Tatijane’s Acute Lymphoblastic Leukemia (ALL) Story
Symptoms: Bone pain in ribs, trouble breathing, fast heart rate, painful lymph nodes in the neck, lump in between breasts
Treatments: Chemotherapy, double CAR T-cell therapy (clinical trial), bone marrow transplant

Tatijane’s Acute Lymphoblastic Leukemia (ALL) Story

Tatijane first knew something was wrong when she started having pain near her ribs. Her pain became so severe she was rushed to the ER and was then diagnosed with acute lymphoblastic leukemia, both B and T cells, with mutations. At 24, she was then given 6 to 8 weeks to live.
She shares how she processed her shocking diagnosis, the different treatments she’s undergone including a double CAR T-cell therapy clinical trial, and how she’s giving back to the cancer community.
She voices how she coped with three cancer recurrences, the emotional toll her diagnosis has taken on her, and how she found support.
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
- Name: Tatijane W.
- Diagnosis:
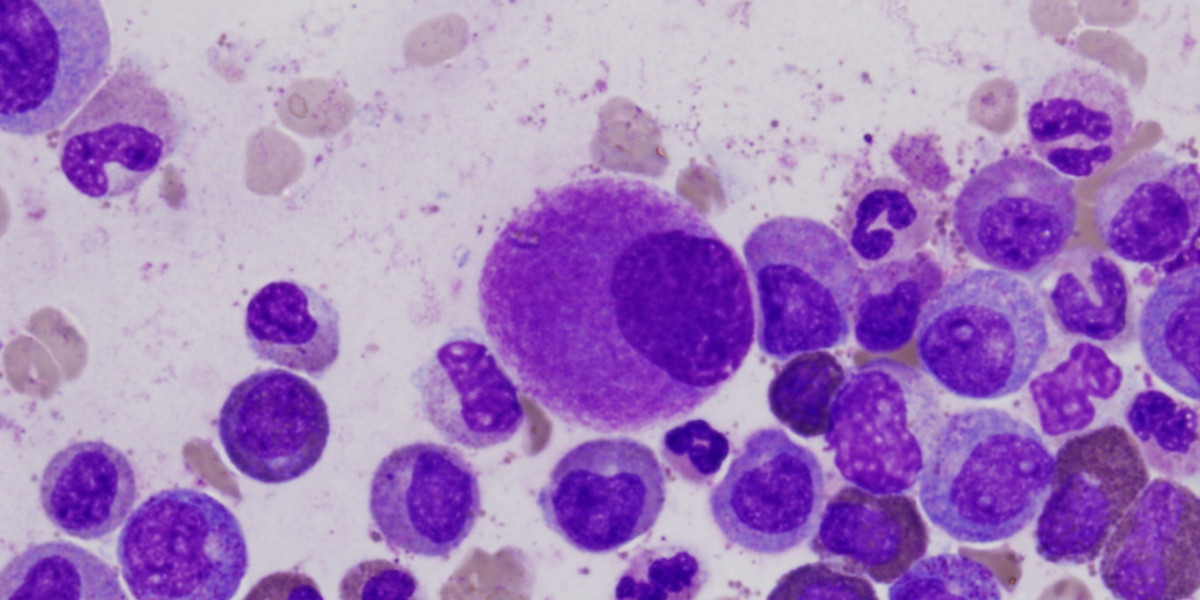
- Acute lymphoblastic leukemia (ALL), B and T cells, with mutations
- Symptoms:
- Bone pain in ribs
- Trouble breathing
- Fast heart rate
- Painful lymph nodes in the neck
- Lump in between breasts
- Treatments:
- Chemotherapy
- Radiation
- Double CAR T-cell therapy (clinical trial)
- Bone marrow transplant
Even now, I still feel like death is just sitting there in the corner, waiting and watching me. I’m not a curable patient and, at some point, they say that this cancer is going to take me. But I also am pretty tough and I’m a fighter so we’ll see what happens.

Introduction
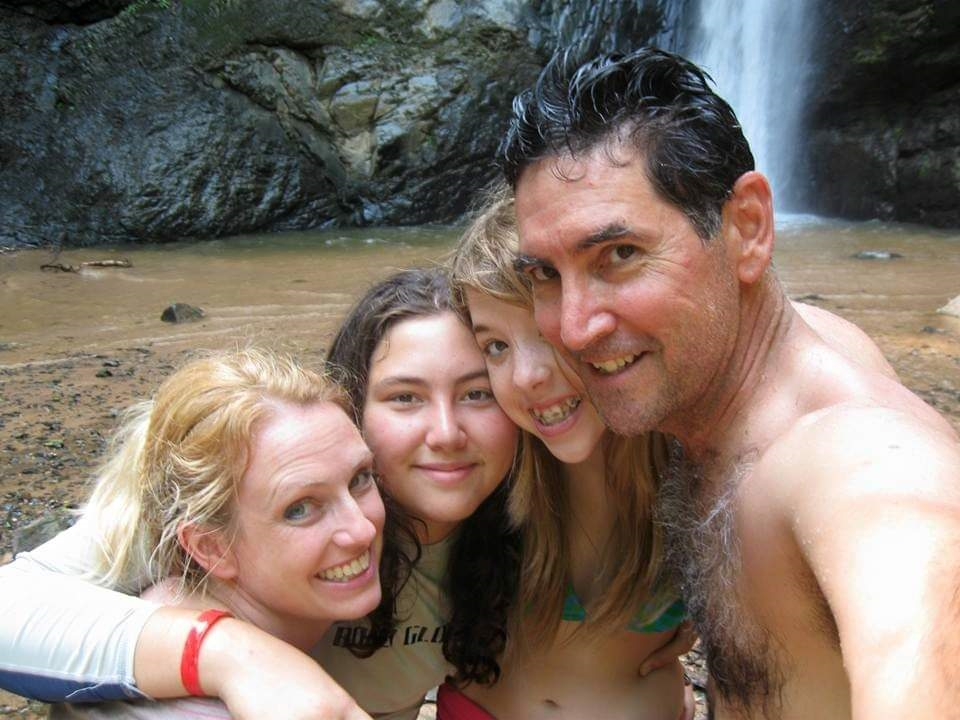
I’m an artist. I do photography, I like to draw [and] paint, [and] I did glass art for a while. I specialized in sandblasting, but I did do some stained glass.
I love music, watching TV, [and] movies. I love crafting and knitting. I like to stay very busy with artsy, crafty things.
I love mermaids. I have a mermaid tail that I actually swim in. My whole house is mermaid-themed.
I love being with my family and friends.






Pre-diagnosis
Initial symptoms
The January before I was diagnosed, I was starting to have bone pain in my ribs. I developed this mass in between my breasts. I started to get what I thought were tight muscles or little knots in my back. It was very painful, but I just kept getting massages from my family to try and get that.
I stopped eating so much because it was hard to eat. I was having issues breathing, but I was also overweight. I was 306 pounds so I thought maybe all of this had to do with being overweight. When I went to the doctors for all these issues, they said, “Lose weight and it will help.”
Then it was, “You have PCOS (polycystic ovary syndrome) so maybe that has something to do with it,” or “You have insulin resistance; that could have something to do with it,” or I also had other hormone imbalances, maybe that has something to do with it. It always came back to lose weight and it’ll go away.
On February 17th, my best friend stayed the night at my house. Then [on] the 18th, I went into the ER because I was in so much pain [that] I couldn’t handle it. I was diagnosed [on] the 19th. It all happened very fast.
Feeling like there was something more there
I didn’t think they were doing enough tests. I thought there was something else because none of it made sense. [What] does this have to do with being overweight? It was very frustrating, but it felt like I couldn’t really get any other resolutions from this.
I was messaging my doctor on the 18th, saying, “I can’t handle this pain anymore. What can I do?” He said, “Just go to the ER. It is a cyst that needs to be drained.” Nope, that’s not what it was.
Being in the ER that night was very traumatic because it was during COVID. I was in the ER by myself. They started running these mandatory ER tests.
They did a scan and saw the masses. The mass on my chest was so large, it was as if I was wearing a sports bra. It ended up collapsing my right lung and it was surrounding my heart and crushing it.
When I was diagnosed, they gave me six to eight weeks to live. I was alone in the ER getting diagnosed with that. It was so crazy.




The doctor had to come in and said, ‘I’m really sorry to tell you this, but you have cancer and it’s throughout your whole body. You would have 6 to 8 weeks to live.’

Getting the official diagnosis
My mom was sitting in the parking lot. Then maybe 10 minutes before they came in to tell me my diagnosis, I said, “Just go home,” ’cause it was already one in the morning. “I’ll call you when it’s time for me to come home.”
By the time she got home, I was calling the house phone. The doctor had to come in and said, “I’m really sorry to tell you this, but you have cancer and it’s throughout your whole body. You would have 6 to 8 weeks to live.”
Originally, they said it was non-Hodgkin’s lymphoma. It was very sad and very scary to hear. I remember trying to keep my composure. I was like, “Okay. How do we resolve this? How did this happen?” He was telling me it could be environmental, it could be genetic, all this stuff.
I remember just crying and going, “Did I do something wrong? Did I cause this on myself?” It was the weirdest. Went from mature, “Okay, how can we do this?” to then just crying.
There was no history of cancer in my family and there still isn’t [on] either side. It had to have been environmental. My family and I think we know what caused my cancer.
For it to be you weren’t listening to me and it was something this serious, that was very frustrating because it was like, ‘Could this have been caught sooner?’
Possible environmental cause
I believe my cancer had come from medication for my insulin resistance called metformin. There is a lawsuit against them. It turns out that the factory that they were getting the metformin from in India had jet fuel or something that ended up being exposed to the medication.
There have been many cases of many different kinds of cancers that developed after taking this medication. I was in the right time frame for that to be a possibility for me.
I strongly believe that is what caused my cancer [and] so does my family. It makes me sad because it was something that was supposed to help me and ended up hurting me worse than anything.
But also, if it didn’t happen, then none of this other great stuff would have happened. It’s a positive, but also a negative. I don’t want anyone else to be put into this situation.
Not getting answers when you know something’s wrong
It was frustrating. My whole life, if anything was wrong with me, the answer I always got was, “You need to lose weight.” I was used to it.
I’m used to doctors not listening to me. But then for it to be you weren’t listening to me and it was something this serious, that was very frustrating. Could this have been caught sooner?




Official diagnosis
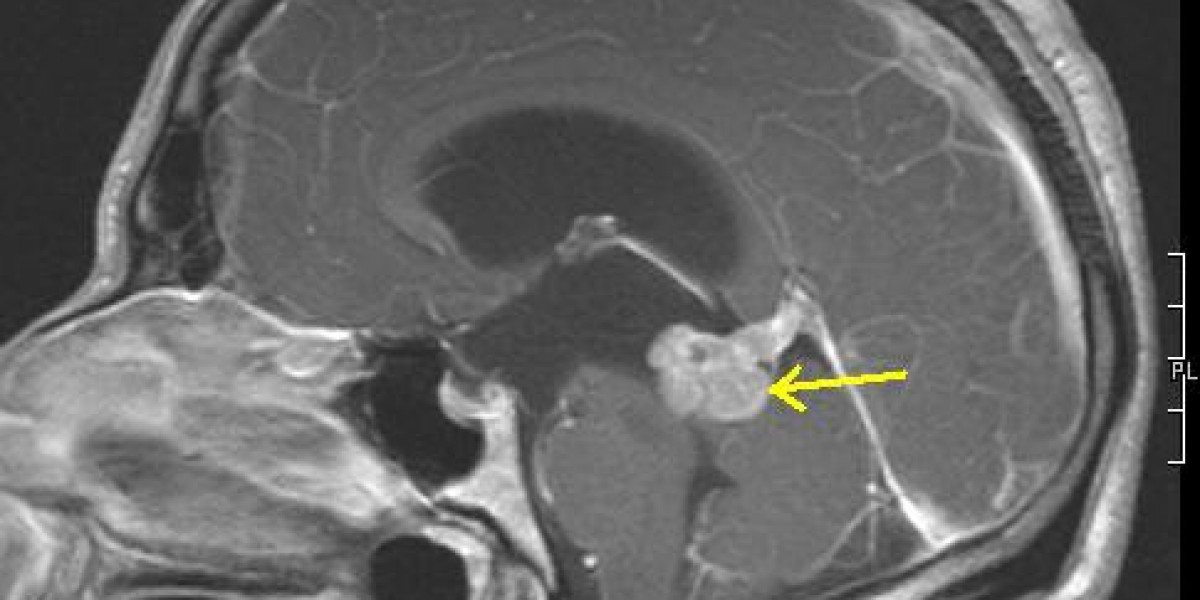
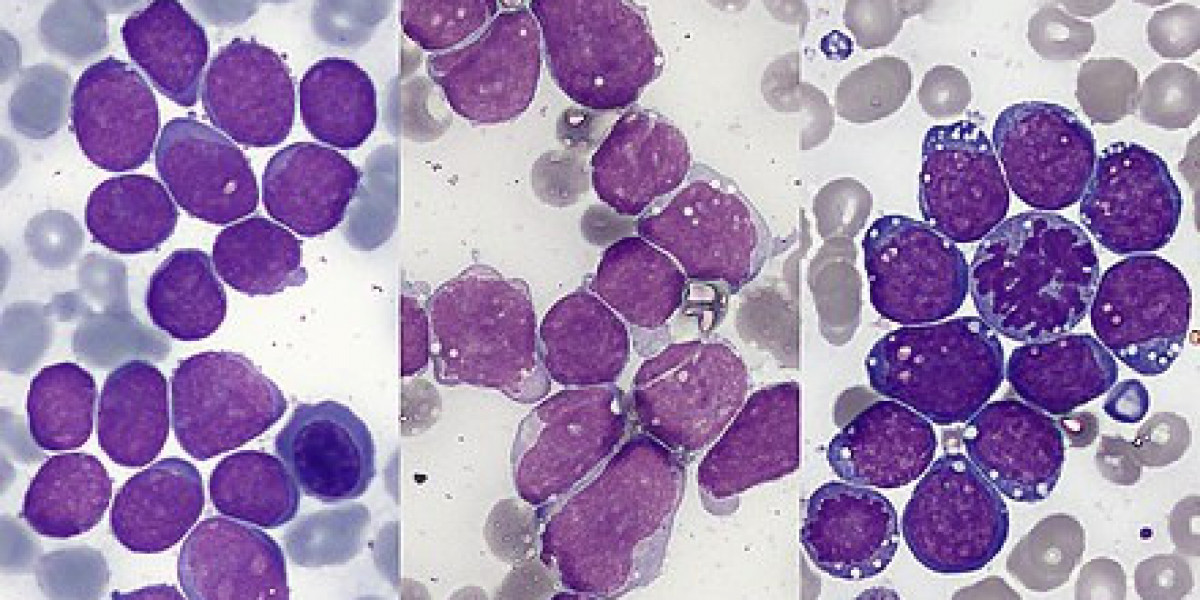
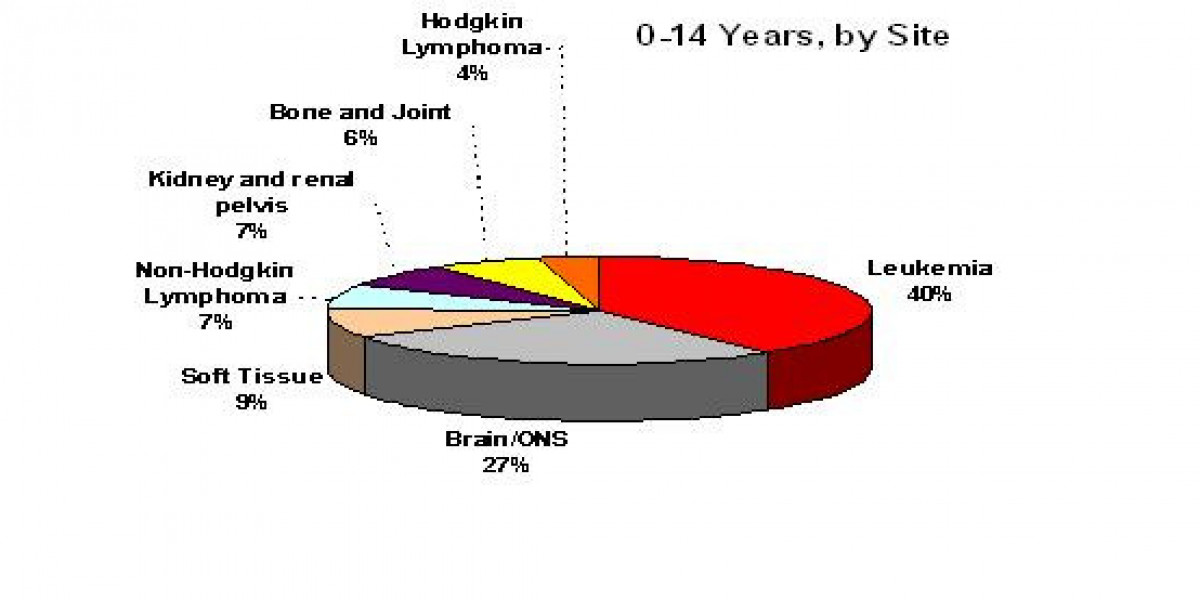
They were thinking it was non-Hodgkin’s. But after doing more tests, they realized that it was acute lymphoblastic leukemia, both B- and T-cell with other mutations.
I understand that my cancer is one that you either have one or the other, not both. It’s not typically found in adults and it usually doesn’t grow as fast as mine does.
Treatment
They [said], “We have to get you an oncologist and we have to keep you here until we could do the next steps.”
I spent the night in the ER. The next morning, they admitted me into the hospital for about two weeks.
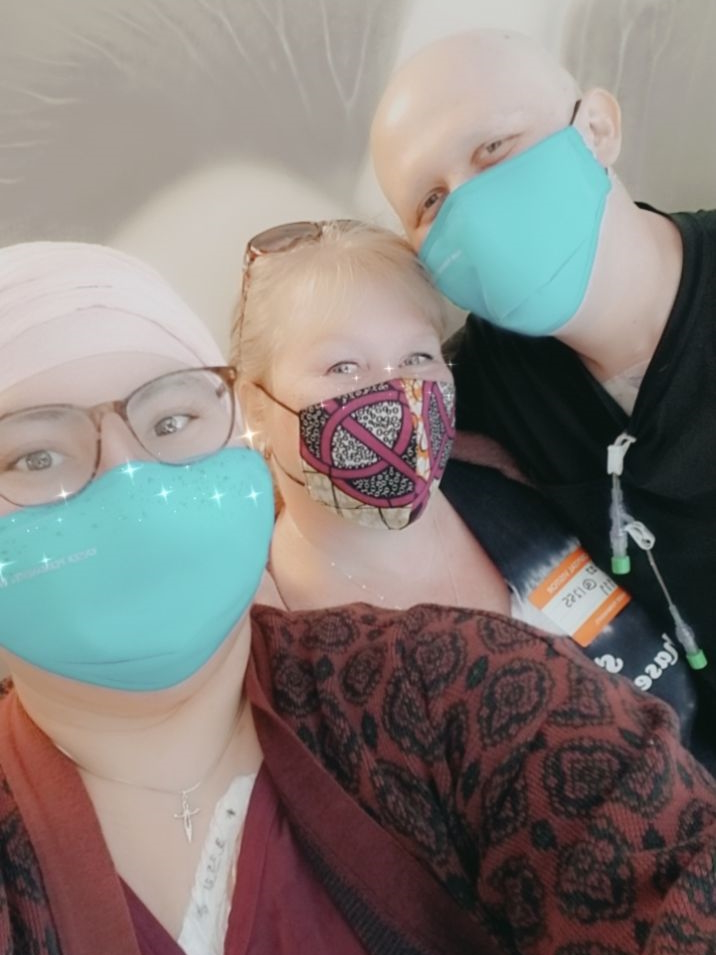
I couldn’t see my family and friends in person except out the window of the room that I was sharing with someone. I was on the third floor so I would look down and they looked like little ants.



I was having such a tough time and I was crying. Luckily, one nurse, the head of that floor, came in to talk to me. She actually allowed my mom — if she had her COVID vaccinations, took a COVID test beforehand, wore a mask, all that stuff — to come in.
It was the first time I saw her since going into the ER. I just cried and hugged my mom. That was all I wanted to do because it was such a scary moment. I will forever be so grateful to this woman because for her to let me do that was the best thing ever.


Treatment plan
I got my oncologist. I was released from the hospital for about four days, just enough time to pack.
I started my stay in March. It was [a] six-step plan. I don’t remember what it was called, but the first step was being in the hospital, getting different types of chemos around the clock in a way. I got spinal tap chemo, chemo through the veins. I did radiation as well. I did that for the whole month.
We checked my body with a PET scan and I was actually in remission. It was so exciting. Then they started step two.
Halfway through, the mutations figured out the treatment plan and mutated to fight against the treatment so I was no longer in remission. Because of that, we couldn’t finish the six-step plan.
Luckily, my oncologist was talking to Stanford and they had a double CAR T-cell therapy trial going on. I said, “Yes, I will do anything.” I know that it was a trial. But knowing that going through this could possibly cure me [and] also help other people in the end, that was super important to me. My whole life, I just wanted to help people.

Double CAR T-cell therapy clinical trial
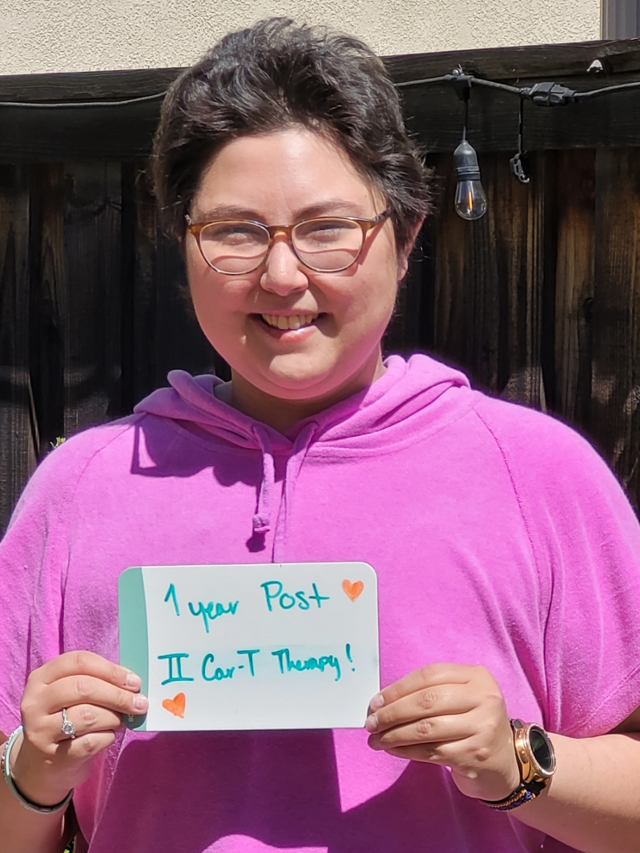
We went to Stanford [and] did a double CAR T-cell therapy. I did it in June and it was fantastic.
Dr. Muffly at Stanford, who was doing the trial, [was] the one that talked to me and became my primary over there.
I did actually have neurological problems through it. There were side effects, but in general, the process is very easy and it was very interesting to learn. That put me in remission for a little while.
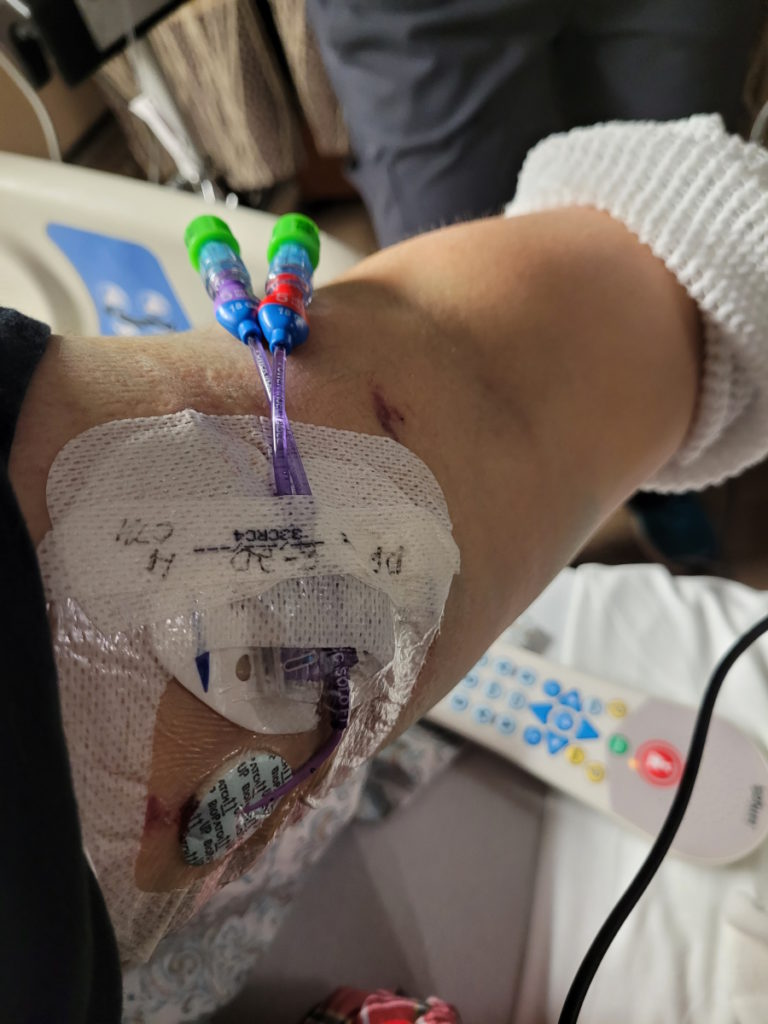
Two weeks before I went into the hospital for the double CAR T-cell therapy, I went in as an outpatient and they took the T cells out. It was a very easy process. It was just like giving blood if you’ve ever done that. They just take the [T cells] out and put the remaining blood back into your body.
What they did with the T cells was make them like little ninjas. You get put inpatient and when they put the CAR T cells in my body, it was just like getting any other infusion. Then you just hang out and see what happens.
They watched you. They do neurological tests every day where they ask you questions. You have to write your name every day as well to see where you are [and] if you’re going to have a neurological issue. They watch for other side effects as well. But for the most part, it’s just easy.
I was in remission for a short time. Then I came out of remission. The cells that they were attacking were C19 and C21. My body figured out the treatment plan again and changed itself to then attack the CAR T so the cancer began to grow back.
It was only maybe a month or two. It might not have even been that long because I got my double CAR T-cell [on] June 11 then I got my bone marrow transplant [on] August 27. It wasn’t that long in between.
The process of joining a clinical trial
There was a lot of paperwork. They go through that information with you. I remember being in the office and it ended up being like an hour and a half meeting instead of a 30-minute meeting because there was just a lot to go through.
They explained how the process worked as [simply] as they possibly could so that was nice.



Honestly, the bone marrow transplant was the hardest treatment I have been through.

Bone marrow transplant
We tried a bone marrow transplant. They knocked everything out of my body. At that point, I was [at] Stanford for about four or five months already for the double CAR T and then another five to six months for the bone marrow transplant.
Honestly, the bone marrow transplant was the hardest treatment I have been through.
They already knew that I needed a bone marrow transplant prior to the double CAR T. They just thought that they would get a little bit longer before they can give it to me, but it really wasn’t that long.
They [paired] with Be The Match to find a match for me and I ended up getting the perfect match. They were a year younger than me, but that was all I knew.
I did four days of radiation, twice a day. It was [the] full body but also localized to the lung area and sternum area. I also did heavy-duty chemo for about four days to maybe even five days. Then they gave me the bone marrow, which was the big bag.
My donor went above and beyond to be able to be my donor. They got a tattoo a few months prior to being asked to be my donor because they had no idea. They told me, “They can’t be your donor now unless you say that it’s okay.”



My donor got all the information to show this is a good location where I got it, all the stuff was clean, [and] all this other stuff, went above and beyond to still be my donor. I was like, “Of course, yes, they could still be my donor. Let’s do this.” The fact that they did that was so amazing to me because that really showed they really wanted to help.
They gave me the bone marrow and that was a three-hour process, I believe. Then I just hung out in the hospital as the side effects started.
With a bone marrow transplant, you get graft versus host disease. To treat graft versus host disease, they give you steroids. They did that and immunosuppressants.
They figured out that my cancer feeds off of those. I was in remission and then I wasn’t because the steroids and the immunosuppressants caused my cancer to grow.


I think that one was maybe two months. I got to go home a week before Christmas after my bone marrow transplant. I was not in remission at that point, but it was low enough that they could deal with it.
Then after that, I was put on experimental chemo, called navitoclax, paired with venetoclax, which is a normal chemo. I was on that for seven months. I did really [well] and then my body figured it out.
Now I’m on Blincyto. I’m on my two-week break. After two weeks, I get put into the hospital for two days and start round two on the day that I get admitted.
I’m watched for two weeks, get sent home for the remaining four weeks of treatment, and then go to the infusion center every week to get my bags changed. Then two-week break and then back in the hospital for round three. They want to do this for as long as my body will allow it, basically.
I was trying very hard to be positive, but it was difficult during that time.