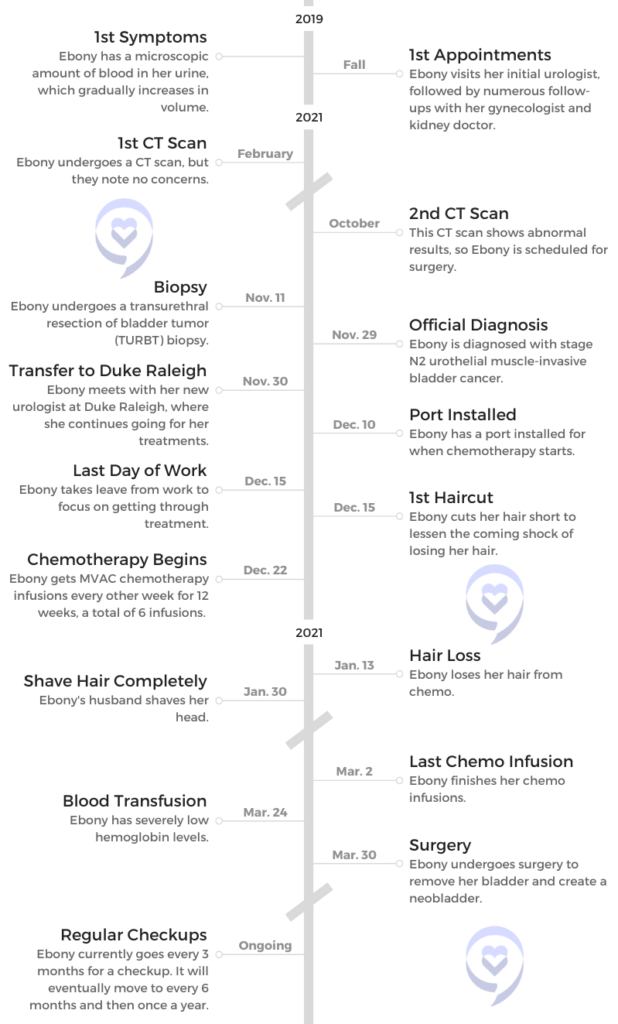
Ebony’s Stage N2 Muscle-Invasive Bladder Cancer Story
Symptoms: Blood in urine, weight gain
Treatment: MVAC chemotherapy, bladder removal surgery, neobladder

Ebony’s Stage N2 Muscle-Invasive Bladder Cancer Story

Ebony was only 45 years old when she was diagnosed with stage N2 bladder cancer. Having lost her own father at a young age, she had to process the fear of not being there for her 3 sons.
She then underwent MVAC chemotherapy and an 8-hour surgery to remove her bladder. As part of this surgery, part of Ebony’s small intestines were used to create a neobladder.
Ebony shares her cancer journey, including taking control of her hair loss, the experience of African Americans in the medical system, the importance of self-advocacy and support, and using her story to be a light for others.
- Name: Ebony G.
- Symptoms:
- Microscopic amount of blood in urine
- Increased to visible amount of blood
- Pain when urinating
- Weight gain in midsection
- Diagnosis (DX): Urothelial muscle-invasive bladder cancer
- Staging: N2
- This means the cancer has spread to 2 or more lymph nodes in the region
- Tests for (DX):
- CT scans
- Checking IUD for issues
- Cystoscopy
- Biopsy
- Treatment:
- MVAC chemotherapy
- Methotrexate, vinblastine sulfate, doxorubicin hydrochloride (Adriamycin), and cisplatin
- 6 infusions, biweekly
- Surgery
- Removal of the bladder
- Neobladder
- MVAC chemotherapy
- Introduction and First Symptoms
- Finally Getting Diagnosed
- Next Steps After Diagnosis
- Processing the full diagnosis
- Losing a parent at a young age
- Worrying about leaving your kids behind
- Telling your children about the diagnosis
- How did your urologist describe the results to you?
- Receiving treatment at Duke Raleigh Hospital
- Receiving a binder of information to prepare you
- Was the pamphlet comforting, or what did you feel looking at it?
- Hair Loss
- Treatment and Recovery
- What was your chemo regimen?
- How did your doctor describe the treatment regimen to you?
- Importance of hearing from people you can relate to
- What were your options for removing your bladder?
- How long was the surgery?
- Recovering from the surgery
- Recovery in terms of sexual health
- How long has it been since the surgery?
- Finding Support and Advice
- Reflections
This interview has been edited for clarity. This is not medical advice. Consult with your healthcare provider for treatment decisions.
Introduction and First Symptoms
Tell us about yourself
Hi, my name is Ebony, and I was 45 when I was diagnosed with bladder cancer.
I am married. I have 3 sons. I am an engineer by day. I just want to live my best life like everyone else. Those are the biggest things. I really want to live my best life and help others do the same.
What were your first symptoms?
My initial symptom was after a visit with my annual gynecologist, and they noticed that there was blood in my urine [at] a microscopic level. I couldn’t even see it, but a microscopic level of blood in my urine. They referred me to a urologist to try to look into what was going on. [It] kind of freaked me out.

That’s how it started over 2 years ago, pre-COVID actually. I proceeded with the urologist. They couldn’t find anything. I had different scans [and] different scopes that were performed and initially couldn’t find anything.
He said, “We’ll just keep you on a schedule. You’ll just keep coming every 6 months, and we’ll check on you.” I didn’t have any other red flags. Generally very healthy. [I] never went to the doctor except for my physicals. [I was] not on any other medication, [and I had] no high blood pressure, cholesterol, diabetes, no other health issues. [I] was pretty active.
The doctor was kind of like, “We’re not seeing any smoking gun, so we’ll just keep watching you.” That’s how it started. [I] didn’t have any pain [and] no other symptoms.
Looking for potential causes
We looked at several things. We initially thought it was a UTI, so I was prescribed an antibiotic and then thought, “Okay, we’re good to go.” It kept going, so then the next thing was, “Okay, let’s check your IUD. Go back to your gynecologist, check the placement of your ID, [and] make sure that that’s in place.”

[I] did that. [The] gynecologist was like, “Yep, it’s good. No problems.” Then they thought we have to confirm what the source of the blood was. Is it just menopausal stuff going on? What’s going on?
I’ve read and studied that most women are misdiagnosed because I guess our bodies are a little complicated. People go grasp for the initial things that may be probable, but all of those things were batting zero.
He referred me to a kidney doctor to look at the functions of my kidneys, and all was well. I went back to the urologist, and they were like, “Well, we’ll just keep an eye on you.” That eye on me was a check every 6 months.
What scope did they perform?
I can’t remember the technical term right now, but it was a scope where they basically filled my bladder with liquid and checked. It kind of would magnify if there was anything going on in my bladder.
There wasn’t anything to be found. Generally, it made me feel like I needed to urinate. [It] wasn’t the most comfortable feeling. That was one of the initial scopes, and then also a CT.
How were you feeling through this process?
I wanted to trust my doctors to believe that they would know what was wrong. When the doctor was telling me, “Well, we don’t know,” I was like, “Okay, if you don’t know, yeah, I’m a bit concerned.”
He even told me at one point, “There are some people that over time, as they get older, their bodies function differently, and maybe that’s just you. I was like, “No bueno. No, I’ve never had this as a problem.”
I remember telling my husband, “I feel like the woman with the issue of blood, like biblically. It just won’t stop. I don’t understand.” At that point, a year passes, and now I can actually see the blood when I went to the bathroom.
Now it’s more prevalent, and my doctor is still saying, “Maybe this is just what your body’s going to do.” I was like, “This can’t be likely. This can’t make sense.”

I even started gaining weight, particularly in my midsection. I remember thinking I never gain weight in my midsection. With each of my boys, I gained 60 pounds when I was pregnant. But every time, I always gained weight in my hips and thighs.
For me to gain it in my tummy area, I was like, “This doesn’t seem right.” But even the nurse at the practice was like, “You’re in your upper-40s, mid-40s. Maybe that’s just what’s happening. You’re just gaining weight in a different way. I was like, “Yeah, no.”
I was very concerned because they couldn’t figure out what was going on after a year and a half. It got to the point where I was like, “If they don’t find something this time —” fast-forward, that was September 2021, ” — I’m going to someone else.” I also at that point had had the IUD removed. [I was] just trying to remove every possible potential cause, and we still couldn’t find anything.
Can you list those emotions you were feeling during this?
Confusion. Despair at some points because I just really didn’t know. I was wondering if there was some underlying something. I was Googling things [and] trying to figure [it] out. [I was] just kind of confused and lost as to how the professionals don’t know.
Honestly, I had never heard of bladder cancer. It never occurred to me as something to delve more into. To be honest, I don’t ever recall my urologist saying, “If you see this additional sign, then maybe we should dig more, or let me know.” I was very concerned and stressed about what this could be.

Finally Getting Diagnosed
How did you finally get a diagnosis?
The other thing was I’m not sick typically, and I remember actually coming down with COVID [in] August of 2021. Everybody was catching COVID, but still, I was like, “I’m never sick, and now all of a sudden, here we are.”
Then I actually started feeling pain when I urinated. I was supposed to go to the urologist [for] my normal 6-month check that August. Due to him being on vacation, we rescheduled the appointment. When we rescheduled the appointment, then I ended up with COVID, and so that appointment was pushed off to October.
I went in again, and he said, “You know what? We’ll go ahead and do another CT. Then we’ll see from there.” We did another CT in October. Then he called me in his office, and he’s like, “Something’s abnormal here. We’re going to need to have a surgical procedure because I see something.”
He also did that scope, the same scope that he did that year prior. In that scope, he saw something, which freaked me out. Then he’s like, “I actually need to see you in surgery in the next 2 weeks.”
I was like, “What? 2 weeks? Surgery?” My last surgery was, at that point, probably 12 [or] 13 years ago when I’d had my last C-section.
We had the abnormal CT, the extra scope that was abnormal, and then the surgical procedure to biopsy this growth that he saw to see more of what was going on.
Processing the possibility of cancer
That was in person. For that appointment to talk about doing the surgery (prior to the biopsy), I was by myself. He did [describe it as a growth or tumor], and I instantly thought cancer.
I was like a ball of tears, and the nurse that was with me said, “You’re going to be okay.” She was extremely comforting. This was a different nurse. She’s like, “I’ve been through this before. You’re going to be just fine.”
But at that moment, I remember thinking, “I’m going to die. What is this? How did we catapult from, ‘Not only it doesn’t seem like much, [but] this is probably what you’re going to always just deal with, because this is just the way your body is functioning,’ to, ‘We need you to have surgery in 2 weeks and dig further to understand what’s going on.’”
It was pretty traumatic by myself in the office, but the nurse tried to reassure me and tell me, “You’re going to be okay.”
What was the value of having someone trying to comfort you?
Honestly, I didn’t believe her, but it was a bit comforting to know that someone had been through something similar. I didn’t have my wits about me to ask more detail of exactly what she meant that she’d been through it, and I haven’t seen her since.
After that few weeks, the urologist ended up referring me to a surgical urologist, one of the top urologists in the area, to proceed with my treatment. While it was a bit comforting, I was still like, “Yeah, I don’t know that you can relate to what I’m going through. I don’t even know how you know what I’m going through. Did you really have this procedure?”
Did you feel a shift when you found out it could be cancer?
There were 2 shifts. That was one shift because I remember thinking, “I’ve trusted you for a year and a half to try to find something, and what was it about everything that has gone on in the past year and a half where you didn’t find anything?”

Of course, we trust doctors [and] trust that people are going to do things in our best interest. But I began to wonder what other signs were there that maybe you overlooked. I honestly was a bit angry because I thought, “I’ve been coming to you for a year and a half, and you haven’t seen anything. Now, all of a sudden, I need to be in surgery in 2 weeks.”
That was one shift, and then the second shift was when he told me specifically after the surgery that the growth was confirmed to be cancerous and that he wanted to refer me to someone else that could better help me.
Undergoing a biopsy on the growth
November 11th last year (2021) was when I had the surgery. I was extremely scared because even with my 3 C-sections, I was very alert in what was going on. At this point, I’m like, “Oh, you’re going to take me under?”
I’m just a bit paranoid about, like, am I going to come out okay? Then the fact that you have had a challenging time diagnosing me, and now you’re about to take me under to try to figure out what this is. I was Googling left and right [and] Googling the report to try to figure out, “What does this mean?”
That was on November 11th. Then we had plans for Thanksgiving to go visit family. I remember thinking, “You should be able to tell me what the results are almost instantly, even if it’s a week.”
But it was November 29th, 2021, before I found out that it was cancerous. The crazy thing was, in the meantime, I got this random text from another hospital not even in the state that was something about checking into the cancer center.
[It] freaked me out because at this point, it was in between me having the surgery and getting the results. I remember texting my husband, “Oh my God, does this mean I have cancer?”
But it was a total random text from a hospital not even in the state that we live in. He was like, “Ebony, don’t worry about it. That’s just a random text. It’s nothing.” But I was like, “This is way coincidental.”

Waiting for the biopsy results
It was like 6 in the evening when I received the text. I couldn’t call the doctor’s office because it was after doctor’s hours, so after the working hours. I remember calling the doctor’s office the next day, saying, “Hey, I got this random text. Does this mean that this tumor was deemed to be cancerous?”
The receptionist was like, “Oh, no, no, no, that’s not even affiliated with our practice.” But I was like, “Of all the times to get this random text… Is this the Lord preparing me for what’s about to come?” I’m thinking all the worst.
Nevertheless, we went to visit family for Thanksgiving, but the entire time, in the back of my mind I was like, “Am I going to get this result? When am I going to get the result? And is the result going to be one of my biggest fears?”
Fast-forward to November 29th. They called me in to come get the results. I remember thinking, “Okay, the fact that they’ve called me in can’t be good.” My husband went with me for that appointment, and that’s when I first saw the verbiage on the report to say that I had a high-grade urothelial, muscular-invasive bladder cancer.
I was like, “What? What does this mean? What stage? What?” I remember that was the second shift, where I was just devastated. I don’t know that I’ve ever cried like that after getting those results.
»MORE: Patients describe dealing with scanxiety and waiting for results
What was your official diagnosis?
They diagnosed me with stage 2 urothelial muscular-invasive bladder cancer. I want to say it was staged N2 because a couple of my lymph nodes were impacted.
Next Steps After Diagnosis
Processing the full diagnosis
I remember my eyes just welling up. I couldn’t even read what was on the paper just because I was so emotional from what the diagnosis was. He was optimistic and trying to be encouraging in that visit.
I just remember thinking, “What if I hadn’t come back? I’m listening to you all, and you’re saying, ‘Oh, well, it should be fine. Your body’s just maybe designed to work this way.’ What if I hadn’t come back? What if I didn’t prioritize this visit based off of some of the other verbiage that y’all were sharing with me, yet me telling you something doesn’t seem right? What if I hadn’t come back? Now you’re telling me that I’ve got this aggressive tumor growing in my body, and now you’re telling me you’re going to refer me to someone else because it’s a little more complicated than what you thought. Really?”
Losing a parent at a young age
Imagine this. I’m a 45-year-old woman, married with 3 kids. Our sons at the time were 20, 13, and 14. When I was a senior in high school, my father passed.
When I heard the diagnosis, I instantly thought, ‘Here we go. I’m not going to be around for my children.’
It was a pretty quick sickness. I remember thinking, “He’s going to recover just fine.” But I didn’t know the seriousness of what was going on. I was devastated when he died my senior year in high school. There’s always been a part of me that has wondered, “What if that happens to me? What if my boys are left without me?”
»MORE: Parents describe how they handled cancer with their kids

I’ve gone through pretty much my whole adult life missing that presence. He wasn’t able to meet my husband. He wasn’t able to meet the boys. He wasn’t able to offer insight on different things. I wasn’t able to ask him questions like, “Daddy, what do you think about this? What do you think about that?” Just input that I would have loved to have received.
Worrying about leaving your kids behind
I’ve always wondered and prayed that that would not be my outcome. When I heard the diagnosis, I instantly thought, “Here we go. I’m not going to be around for my children. What are the things that I’ll be able to do so they’ll remember me, they’ll know me, [and] they’ll know my feelings for them? What can I quickly try to do where they will have fond memories of me?”
They’re still very young, and honestly, there are a lot of memories that I don’t have of my dad because I was young. My instant thought was, “Oh, my God.” I honestly was a bit angry with God.
I’ve had to do a lot of personal work to get beyond missing that presence of my dad and wanting him to be proud and wanting to accomplish certain things. That’s been a lot for me. To think that they would potentially be catapulted into this same space was extremely devastating and challenging for me.
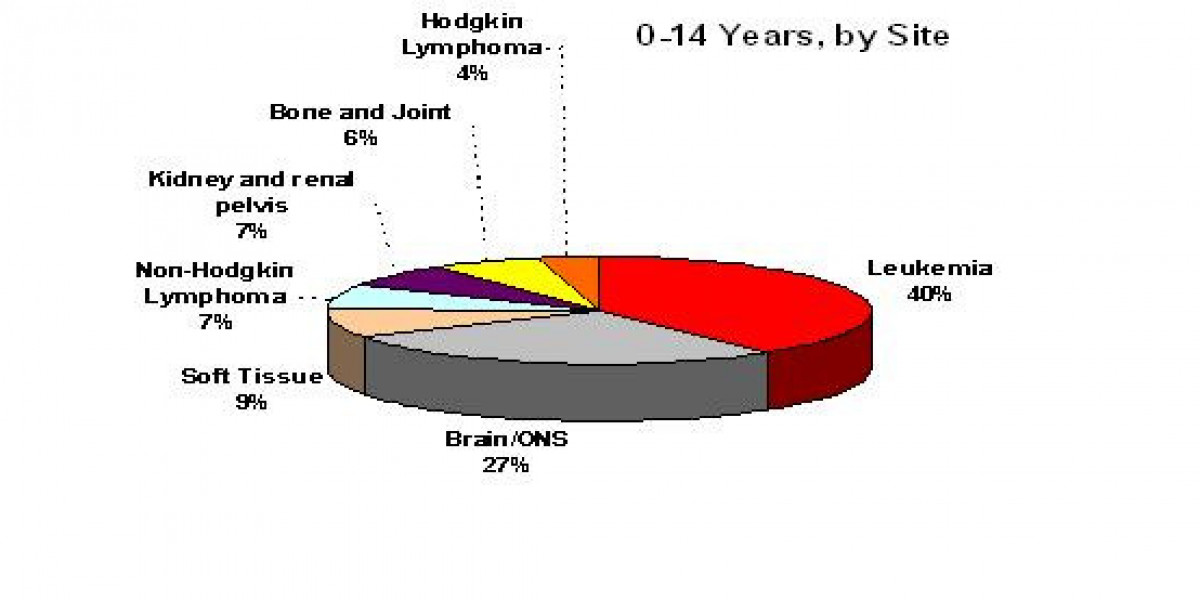
I just remember my instant thought was, “How much time do I have? How much time do I have?” I didn’t know anyone with bladder cancer. I’m a bit of a fluke. The doctors would say, “You’re a unicorn. You’re checking all the boxes, [by] trying to live a healthy lifestyle. Yet here we are. You’ve never smoked. You’re not an older white male, yet here we are.”
It was extremely devastating for me because I remember thinking that my children are going to grow up without their mom. That was a space that I’ve always not wanted to be in because I hated having to experience it myself.
Telling your children about the diagnosis
I’m trying to think how we even came to how we were going to share, because I didn’t want them to worry. We decided not to share much. Initially, we weren’t going to share really much at all because my first appointment with the other urologist, it sounded like, “You’ll still keep your hair. Your hair may thin a little.”
I was planning to continue to work. I was really trying to kind of maintain that normalcy. Fast-forward [to] when we met with the hematologist. He was like, “Oh, no, boo-boo, you’re gonna lose all your hair,” which was extremely devastating. “You’re going to have chemotherapy or infusions every other week. After the second infusion, it’ll be extremely challenging for you.”
Hearing all those things made me say, “Okay, we probably need to share something.” My husband honestly did all the talking when we shared. I’m extremely emotional, and I’m a big crybaby. He was the one that shared. We didn’t discuss details of staging. We weren’t intending to, but the oldest one, who was 20, was instantly like, “Okay, what stage is it?”
We just talked as a family. This is the deal. This is what’s going on, but we will get through this. Like I said, he did all the talking because I would have been a blubbering mess. He did all the talking, and I honestly think that was the best part of it, that he was the one that kind of put a positive spin on it all for them.

How did your urologist describe the results to you?
It was a very short appointment. I remember him asking me if I had any questions, but I was like, “Yeah, I got all the questions, but I don’t know what questions to ask.” I don’t know if he was just struck by the amount of emotion that I was expressing.
It was just more of a, “I’m going to connect you to someone else that is going to help you better than I can.” I remember thinking, “Well, dang.” I was just so overwhelmed. I didn’t know what questions to ask. I had a ton of questions, but I really didn’t even know.
Of course, some of the main questions were, “How serious is this?” There was not any discussion at that time of treatment. No discussion about any of that. I didn’t really get into all of that discussion until I met with my other urologist.
Receiving treatment at Duke Raleigh Hospital
All of my treatments after that point were primarily through Duke Hospital in Raleigh, North Carolina. Honestly, that was probably one of the best decisions for me. It’s great because the treatment was relatively close to us, so we didn’t have to travel far.
After that diagnosis, there was a slew of appointments. I can’t even tell you how many appointments. Every day, it felt like I was at another appointment, and it was a whirlwind of appointments.
That surprised me because I had to go to different doctors for them to check my heart, to check my liver, to check all these different organs. The hematologist knew what my body was about to have to undergo. They were trying to make sure that my organs were going to be able to withstand all of these really harsh treatments that I was about to start taking.
Most of my treatments were at Duke Raleigh. The hematologist and urologist worked hand in hand to enlighten us on what was about to happen.

Receiving a binder of information to prepare you
My first appointment with the urologist was accompanied with this huge binder, this 3-inch binder of tons of information, including a section on hospice care.
All of it was about the medications that I was going to have to take, the potential types of urinary diversion, you name it. That binder was the gospel for me for the next several months. [It was] a little daunting to get that binder. Then there was another little pamphlet that had pictures of people, I guess, that had bladder cancer.
I remember thinking on the cover of that little pamphlet, “None of the people that have been diagnosed with this look like me.” There may have been one woman on the picture, but she wasn’t African American. Everyone on that pamphlet looked older and not like me, but I was like, “Okay, here we go.”
Was the pamphlet comforting, or what did you feel looking at it?
I looked at the different types of urinary diversions when I opened it, and I remember thinking, “Wait a minute.” I was actually kind of vain at the time. I was like, “Wait a minute. What is this? Does this mean I’m going to be left with a bag outside of my body? Does this mean I’m going to lose my hair?”
I was physically trying to think through what the impact was going to be. I remember talking to the urologist initially, and he said, “This is the new and improved one.” I remember him saying, “Your hair will likely thin,” and so I remember thinking, “Okay, I can manage that because I had a ton of hair.”
I was okay. Then right after his appointment, I had the appointment with the hematologist [the] same day. The hematologist was like, “You’re going to lose all of your hair.”
I just was devastated at the thought of, ‘How am I going to manage not having hair?’
I went from, “Okay, I think I can manage this,” to, “Like all of it, all of it?” He’s like, “Yeah, no, without a doubt, you’re going to lose all of your hair.” Again, I [was] just devastated, bawling in the doctor’s office. [I] can’t even read the material that they’re handing to me.
We didn’t tell the boys at that point. It wasn’t until for sure we knew I’m going to be physically impacted. I’m not going to be able to hide it per se. That’s when we decided to share with them.
Hair Loss
The importance of hair as a Black woman
As a black woman, actually it takes a long time for our hair to get to the lengths that we enjoy. My crown, as I call it. There’s a lot of pride and joy in my hair. Actually, for about 7 or 8 years, I had decided to become natural, so not having any chemical products in my hair, not having any relaxers to relax my curl pattern.
I had really worked hard to grow those chemicals out of my hair. [I would] keep cutting the hair and just growing out for it to be at its natural state. To get to this point, where it’s 8 years in the game of being what we call ourselves naturalistas, to find out now it’s all going to come out. Like, what?
Then I’m thinking to myself, “Is it going to grow back?” You hear stories, and you see people where it does grow back. I was like, “What does that mean for me? Is it really going to grow back?”
I just was devastated at the thought of, “How am I going to manage not having hair?” That was honestly the tip of all of the side effects that were going to come from it, but the initial thought was no hair. I’ve worked really hard to become a naturalista and take pride in this crown that I wear, and here we are.
It was incredibly devastating.