Margo’s Plasmacytoid Bladder Cancer Story
Margo W., Bladder Cancer, Stage 1
Symptom: Blood in urine
Treatments: Chemotherapy, surgery (radical cystectomy)
Margo’s Plasmacytoid Bladder Cancer Story

Margo never expected to develop bladder cancer, let alone two versions at the same time.
When Margo noticed something was off, she visited her OB/GYN, then a urologist and urologist oncologist. If she hadn’t advocated for herself, she would not have gone to MD Anderson and discovered a second diagnosis of plasmacytoid, a rare and often deadly form of bladder cancer.
Margo underwent intense chemotherapy and a radical cystectomy to save her life. Margo shares her story of dealing with loss and isolation during treatment, finding humor and the sliver linings in life, and writing a book about her incredible journey.
- Name: Margo W.
- 1st Symptoms:
- Blood in urine
- Diagnosis (DX):
- Stage 1 bladder cancer
- Plasmacytoid
- Tests for DX:
- Cystoscopy
- TURBT
- Treatment:
- Chemotherapy
- Methotrexate, vinblastine, doxorubicin and cisplatin
- Radical cystectomy
- Chemotherapy
- 1st Symptoms and Self-Advocacy
- Introduction
- Cystoscopy and TURBT
- In mid-December, you find a urologist. What happened at the appointment?
- Did you know you were going to have a cystoscopy before the appointment?
- What was the cystoscopy like?
- Did you have localized anesthesia or a painkiller?
- Results of the cystoscopy
- Transurethral resection of the bladder tumor (TURBT)
- Managing scanxiety while waiting for results
- How did you find out the results?
- How were you feeling?
- Breaking the News to Loved Ones
- Getting a Second Opinion
- Second Diagnosis
- Receiving an additional diagnosis
- Processing the plasmacytoid diagnosis
- What were you feeling?
- The importance of self-advocacy and getting additional opinions
- Seeing a specialist
- Don’t worry about hurting doctors’ feelings
- Many doctors say, "It's your prerogative, and you go do what's best for you."
- Treatment
- Chemotherapy
- What was the plan going forward?
- The chemo plan was methotrexate, vinblastine, doxorubicin and cisplatin. What were the major side effects, and what helped with them?
- What was it about that moment in particular where you felt this eruption of all this emotion?
- Giving yourself grace to grieve
- Undergoing chemo during the pandemic
- How were you able to manage the extra isolation?
- Radical Cystectomy
- Undergoing a radical cystectomy (removal of the bladder) for 7-8 hours
- Finding the silver linings
- What were your options after the radical cystectomy?
- Anxiety surrounding the neobladder
- What guidance do you have for someone getting a radical cystectomy?
- Changing perspective
- Talking to others who have been through it
- Hair Loss
- Reflections
- Normalizing the conversation about sexual health effects
- Physical effects of treatment
- Emotional effects of treatment
- What other losses did you experience around this time?
- Losing your mom
- Taking time to celebrate remission
- Experiencing more loss
- Getting through so much loss
- You filmed a video as Wonder Woman. What did that mean to you?
- Margo’s book “Gratitude in the Storm: When Not Dying Is Enough to Keep Fighting"
- Chemotherapy
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
1st Symptoms and Self-Advocacy
Introduction
Tell us about yourself
I am a seize-the-day, make-the-most-of-life, passion-for-life kind of a gal, and I pretty much always have been. For example, we go on family dive trips. I got my children certified to dive when they were 13, the earliest age that you could do it. We like to travel. We love our dogs. We love spending time together. I’m married to a great guy and I consider myself very fortunate.
You noticed something wasn’t right in November 2019. What happened?
I think one of the things that is very common for cancer patients is that we don’t feel anything. Nothing’s up. We don’t have any pain symptoms or discomfort or anything like that. It was the same for me, except for that one day late in November, I noticed that my urine was the color of rosé, like a deep rosé.

I thought, “Well, that’s not right.” I’m old enough that menstruation could not have anything to do with it, but women are often kind of swept under the rug when it comes to things like that. At any rate, it stopped. The afternoon was clear. Then the next morning, it happened again. A little bit of blood in the urine. Then I never had it again. That’s the only symptom I had.
I consulted Dr. Google, which is both a good and a bad thing. I immediately went to a lab and did a UTI test. Now you can get them over the counter, which is awesome. I was on extra alert and a little concerned.
I have developed over the years a way of saying to myself, “I don’t have that information. If it is worst-case scenario, I will have plenty of time to stress and worry and fret over it. If it’s not worst-case scenario, why put myself through that in the meantime?” I tried very hard to hang on to that. The lab called and said, “Great news, it’s not a UTI.” I was like, “No, that is not great news. UTI would be so much better.”

OB-GYN appointment
I called the OB-GYN. I treat her very much like my GP. A lot of us do, I think, especially if your GP retires, and you’re like, “Yeah, she knows me. We had babies together.” I called the nurses there, got a hold of one of them, and I told her what had happened. She said, “Well, let’s just keep an eye on it.”
I thought to myself, “Nope, I’m not doing that, because nothing good happens from waiting.” What’s the worst thing that happens if I go right away to a urologist and find out that it is nothing? I don’t know what it could have been that was nothing, but it might have been.
What am I? I’m not a doctor, so I don’t know. That information can only help me. Waiting cannot at all help me. That would absolutely make things worse, especially given that it was actually something nefarious.
I immediately started looking for a urologist, and for one that I could get in to see pretty quickly. It was 2 weeks out, so I made the appointment with the urologist, who had a good reputation.
How did you research and make decisions?
First, I call my friends. I say, “Do we have a urologist in the stable of providers?” We do the same thing with shoes. “I need silver platform shoes for a dance. Does anybody have one?” Nobody had a urologist. I did do some research and looked for health grades and a couple other things like that, and I did what I could for due diligence. He had a good reputation, and everybody seemed to love him.
Cystoscopy and TURBT
In mid-December, you find a urologist. What happened at the appointment?
I don’t know the outcome, and I’m doing the discovery. I’m getting the answers. It’s very scary. We could very easily go to DEFCON 5. What good is that going to do? I can’t operate at my best abilities to make decisions and continue self-care and advocating for myself if I’m just freaked out.
I kept doing that, but it’s beginning to take more effort at this point. But I did that, and we went in. That was early mid-December. A little nervous, not too bad. Went in, did the cystoscopy, and I actually could see it. You could look over on the monitor and see this little soft cauliflower wafting. It looks kind of pretty.
Did you know you were going to have a cystoscopy before the appointment?
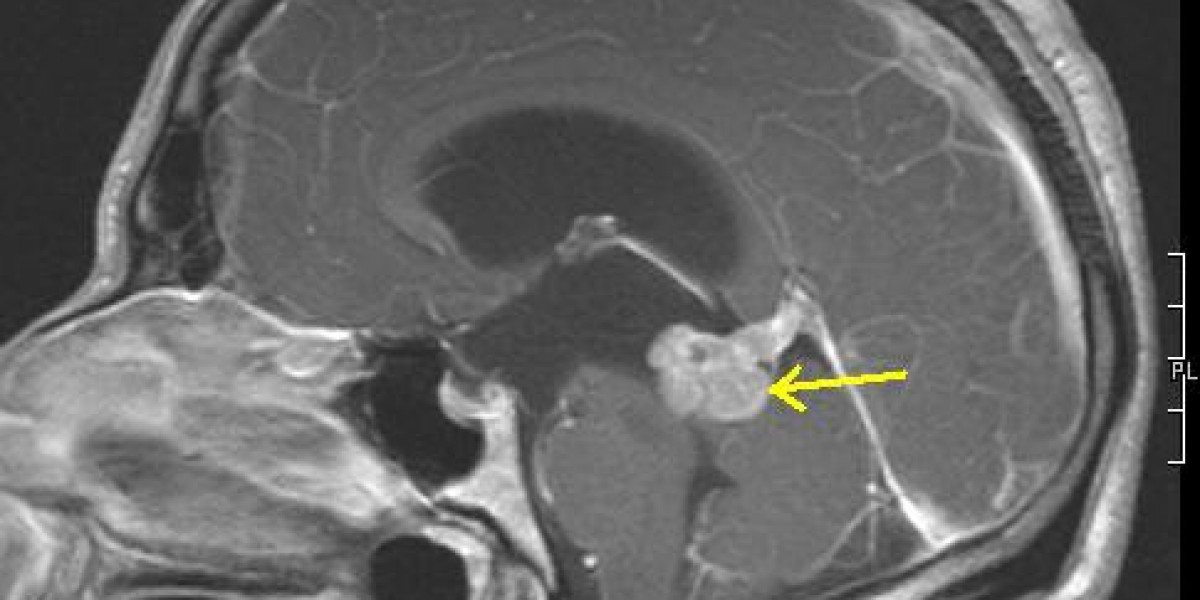
Actually, I just collapsed 2 appointments together. I went into the first appointment with the urologist. He said, “Yes, we should do some looking around. Go get an MRI, and let’s meet back here for an appointment.” The MRI had showed nothing.

I actually tried to cancel the cystoscopy because I was like, “Since there’s nothing on the MRI, I guess we can go ahead and say that it’s all fine.” They were like, “Sometimes it doesn’t show everything.” Then we ended up with a cystoscopy. That was after Christmas. That was actually a day before my birthday, on the 27th.
What was the cystoscopy like?
What I will tell you is that men complain about this a lot more than women do. It’s a little more complicated. There’s more acreage that has to be covered with a man, but they’re basically slipping a tiny tube with a camera through your urethra to head on into the bladder and have a look-see around. That’s being shown on a screen. It might have an easier term than that, but that’s what’s happening.
Did you have localized anesthesia or a painkiller?
They said it’s not necessary. I said, “Well, maybe for you. Can I please have a Xanax at least? Or I’m going to have 2 margaritas before I come in here. Either one.” They gave me a Xanax.
Your urethra is one of the several areas that is designed to be a one-way street. It is not comfortable. It was worth the discussion. If you’re a doctor and you’re doing 20 of these a day or something, it’s nothing to you, but it’s not nothing to the patients.
Results of the cystoscopy
[The doctor] said, “Oh, yeah, that’s a lesion.” That was his less scary word for a tumor. I learned that that’s what he meant when I had coffee with a good friend of mine who shares the same birthday as me the next day. I said, “Oh, I’m not really worried about it because he said it was just a lesion.”
She said, “Yeah, that’s a nice word for a tumor.” She’s a doctor. I thought, and then I said, “Yeah, but at that point, I’m still feeling pretty positive because it could be a tumor. It could still be benign. Those happen as well.” The next step was to schedule the transurethral resection of the bladder tumor.
Transurethral resection of the bladder tumor (TURBT)
They again go in through the urethra and use whatever tools that they use to remove tumors. I imagine there’s cutting things involved. Then they send that off for biopsy to find out what’s going on with it.
Managing scanxiety while waiting for results
I focused on that I still had my kids at home and family to enjoy and everything else I could think of. I also had work, so I just focused on everything else that I could think of. Again, I’m flexing that muscle more and more and strengthening it to be able to put it off and say, “I’ll wait till I have more information before I freak out or get concerned.” I also discontinued Googling all this stuff at that point, which is what I advise.
»MORE: Patients describe dealing with scanxiety and waiting for results
How did you find out the results?
6 days later, I still had a catheter, which is just no fun. You’re carrying a bag around. 6 days later, I was in the office. They remove the catheter, and they go, “Okay, so you have stage 1 highly aggressive bladder cancer.” That’s staggering.
I thought I had a contract with cancer. I will do the lifestyle things over here, and you leave me alone. I thought that I had made that arrangement. Cancer didn’t sign that contract, so it was void.
Then he drew a crude picture, just like a basic picture of, “Here’s a bladder; here’s the ureters.” He said, “Here’s what’s going on. Stage 1 means it’s only in the bladder. It hasn’t crept through to some of the other layers — 2, 3, 4 and so on. The good news about that is that we can treat this with BCG.” I don’t remember what that stands for, but it’s related to what they use to treat tuberculosis.
Immunotherapy in this case would be inconvenient, not very pleasant. Again, it’s going through the urethra to deliver immunotherapy to the bladder. At this point, I’m just thinking, “Ugh, okay, so now I’ve got to do this every 6 weeks. Then I’ve got to have another cystoscopy, so I’ve got to do this for the next 2 years.” I’m making peace with that. That’s what’s happening in that doctor visit.

How were you feeling?
I think this is probably the case for a lot of us. You’re thinking, “This cannot be. This doesn’t make any sense to me. Nothing about this makes sense to me. This couldn’t be more out of the blue.” Zero kind of cancer runs in my family. Lots of other stuff, but just not that.
Smokers are associated with many kinds of cancer, and actually, bladder cancer is one of the things. So I’m like, “It’s not that.” Because in the meantime, I had done research on causes, trying to understand how we got here? I gave up sodas. I eat clean. I drink a lot of water. I exercise. I do all those things.
I thought I had a contract with cancer. I will do the lifestyle things over here, and you leave me alone. I thought that I had made that arrangement. Cancer didn’t sign that contract, so it was void, and you just never know. I’m told by doctors that sometimes you can figure it out, and sometimes you can’t. Sometimes it’s just random, which is 100% unsatisfying.
All of that’s going on in your head at one time. How did this happen? How can this be true? Come on, universe, higher being. I have enough character. I feel like now I am hogging the character. Somebody else wants to have a shot at going through something difficult. I’d been through a lot already in life. That’s what I thought. Really, another thing that’s really hard? All of that was going on through my head at the time, and it’s frightening.
»MORE: Patients share how they processed a cancer diagnosis

Breaking the News to Loved Ones
How did you break the news to the rest of the family?
My hubby was with me the whole time for all of that, which was really great. His name is Coleman, and he’s unbelievable. I think that caregivers have a whole different set of needs than patients. They go through all of it with us, just not the physical part of it. They can’t lean on us as patients to be there for them, so they definitely need to have resources and support.
It was wonderful that he was able to be that support for me. With me, I could squeeze his hand as tight as I needed to, and he could handle that. Then we just looked at each other like, “Okay, well, we’re going to get through this somehow, some way. We don’t need to know all of the ways and the details and what comes. We don’t need to know all those things. We just know we’re going to get through this.”
Talking to your kids about cancer
My kids at this point are 19 and 21. They’re adults. One’s in town. One is not in town. This is not news you like to break over the phone to people.
Part of what made this hard for me telling my kids is that I’m their only living parent. When they were in middle school, their father died. I was not married to him at the time, but he died. There wasn’t a reason that he should have died, but he did. He basically died from alcoholism. He drank himself to death.


That was a terrible experience for me to have to come home and tell them that their father had died. Not only was I thinking I don’t want to worry them because I am their only parent. Even though they’re 19 and 21, they still need parents and family. That was the biggest concern I had. How do I make sure that I explain this to them in a way that doesn’t feel as scary and life-threatening and doesn’t freak them out?
I don’t want to mince words either. I don’t want to mislead them. I don’t want to sugarcoat it. Kind of choosing the right way to communicate with each of them. Now, at this point, that’s all I know about my cancer. I’m still thinking it’s garden variety, essentially, and this is going to be really inconvenient. That’s what I understood at that point.

Is there anything you learned in terms of guidance for other people on how to navigate that?
Yes, there is. I learned that the best way to do this, at least for me and definitely for them, is to go right to it and to say, “Reed, we just got home from the doctor, and it does turn out that this is cancer. It is stage 1, and here’s what we’re going to do about it.”
Right to the point. Don’t go heavy into details. In this case, I just said, “Here’s the therapy.” They’re grown, so they can understand it, but that’s not the point of the conversation. Then follow it up right away with, “And we’re going to get through this.”
Getting a Second Opinion
Why did you get a second opinion?
Actually, it’s my job. I sell health insurance policies for self-employed people, like realtors. I had learned a lot about what most policies do and don’t include. Second opinion is really, really important. I’d learned that the data shows the number of misdiagnoses is really high. I didn’t know how high. For cancer, it’s actually 70%. That’s what my oncologist told me.
I said, “How many of the cases you see are wrong, or it’s an incomplete diagnosis?” They all said 70% in separate appointments. I knew to take advantage of a second opinion service, which I did. The second opinion service was an oncologist urologist.
Back up for a second. I went to see a urologist. At this point, what do I know? Do I know that there’s a urologist oncologist in the world? I know nothing of this world. I don’t know that I should be seeing an oncologist urologist. Who tells you that? Not your urologist.
There’s a lot of this seeking information, gathering it real time while you’re experiencing it, trying to process it, trying to hold it together and figuring out what’s the best path forward. It, as you know, is a mind-numbing experience. It’s a soul-numbing experience.
Without this experience, you may not have known to ask for a second opinion
I may not have. I’d kind of like to think I would, but I can’t say for a fact that I would. You don’t know what you don’t know. If you are aware and then you choose to not get that information, that’s on you. But if you don’t even know, it’s tough to say, “Oh, I should have gone and done that.” I’m really glad I did go get that second opinion from a specialist, who was a urologist oncologist.
Seeing the urologist oncologist
He said, “About 20 or 30% of the time” — this was his number — “stage 1 bladder cancer is actually stage 2 bladder cancer. Completely different treatment regimen. I want you to go get a blue light cystoscopy.”
I thought, “Oh, that sounds almost fun.” The blue light picks up on cancer cells that aren’t visible to the naked eye. Okay, that sounds like a good thing to do. I hung up the phone. Actually, it was a virtual visit.
Then I called my urologist office, and he said, “Oh, I don’t have the equipment to do that. It’s a good test. I believe in it, and one day we’ll all use it. But right now, nobody in Austin does it.”
Going to MD Anderson
I did my own research. I live in Austin, Texas. MD Anderson is right down the road in Houston, 3 hours away. I’m aware of them and their reputation, and I thought, “Well, I’m stage 1, garden variety bladder cancer. I don’t need to go to MD Anderson.” Why did I think that? I have no idea. That’s kind of the bias that you have — it’s not that serious. I so wanted to cling to that.

At any rate, when the second MD recommended the blue light, I couldn’t find one here. I had to start doing research, and I found that there were 3 places nearby. One was San Antonio, and 2 were in Houston. What I did — and I think this is really smart — is always ask the people who know more than you do and ideally who know the most of any one thing.
What did I do? I sent those names to the urologist oncologist, who was the specialist in my second opinion. I said, “What do you think of these?” He goes, “I can vouch for these 2 cases. I’m just saying, don’t go to the one in San Antonio.” He didn’t vouch for that one.

Then I basically figured out how you open up records and let hospitals see your records and start the process. You don’t know how any of that works, and so you’re figuring that out as you go. How do you get an appointment? I went through the process of getting the documents in my records and everything to them.
Within days, appointments started showing up on my calendar. MD Anderson — you’re going to have a blood test; you’re going to have all these different things. I thought, “Okay, I guess I’m going to MD Anderson.” They’re one of the best. They’re rated the top all the time. I felt confident about that and good that I’d found one that was highly [recommended]. I was, at this point, still hopeful that this was just mainly super inconvenient and uncomfortable.
Seeing Dr. Ashish Kamat
He’s a superhero. He’s amazing. I had an occasion to see him at a bladder cancer event recently, where I was one of the 3 patients that shared their stories. We just hugged. I had sent him the first chapter of my book and said, “I don’t know if you feel like saying anything.”
The second kind is lethal. It is very rare, it’s fatal, and it always comes back. We have to do everything. If we do everything, we throw the kitchen sink at it, we can save your life.
Dr. Ashish Kamat
I didn’t know if he was going to read this email or not. He replied back through one of his assistants. “Here’s what I think.” He said these glowing, wonderful things. 2 years to the month later, he told me in person at this event, “I want the whole book, and I want it signed by you.” Okay, I’ll do that for you.
Second Diagnosis
Receiving an additional diagnosis
[Seeing him] would save my life. I did a bunch of breathing exercises while we sat in the room waiting for him to come in. I’d done blood work and X-rays and things, but I’m still thinking that he’s going to go, “Yep, we need to do immunotherapy.” But I also know there’s a chance that it could be something else.
It takes forever. There’s so much waiting. The good news about all that waiting is not that you’re waiting with your thoughts to yourself, but it is that when it’s your turn, they’re there for you. I used all of my best coping skills to get through the [waiting]. It felt like an hour. It probably was 30 minutes. Breathing in and out, and just trying to stay calm.
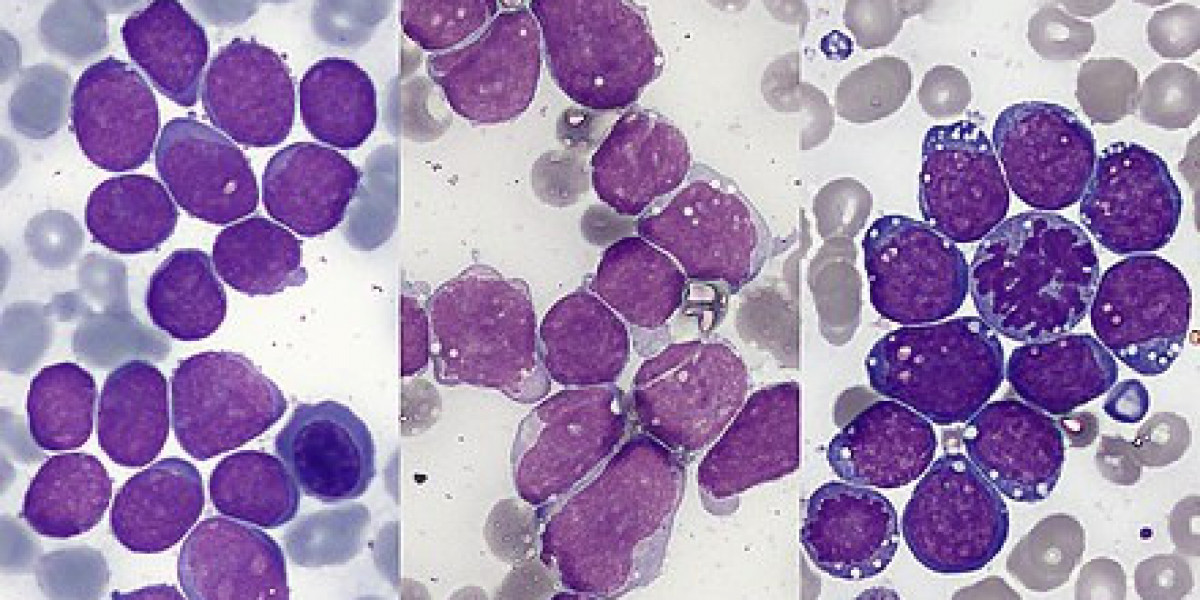
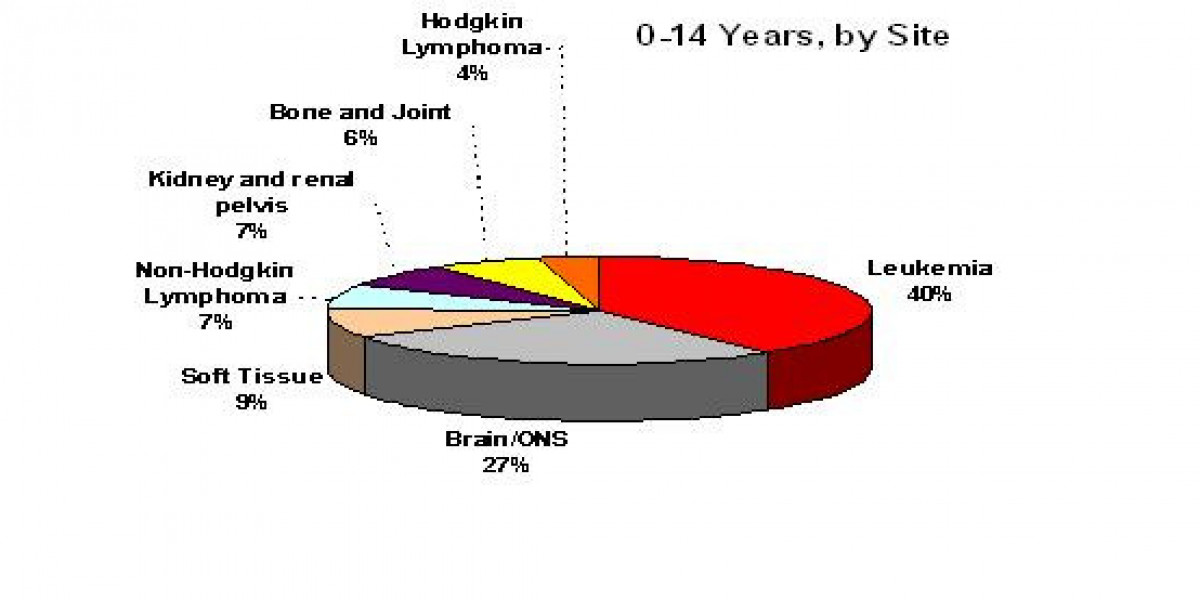
When he came in and talked to us, he got right to the point. He said, “We’re not going to do a blue light cystoscopy tomorrow, or at all. Because looking at your slides, at the images from your biopsy, you have not 1, but 2 forms of cancer in your bladder.”

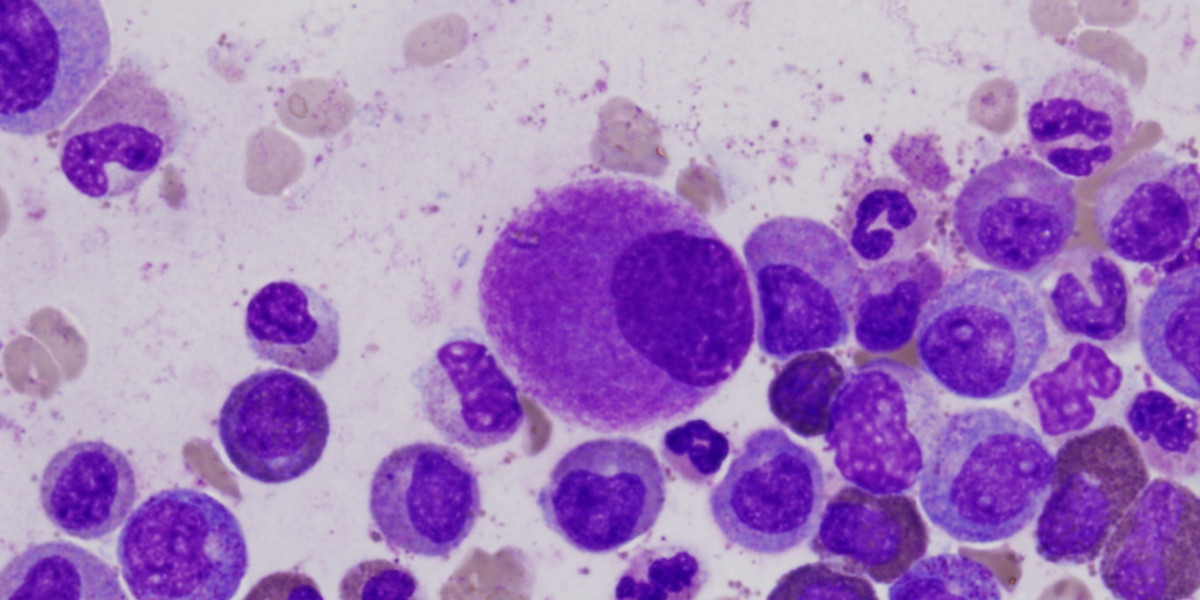
I’m thinking, “Yet another thing I had no idea was possible.” What’s the limit? How many is the most you can have in one place? 2? He said, “The first kind that you already know about will respond to BCG. The second kind is lethal. It is very rare, it’s fatal, and it always comes back. We have to do everything. If we do everything, we throw the kitchen sink at it, we can save your life.”
Processing the plasmacytoid diagnosis
That is the hardest thing I’ve ever had to hear. You don’t even know how to react when that’s what you hear. Save my life? I’m fine. Look at me. I’m healthy. I don’t feel anything.
He went on to explain that this second form is a plasmacytoid, and it does sinister things like cloak itself and make itself look like bladder cells to the other bladder cells. That’s very sneaky. That is one of the reasons it’s so hard to treat.
Throwing the kitchen sink at it in this case was 4 kinds of chemo every other week for 8 weeks, followed by a radical cystectomy. That is the removal of the bladder and usually some other things along the way.