How long were you in the hospital?
I was in the hospital for about 10 days. Actually, it was only about a week, and they did radiation every single day, trying to get that tumor down until it was safe for me to move around.
My parents live in Denver and were coming up to visit us for Thanksgiving, and so they just bypassed Rock Springs, picked up our kids in Evanston, and then came to us in Salt Lake City.
They stayed in a hotel for a little while while I stayed in the hospital, and then I had to stay in the hotel. My husband and I ended up staying in the hotel with them for a few days after because they let me go from the hospital, but I was still doing radiation for a few days. I had other appointments that they wanted to look at. They wanted to see what the ramifications of the tumor were going to be on my spine.
Processing the Diagnosis
Getting your prognosis
There’s just a quick story about the neurologist that I saw. He said, “Oh, there’s some things that we could do, but you’re not going to survive long enough to make it worth it.”
I know. It’s just crazy. I was like, “Oh, okay, well, I guess.”
The oncologist gave us a prognosis of 2 to 3 years at the time, and then this neurologist told us that. At that point, we were just feeling like, “This is a short-term thing, or I’m going to die from this. We got to figure out what to do with our life, with our kids. How’s Mark going to raise these kids by himself?”

Dealing with the possibility of a “terminal” diagnosis
It was really difficult, and it was difficult for me to have the kids there in some ways while we were in the hospital. I loved having them there for sure.
I felt like we were all together as part of a family, but I also was dealing with so many emotions that I didn’t want to burden them with my dealing with that I have cancer and it’s terminal. I’m probably not going to live very long with it.
That was really difficult. I think my daughter still struggles with some of that because she was five. She remembers some of it. My son doesn’t have any recollection of any of that happening, but I can remember them coming in, sitting on my bed, playing with the up and down buttons on the bed, different things like that, but there were some difficult parts of that.
I was glad to have them there because a mom wants their kids by her side. At the same time, it was hard on them, and I wish they didn’t have to go through it.
How did you break the news of the myeloma diagnosis?
I remember sitting in the hospital and Mark, my husband, calling a lot of people and telling them what was going on. We’re churchgoers, and we have a lot of close church family. In Evanston and in Rock Springs, we had that.
»MORE: Breaking the news of a diagnosis to loved ones
What support was most helpful from other people during this time?
There were a lot of people who wanted to support us. They came and visited. When we got home, they brought meals and cleaned our house. They did so many things for us, which was just amazing.
They took care of our kids. They would take them on trips. If they were going to the store, they’d come and pick them up. If they were going to McDonald’s, they’d come and get them or whatever. That was really helpful.

How did you handle the cancer diagnosis with young children?
I think the way that we just dealt with the kids was just that, “Mommy is sick, and she’s going to have to do some medication.” They were too young to really understand.
We use the word “cancer,” but they didn’t understand what that meant and the ramifications of that until later on in their life. They just basically have lived with it their whole lives pretty much.
I can remember when I lost my hair the first time, my daughter did not want to see me with a bald head. I always wore a hat or a scarf or something. I didn’t wear wigs too much.
I just didn’t have access to good wigs at that time, with where we lived and the cost of them. They have such better resources now.
Anyway, my son loved it. He would take my hat off. He would rub my head. He just thought it was so cool that I was bald. That was a difficult thing to manage because I didn’t want to upset my daughter.
At the same time, I couldn’t stop my 3-year-old from that. We just lived that life. I was homeschooling my daughter in kindergarten at the time, which is crazy.
I was doing the first line of treatment, the VAD, which was vincristine, Adriamycin, and dexamethasone. They would hook me up in Salt Lake with a pump with this fluorescent pink medication in it that had “biohazard” written all over it, and I’m thinking they’re pumping this right into my veins.
They would hook me up in Salt Lake. I would go home for 4 days, and then a home healthcare nurse would come into the house and take care of it.
My kids were around this all the time, and I had very difficult veins. The poor nurses would just struggle and struggle. My kids would be walking around while they’re doing all of this.
Sometimes, I think maybe I would try to expose them less to less of that if I had to do it over again, but I didn’t know what I was doing. This was all new to us. I was just trying to survive the day and do what they told me to do.
It was a difficult treatment. It was very hard on the body, and it was really the only treatment at that time — that was widespread, anyway. Luckily, my husband worked really close to the house and had a very flexible job. If he needed to come home while I was feeling sick or whatever, he was able to do that and take care of the kids.
A silver lining to the shifting household roles
One thing, I guess, is that it developed a really close relationship between their dad and them because he was their caregiver in a lot of situations where, normally, I would have been.
My mom would come for about a week during that time when I was doing the VAD treatment. Then the next time, the next month, my mother-in-law would come, and they would just switch back and forth and help with the kids.

“Let people help you”
I think the thing that I would tell other people is to accept help. Let people help you, and ask for help if you need to. I know it’s so hard. I want to do everything on my own and just do it.
Sometimes if you need help, it’s okay to ask.
VIDEO: Finding Treatment in a Small Town
Rural Cancer Care Experience
Beth underwent radiation therapy to decrease the lesions and the plasmacytoma on her spine. She then had the chemo, the VAD, which did not reduce the lesions. The following year, Beth went through an autologous stem cell transplant and responded well.
How did you manage getting treatment in such a rural area?
Because we lived in such a small town of Wyoming — and really in Wyoming, they don’t do stem cell transplants anywhere — we had to go to Denver, which is where my parents lived. That worked out really well.
They wanted us to go to Salt Lake City because that’s where my original oncologist was, but it worked out better in Denver because my parents were there. They could watch the kids.
The need for more support
We knew it was going to be most of the summer of 1998. My husband had just gotten a job. We had just moved recently from Evanston to Rock Springs. He was new to his position.
They made it so nice for him. They donated sick leave. All over the state, they donated sick leaves. He was able to come and be with me during the entire transplant, which was 30 days in the hospital.
Autologous Stem Cell Transplant

Describe going through the stem cell transplant process
We went to the University of Colorado, and that’s where I had my stem cell transplant. They had no problem getting enough cells for that.
It was a really, really hard time. Basically, they kill your bone marrow until it’s basically nothing so that they can restart it.