Table of contents:
Coping with chronic lymphocytic leukemia (CLL) can be a challenging and deeply emotional experience—both for the person diagnosed and for the friends or family members providing support. Recognizing how CLL progresses and understanding the symptoms that may appear as the disease advances can offer a sense of preparedness. At the same time, learning about available treatments, diagnostic procedures, and avenues for support can bring hope and a clearer path forward.
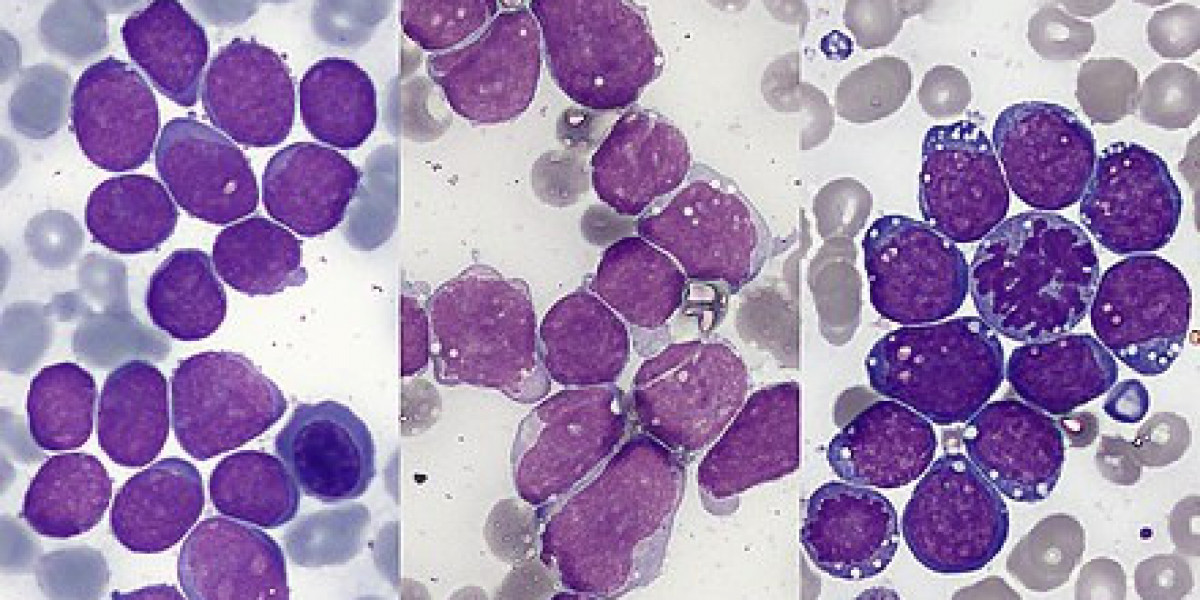
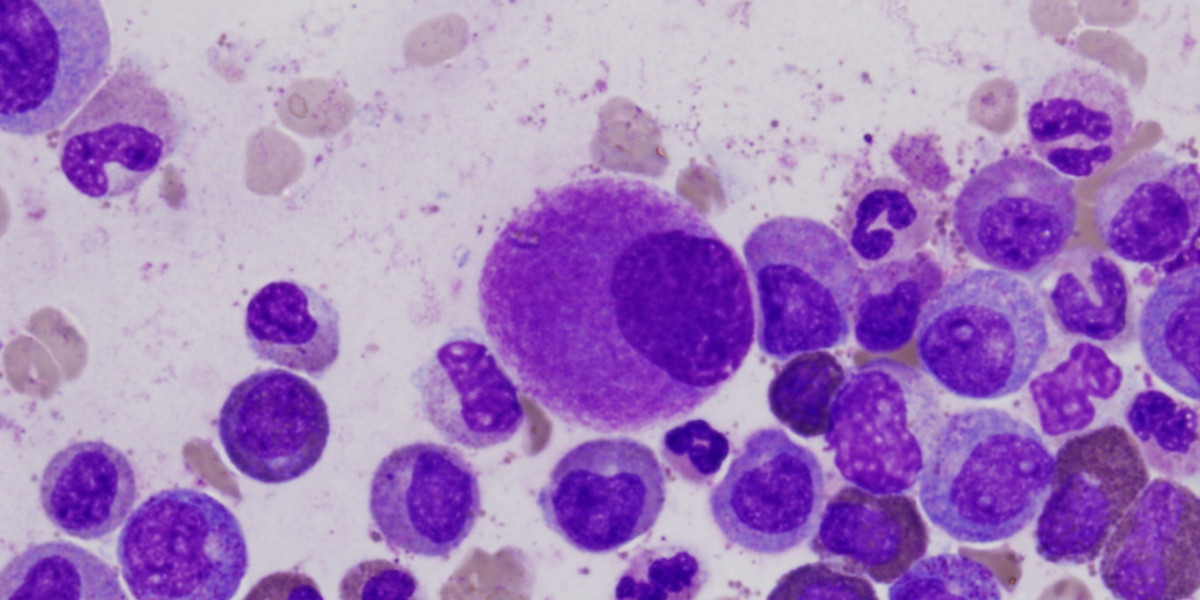
Chronic lymphocytic leukemia ( CLL ) is a type of leukemia affecting white blood cells known as lymphocytes, which are crucial to the immune system, fighting off infections and diseases. In CLL, a genetic mutation occurs in a single lymphocyte, causing it to behave abnormally. Instead of maturing and functioning normally, the mutated cell begins to multiply uncontrollably, producing large numbers of abnormal lymphocytes. Over time, these cells accumulate in the blood and bone marrow, crowding out healthy cells and weakening the body’s ability to fight infections.
Unlike acute leukemias, which progress rapidly, CLL usually unfolds more slowly. Some people may not notice any problems at first and can feel reasonably well for years before requiring active treatment. For others, the disease can take a more active course (Eichhorst et al. 2020).
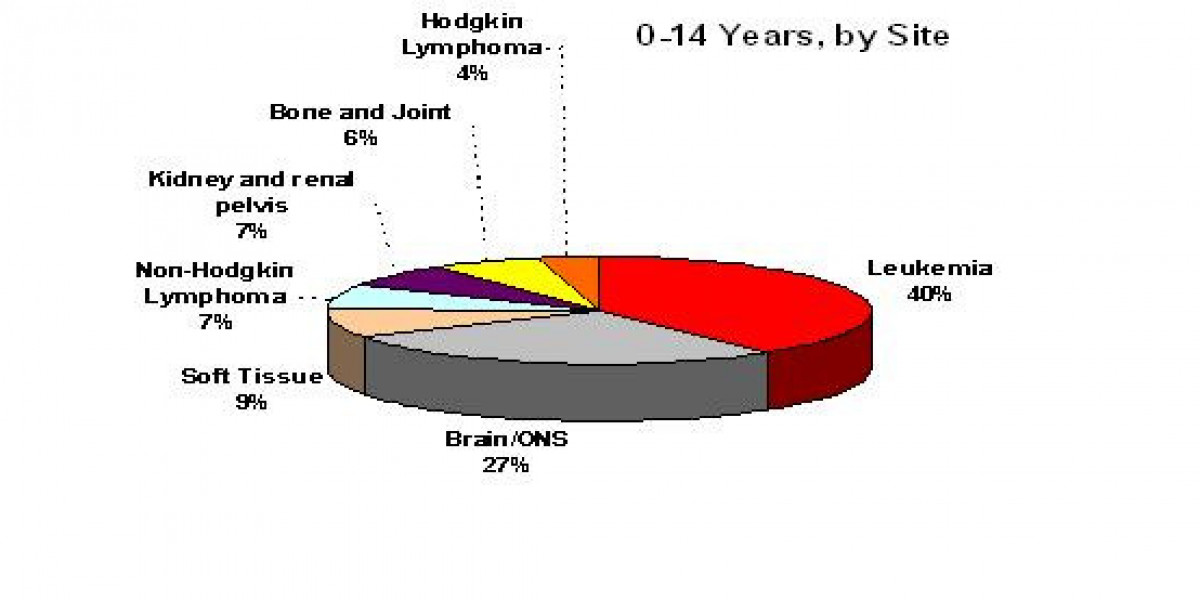
Researchers and healthcare professionals have long used specific systems to define CLL progression so they can better determine treatment strategies. The Rai system, popular in the United States, classifies CLL into five risk categories (Rai 0 through IV) based on factors like lymph node enlargement, spleen size, and whether anemia or low platelet counts are present. Lower stages typically involve fewer symptoms and are considered lower risk, while higher stages may indicate more significant blood cell count issues and greater disease burden (Rai et al. 1975).
Meanwhile, the Binet system, commonly used in Europe, divides CLL into stages A, B, and C. This classification hinges on the number of areas with enlarged lymphoid tissue (for example, lymph nodes or the spleen) and whether the patient exhibits anemia or low platelet counts. Stage A usually involves up to three areas of lymphoid enlargement with no anemia or low platelets; Stage B indicates more than three areas of enlargement; and Stage C includes anemia or low platelet counts (Binet et al. 1981). In 2016, experts introduced a new tool called the CLL International Prognostic Index (CLL-IPI). This model considers various biological and clinical factors—such as genetic changes in leukemia cells, certain gene mutations, and overall patient health—to better predict how the disease might progress (Molica et al. 2016).
One unique aspect of CLL is that it’s often discovered accidentally. Many individuals are diagnosed after a routine blood test for an unrelated issue reveals an elevated lymphocyte count. In earlier stages, people might notice few or no symptoms of illness. As CLL progresses, however, common symptoms can include:
For those in advanced stages of CLL or nearing the end of life, additional symptoms may appear. These can include:
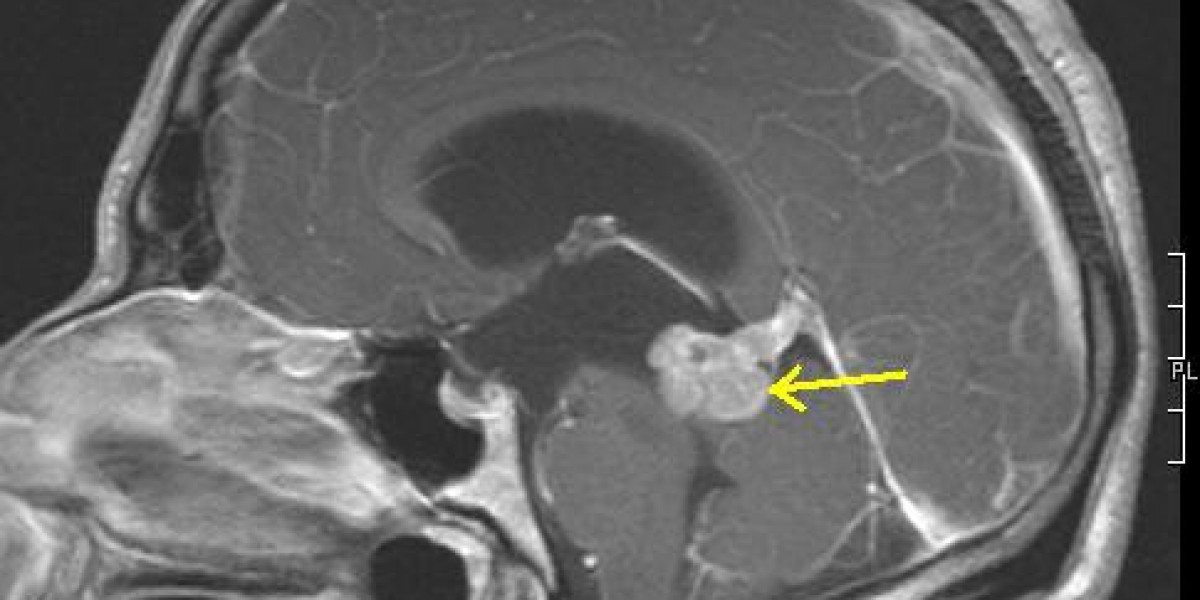
Before a treatment plan is decided, doctors conduct comprehensive evaluations to diagnose CLL . These can involve:
Treatments for CLL depend on the stage of the disease, overall health, and a patient’s specific risk factors. A few primary approaches include:
People with CLL can have widely different experiences due to a number of factors, both prognostic (overall outcome) and predictive (effects from specific treatments). These include:
The Leukemia & Lymphoma Society (LLS) supports people affected by blood cancers through research funding, patient services, and advocacy.
Your generosity powers LLS’s mission . Every donation helps drive forward new discoveries and brings us closer to a future without blood cancer.
Living with CLL or caring for someone who has it can evoke worry and a desire for reliable information. Understanding how CLL is staged, learning to recognize symptoms, and exploring different treatment pathways can lessen uncertainty. With developments like the CLL-IPI bringing precision to diagnosis and treatment and ongoing research propelled by organizations such as LLS, there is a growing network of care and expertise to lean on.
About the author: Dr. Ali is a medical journalist and copywriter.
Eichhorst, B., T. Robak, E. Montserrat, P. Ghia, C.U. Niemann, A.P. Kater, M. Gregor, et al. 2020. “Chronic Lymphocytic Leukaemia: ESMO Clinical Practice Guidelines for Diagnosis, Treatment and Follow-up.” Annals of Oncology 32 (1): 23–33. https://doi.org/10.1016/j.annonc.2020.09.019 .
Rai, K. R., A. Sawitsky, E. P. Cronkite, A. D. Chanana, R. N. Levy, and B. S. Pasternack. 1975. “Clinical Staging of Chronic Lymphocytic Leukemia.” Blood 46 (2): 219–34. https://doi.org/10.1182/blood.v46.2.219.219 .
Binet, J. L., A. Auquier, G. Dighiero, C. Chastang, H. Piguet, J. Goasguen, G. Vaugier, et al. 1981. “A New Prognostic Classification of Chronic Lymphocytic Leukemia Derived From a Multivariate Survival Analysis.” Cancer 48 (1): 198–206. https://doi.org/10.1002/1097-0142(19810701)48:1 .
Molica, Stefano, Tait D. Shanafelt, Diana Giannarelli, Massimo Gentile, Rosanna Mirabelli, Giovanna Cutrona, Luciano Levato, et al. 2016. “The Chronic Lymphocytic Leukemia International Prognostic Index Predicts Time to First Treatment in Early CLL: Independent Validation in a Prospective Cohort of Early Stage Patients.” American Journal of Hematology 91 (11): 1090–95. https://doi.org/10.1002/ajh.24493 .
Originally published on LLS Blog.