Blogs > I was an oncology nurse practitioner, and then I got breast cancer
At 39, I went from caring for breast cancer patients to becoming one
My name is Karen Powell. I’m a mom to four amazing children including a nine-year-old son, eight-year-old twin boys and a three-year-old daughter. I'm also an oncology nurse practitioner and menopause specialist. Most recently, I became a breast cancer thriver at 39.
My family and I live in Monmouth County, New Jersey. We moved when our rapidly growing family outgrew our small Manhattan apartment. In the years that followed, I spent the better part of my thirties acquiring fine lines and enormous blessings. I was raising my spirited children while working as a breast-certified oncology nurse practitioner, specializing in plastics and reconstruction and working at a startup menopause clinic.
On a balmy Tuesday evening in late July, I settled into the comfort of my bed. My husband was away on a business trip, and I had finished kissing all of my children goodnight, right on the tops of their sun-kissed noses after a busy evening. I was clicking through multiple tabs on my laptop, planning carpools and ordering groceries, when I casually brushed my hand against a lump I hadn’t been looking for.
From there, my attention shifted to myself, I felt every aspect of my breasts from every angle. Leading up to this point, I knew my girls very well. Between breast feeding, self-breast exams and boob scoops, I immediately knew this lump – though smaller than a pea – was new, firm and irregular.
I felt the ground falling from underneath me. The thought of switching roles from a cancer provider to a cancer patient hit me like a wave. My mind raced from denial to anger. This can’t be happening to me. Hadn’t I made all the right choices? What had I missed? I took a microscope to my life, scrutinizing any and every possible lifestyle choice that led me to this instant.
Then fear grew a gnawing feeling in the very pit of my stomach. Am I going to die? Will I leave my young children without a mother?
As I lay there alone, in my room, my racing thoughts were louder than the sound of crickets outside my window. After several sleepless hours, I told myself the same advice I use to calm my patients: We don't know until we know. And we cannot control the uncontrollable.
The following day, I nervously went to the facility where I work to get my very first mammogram. Familiarity with the exam and the institution, though, didn’t make it any easier. My palms were sweaty. I was afraid that my own self-assessment suspicion would be proven correct. Oh, how I never wanted to be more wrong.
While waiting for my scan, I realized it was exactly 14 years to the day since I had begun my first day of work as a breast surgery nurse. I had built my career there, spending so much of my time helping people through this very process. Now I was the one sitting in the waiting room.
I trusted my colleagues and today would be no exception. During the scan, I reviewed the images with the radiologist, who I’ve known professionally for several years. She said, “I know you know what this is, but we still need to get a biopsy.”
Hearing those words from the other side of the exam table was surreal. I so eagerly wanted to know exactly what this lump was, but on the other hand, I desperately wanted to wake up from this real-life nightmare that felt like there was no end in sight. I then thought to myself, how many women my age would have dismissed this lump and went about their busy lives? The lump was hard, but very small and still very mobile.
A few days later, while in clinic, caring for people on their breast cancer journey, the official diagnosis came. The report came through my patient portal. Wearing my lab coat, professionally dressed, my curiosity got the best of me. I had to know.
I opened my chart, my heart racing. I took a deep breath as if I were about to go underwater, and read and reread the words: Invasive ductal carcinoma of no special type.
I read it over and over and over again. The words were familiar. They were clinical, diagnostic words I read often, but now they had my name attached. Even with all my experience, nothing prepares you for the moment you find out you have cancer, when your life spirals, priorities shift, plans change, and in an instant, your whole world is turned upside down. Mentally, I felt completely disconnected from my body as I began processing my new diagnosis I lingered in that disconnection for the duration of the day, I now realize that was the exact survival technique necessary to remain focused on my patients who were behind those exam room doors – oncology professionals often compartmentalize or disassociate in order to stay mentally grounded. In this circumstance, before seeing my next patient, it was the most necessary coping mechanism I could conjure up. I had a patient waiting, so I closed the app, straightened my lab coat, and moved forward.
There are no guidelines on how to be an oncology patient.
August 2024 will go down as the most difficult, polarizing month of my life.
I was navigating the anxiety of knowing I had cancer growing inside me, while also figuring out childcare during my appointments (without the luxury of nearby family) which filled me with angst. One minute I was creating a surgical plan with my breast oncologist; the next, I was creating a meal plan for the week ahead. I was weighing reconstruction options after a bilateral mastectomy while deciding on new school bags to buy for the first day of school.
Everything felt split in two.
Waiting for the surgical date dragged on forever. Even the stillness of waiting at red lights felt unbearable.
Through it all, I carried the mental weight of not knowing: those lingering questions about the stage and extent of disease that only a final pathology report could answer.
There was a gaping disconnect between what was happening inside my body and the outside world, between the diagnosis I was carrying, and the lazy, blissful beach days that filled our late summer weekends.
At the same time, I also had to stay present for my patients. But now, I understood their experiences in a way I never had. Their fear. Their grief. The isolation. The exhaustion. The loss of control. Now, I truly was aware of the unique challenges young people face when blindsided with a breast cancer diagnosis in the midst of building careers, growing and raising young families, all while coping with permanent body image changes. As painful as it was, I wanted to be the clinician they deserve.
My patients gave me something, too. Strength. Grace. The quiet hope that I could get through this and come out on the other side, and flourish again.
During my recovery, my village showed up. My close friends swooped in like a team of angels, feeding my children with homemade meals and driving them to their baseball and soccer games while I was under restrictions. Most importantly, they wiped my tears and listened when waves of emotion got the best of me.
My husband became my caregiver and emotional anchor. He took time off work to help with our children, managed the house, cared for me and our family. He rose to every challenge with unwavering strength.
From afar, family and friends sent handwritten letters, flowers, and texts. Those messages made a deep impact. They reminded me I had a lot of support.
Facing my mortality at 39 changed literally everything.
I give fewer shits about the small stuff now. I care more about being present, about saying what matters, about laughing at the chaos of motherhood instead of trying to control it.
I’ve gained a new kind of gratitude for soulful friendships, for brilliant colleagues, and for the power of a supportive community.
For my children.
For my extraordinary husband.
I was carried on the shoulders of so many.
Day by day, I’m picking up the pieces of my life. I’m learning to love my reconstructed breasts that replaced the ones my breastfed babies retired long before the cancer did. My scars are part of my story, a declaration of life.
Early detection and early screening saved me. And I want that for every woman.
Get to know your breasts from a place of empowerment, not fear. Trust your instincts, and speak up. Advocate for yourself.
Never forget: Navigating the unique challenges of a cancer diagnosis as a young woman can be particularly isolating. Know that through the fear and uncertainty, I am right here with you, and we will never walk alone.
There are no guidelines on how to be an oncology patient.
DISCLAIMER:
The views and opinions of our bloggers represent the views and opinions of the bloggers alone and not those of Living Beyond Breast Cancer. Also understand that Living Beyond Breast Cancer does not medically review any information or content contained on, or distributed through, its blog and therefore does not endorse the accuracy or reliability of any such information or content. Through our blog, we merely seek to give individuals creative freedom to tell their stories. It is not a substitute for professional counseling or medical advice.
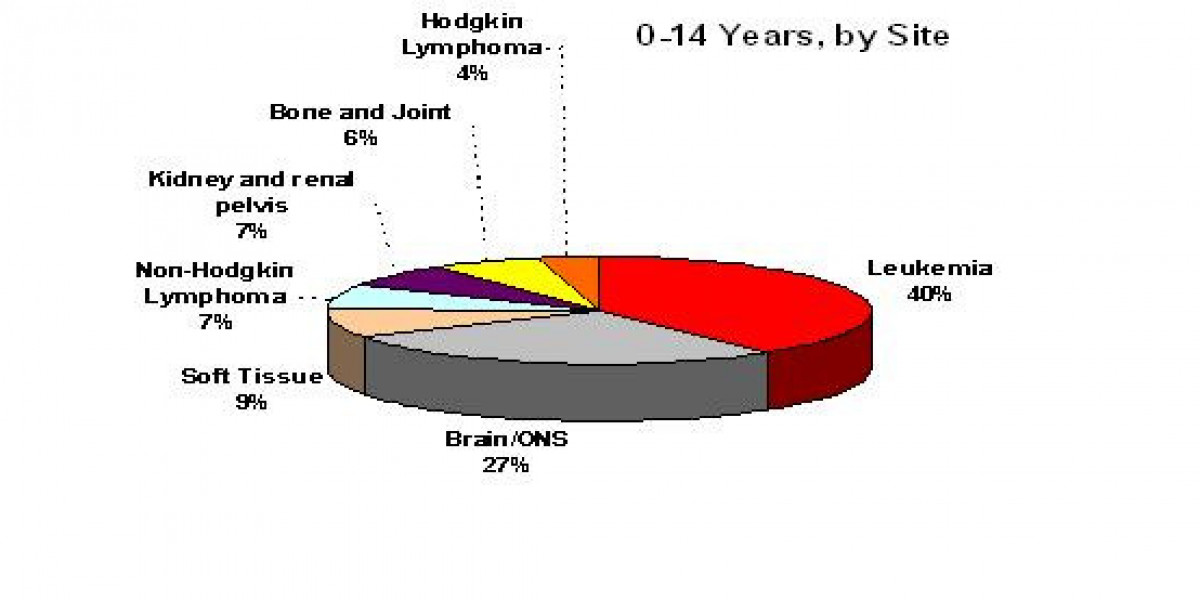
Breast cancer statistics
Discover statistics to answer some of the most common questions and to present a general picture of what breast cancer in the U.S. looks like today.
Young with breast cancer
If you are diagnosed with breast cancer before the age of 45, your medical and emotional concerns may be very different than those who are diagnosed when they are older.
Genetic counseling
Genetic counseling is the process of meeting with a genetic counselor to discuss your family health history and whether genetic testing is right for you. A genetic counselor is a healthcare provider.
Early menopause
If you are premenopausal or perimenopausal, breast cancer treatments may cause your menstrual periods to stop for a while or, in some cases, permanently.
Ovarian suppression
Ovarian suppression is surgery, radiation therapy or medicine that is used in premenopausal women to stop the ovaries from working.
Gonadotropin-releasing hormone (GnRH) agonists
The gonadotropin releasing hormone agonists, or GnRH agonists, are a class of injectable medicines offered to pre- and perimenopausal women with breast cancer in order to temporarily suppress, or slow, ovarian function.
Making decisions about protecting your fertility
You might not be thinking about having a family at the time of your diagnosis, but that’s the best time to talk with your partner, family, and healthcare team about future fertility.
Protecting your fertility during treatment
If you are premenopausal (still having menstrual periods), breast cancer treatments such as chemotherapy and hormonal therapy can affect your fertility. This may make it harder to become pregnant after treatment ends.
Birth control & breast cancer
If you were not in menopause before your breast cancer diagnosis and you are sexually active, it’s important to discuss birth control, or contraception, with your doctor.
Am I in menopause
Women affected by breast cancer may be premenopausal or perimenopausal before diagnosis. Learn more about early menopause, and other ways that you may be affected.
We'll send support straight to your inbox.
Tagged:
Living Beyond Breast Cancer is a national nonprofit organization that seeks to create a world that understands there is more than one way to have breast cancer. To fulfill its mission of providing trusted information and a community of support to those impacted by the disease, Living Beyond Breast Cancer offers on-demand emotional, practical, and evidence-based content. For over 30 years, the organization has remained committed to creating a culture of acceptance — where sharing the diversity of the lived experience of breast cancer fosters self-advocacy and hope. For more information, learn more about our programs and services.
Living Beyond Breast Cancer
40 Monument Road, Suite 104
Bala Cynwyd, PA 19004
©2025 Living Beyond Breast Cancer
Originally published on LBBC.