Leesa’s Chronic Lymphocytic Leukemia (CLL) Story
Leesa T., Chronic Lymphocytic Leukemia
Symptom: Bruising
Treatments: Imbruvica (ibrutinib), Brukinsa (zanubrutinib)
Leesa’s Chronic Lymphocytic Leukemia (CLL) Story

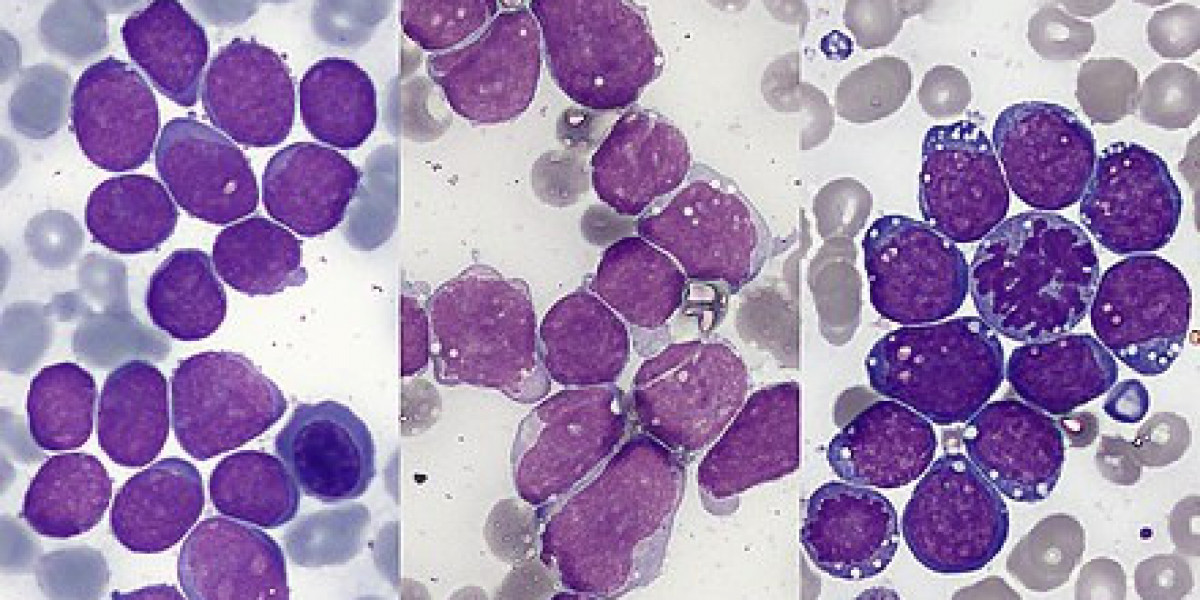
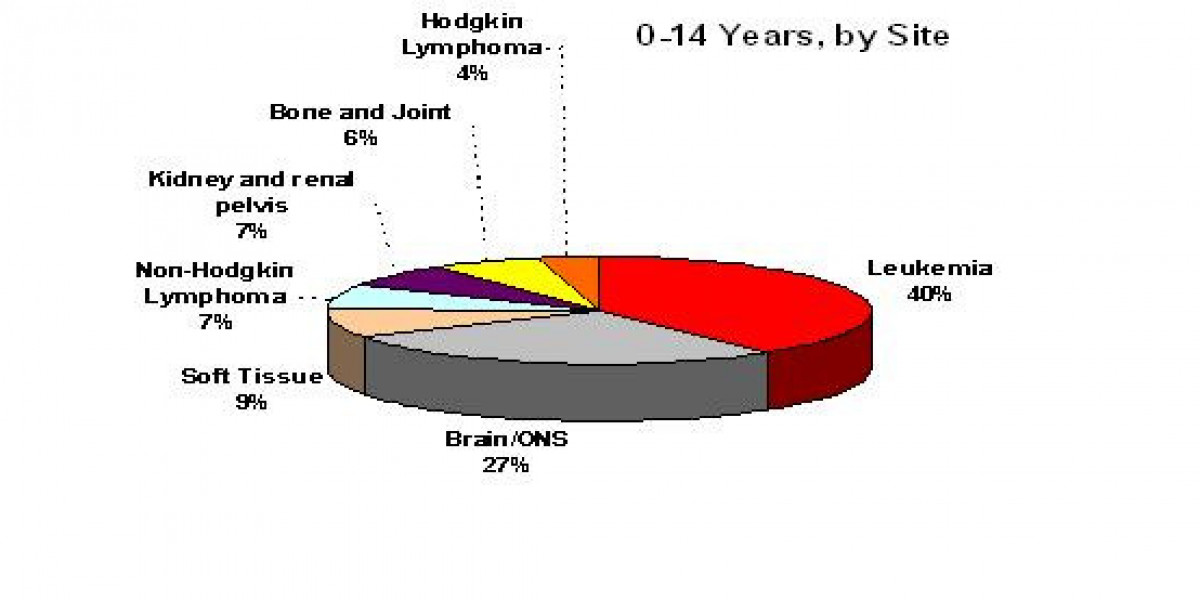
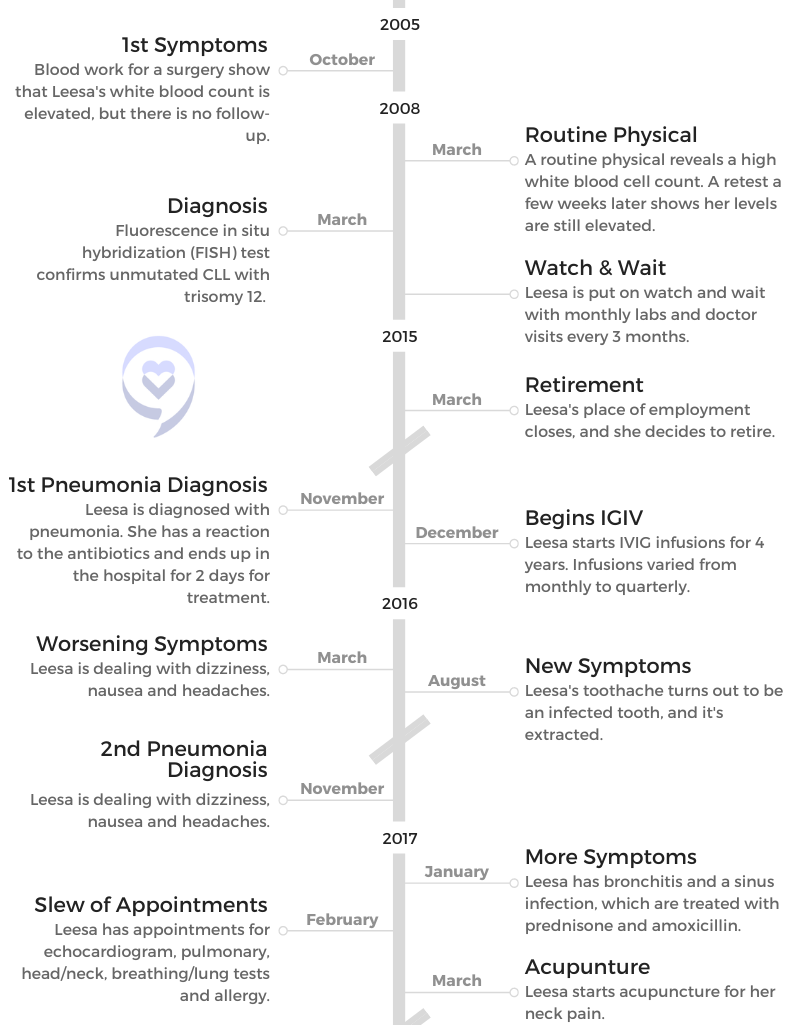
Leesa received an unexpected cancer diagnosis of chronic lymphocytic leukemia (CLL) after a routine physical.
She was put on watch and wait for a decade before starting treatment due to worsening symptoms. These included fatigue, dizziness, infections and ocular disease. Leesa was put on ibrutinib and later switched to zanubrutinib.
Now, 14 years after diagnosis, Leesa reflects on her journey and making the most of the time she has.
Thank you for sharing your story, Leesa!
- Name: Leesa T.
- Diagnosis:
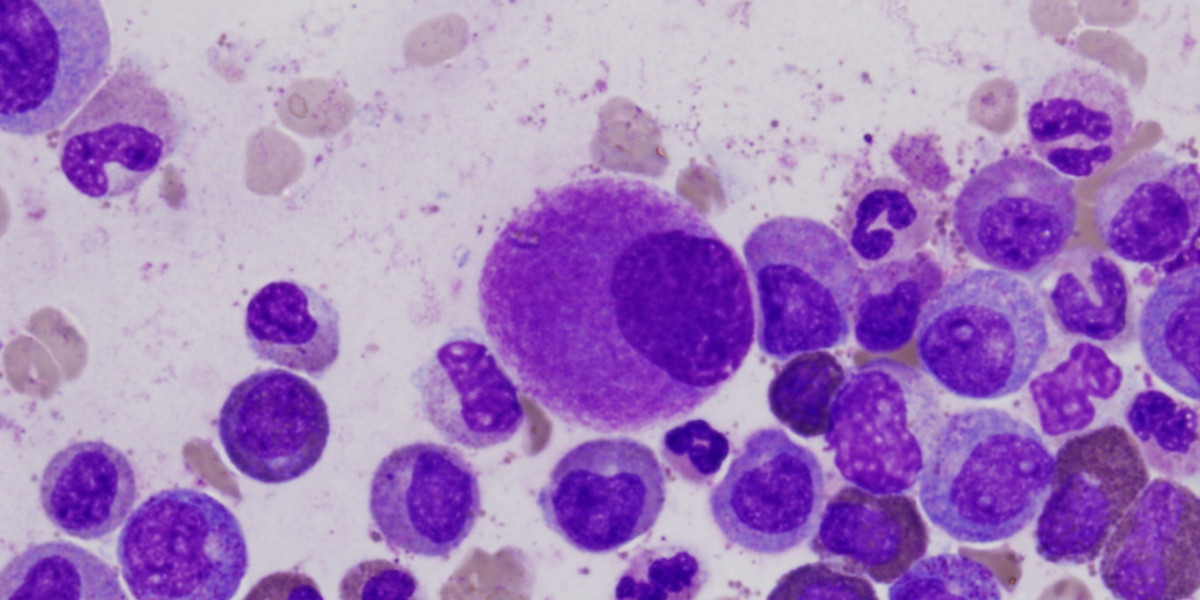
- Non-Hodgkin’s lymphoma
- Subtype: Chronic lymphocytic leukemia (CLL)
- Trisomy 12 unmutated
- 1st Symptoms:
- Bruising, but she didn’t realize until after diagnosis
- Tests for CLL Diagnosis:
- Blood work
- FISH test
- Treatment:
- 10 years of watch and wait
- Imbruvica (ibrutinib)
- Brukinsa (zanubrutinib)
- Side Effect Treatment:
- Eye injections
- Imodium (for GI issues)
- Chronic Lymphocytic Leukemia Diagnosis
- Watch & Wait and CLL Symptoms
- CLL Treatment and Side Effects
- Starting Treatment after Watch & Wait
- Treatment Side Effects
- Treatment side effects and low-purine diet
- Why did you decide not to take the gout medicine?
- What worked for side effects?
- Did you or your doctor make the decision to go off ibrutinib?
- Did Kaiser take care of the insurance and financial side of things?
- Zanubrutinib side effects
- Going to the ER for side effects
- Dealing with diarrhea
- Figuring out how to manage side effects and live life
- Reflections
- More CLL Stories
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
Chronic Lymphocytic Leukemia Diagnosis
Introduction
Tell me about yourself
I like doing puzzles. I like animals, especially cats. I’m married. I live in California and have been retired about 7 years now. I love to travel, although that has been curtailed. Mostly long trips, but I’ve done a few short things. I love my lunch dates with my girlfriends, and that’s me.
I have 4 cats. They’re all seniors, so Dancer and Delilah are 17, and Sammy and Bella are turning 14 on Thursday.
It was really a fantastic distraction for me. You need something bright in your life, and I feel like they were sent to me to help me.


The CLL Diagnosis
You didn’t really have symptoms, so how did the testing and diagnosis process begin in 2008?
I switched insurance, and I decided I’ll have a physical since with this insurance, that’s covered. When my results came back, my doctor said, “Your white blood count is high. Have you been feeling sick?”
I said, “No, I feel great.”
She said, “Then retest in a few weeks,” and I tested again. She said, “Your white blood count is high again. I’m referring your case to a hematologist-oncologist.”
It just floored me. My husband thought that just must be a mistake. You’re healthy; that can’t be true. More blood tests were done. An appointment with hematologist-oncologists and tests confirmed that it was indeed CLL.



How did you process thinking it might be cancer?
Mostly just shock, and it felt like it was just surreal. This can’t really be happening, and I’m going to die. Those thoughts come in your head. “I’m going to die.”
»MORE: Patients share how they processed a cancer diagnosis
What tests did your hematologist-oncologist do?
He’s a hematologist-oncologist, not a CLL specialist. I’m very fortunate in that he’s extremely knowledgeable about CLL.
I had heard of CLL because of my aunt, and she described it. She came from Texas to visit. She described it as, ‘It’s not the kind of cancer that’s going to kill you.’
First off, various types of blood tests. We’ll add all these others on. The other test I had some months later, as I remember, was a bone marrow biopsy, which he was trying to do in his office. I could not tolerate the pain, so that was put off for a time when I could be in a hospital setting and they could give me some sedation. Those were the main tests that I had to get the diagnosis.
[The FISH test revealed it] was trisomy 12 unmutated, which my oncologist said was a moderate progression. It’s not the slowest-growing CLL, and it’s not the fastest-growing. That diagnosis is kind of in the middle.

Processing the CLL diagnosis
Figuring out the path of living with chronic cancer
He told me right away that you’ll be on watch and wait, with having your blood tested about every 3 months and visits with him the same. I think he kind of erred on the side of caution and always has seen me more frequently even than I think some specialists see their patients. That was our course of action.
I had heard of CLL because my aunt, my father’s sister, had CLL, and my dad’s mother, my grandmother, I believe also had CLL. All we knew was she had leukemia, but she lived to be 94 and she was diagnosed late in age. I had heard of CLL because of my aunt, and she described it. She came from Texas to visit. She described it as, “It’s not the kind of cancer that’s going to kill you.”
I never thought I would ever say that I’ve had CLL for 14 years when I was first diagnosed. When I was first diagnosed, I thought I only had a few more years to live.
I think she had actually passed before I was diagnosed, so I couldn’t really give her a call and ask about her experience. But her experience would have been different, because the only drug they had to treat it in 2008 when I was diagnosed was chemo. That’s right when the BTK inhibitors and other drugs were coming out.
She had told me that she was not going to do chemo, and that was her only option at the time. Now, we also know that for people who are unmutated like me, chemo doesn’t work for them very long. It has a very short duration, so I’m really grateful that all these new drugs are available for me.
Processing the CLL diagnosis and breaking the news
I told my husband, and he was just as shocked as me. He cried. I did not tell my father, who was in his late eighties and had mild dementia. I knew that he did not process bad information well, so I chose not to talk to him about it, which is very difficult. You want to be able to share with your [family].
I didn’t have my mother anymore, and I really wanted to share with him, but I knew that for me and for him, that was the best thing to do. I told my good friends. It’s difficult for people to understand this type of cancer and the whole watch and wait thing. My friends were extremely supportive.

A lot of ways it was a blessing, because it taught me, ‘Do not put these fun things off. Do it all now.’

I’ll just say that for the first 6 or 8 months, I really felt like I was just in a complete fog, just going through the motions of life. I’m usually a pretty positive person, but it just knocked me over, and it took me a really long time to wrap my head around it.
Now it’s just part of my life, 14 years later. I never thought I would ever say that I’ve had CLL for 14 years when I was first diagnosed. When I was first diagnosed, I thought I only had a few more years to live.
»MORE: Breaking the news of a diagnosis to loved ones
Living life to the fullest
A lot of ways it was a blessing, because it taught me, “Do not put these fun things off. Do it all now.” There was a trip my best friend asked me to go on with her sister and a friend to the beach, a very expensive place on the beach with massages included and expensive dinners.
I had just bought a new house with my new husband. I’d be like, “That’s just an extravagant, expensive weekend. I can’t do that.” The diagnosis made me say, “I’m going, I can do it. It’s not really that big of a deal.”
There were a lot of moments like that, but that one really stands out in my mind. You just have to put it behind you and enjoy all the days. It’s just something that switches within your own brain.
What support is important from people in your life?
I think you’ll find out pretty early on who’s able to kind of understand it and be supportive to you, and who’s not. Sadly, it doesn’t mean they’re a bad person or anything. They might want to try to sell you this product that they sell. “This is amazing, and it’s going to get rid of your cancer.” They might say, “You should go on this kind of diet,” or that kind of thing. The people who just don’t understand say, “Well, my aunt had it, and she lived to be 90,” or that kind of thing.
You find your people, and they might surprise you who they are and who they aren’t. You just need a couple of supportive people in your life, even one supportive friend or family member, and you go to them.
How the Cancer Could Have Been Caught Earlier

Pulling records from 3 years earlier
My oncologist said, “You probably have had this for a while. See if you can pull some records.” I contacted my doctor’s office, and they faxed the information to me. I’m like, “Wow, he’s right. There it is.”
I had been living with it for at least 3 years, and I suspect a couple of years before that, based on just a couple little minor changes. I started bruising very easily in my early 40s. When my husband first met me, he said, “You’re like a banana,” because I always had maybe about 20 bruises on my legs at any given time. I had to hold my shopping bags out to the side because if they touched my leg, I would bruise.
In retrospect, I should have known, but I was just like, “That’s just me. I’ve been like this for a while.” But it’s definitely a sign.
How do you feel knowing it could have been caught earlier?
When I wracked my brain thinking back to that time, after I got my records, I had this vague memory of the nurse before my surgery — who saw my labs — asking me if I had been sick. That’s a common sign. When your white blood count is high, you’re sick or have an infection.
I said, “No,” and she said, “When your surgery is all said and done and you’re feeling better, you should actually have that checked out or redo your labs.” I totally forgot it, having gone through surgery and recovery for 6 weeks.


I wonder why [my doctor that I really liked] didn’t point it out to me and remind me, because I continued to see him. That should have been a red flag for him to bring that up 6 months later when I saw him, or even while I saw him during recovery. The nurse [should have] called me for a follow-up. But they were not oncologists, and they’re busy.
Watch & Wait and CLL Symptoms
Being Put on Watch and Wait
Reacting to not needing treatment right away
My first reaction is different than a lot of people. A lot of people want it fixed right now, but not me. I’m like, “Oh, thank God, I don’t have to do chemo right now. Watch and wait? I can do that.” That’s how I felt about it.

I realized I didn’t know I felt so bad until I started feeling better.
I just saw him about every 3 months, had my labs done, had a CT scan to get a baseline on swelling of my lymph nodes and other organs that might be affected. That’s fine with me. I want to be on watch and wait for the rest of my life. I never want treatment. That was my thought. Treatment was horrible. That was my thought. But it’s really not.

Did your aunt having CLL make watch and wait less foreign to you?
I did understand that there was this period where it wasn’t going to take her life right away, and she was just living with it, and she was tired. That’s what I knew. She was in another state.
What’s your advice for dealing with watch and wait?
Just try to relax, enjoy it, learn what you can about CLL from reliable sources. Support groups are fantastic. It can be scary, too, in a support group, hearing other people’s stories. I sometimes even felt some guilt because people were so sick.
Here I was working full-time, taking care of my elderly dad’s needs, having fun, living a completely normal life. Granted, when I look back — especially as it neared my 10-year mark when I did need treatment — I was really so sick. When I finally started treatment, I realized how many times I felt so horrible and how much better I felt once I did start treatment.
I had gotten used to feeling bad, used to having these flu-like symptoms, with no clue why and just kind of still carrying on with life the best I could — working, doing everything around the house, living normally within those bounds.
Once I started treatment, of course there are side effects and I had them, but I felt so much better. I realized I didn’t know I felt so bad until I started feeling better.



Worsening Symptoms
Symptoms from November 2015 to December 2017
Dizziness, headaches, nausea, pain on the head, tooth pain that was an infected tooth, pneumonia more than once, bronchitis, sinus infection, pain throughout body, including muscle pain, some arthritis, then at the end of it, vertigo and near blindness in left eye.
I don’t know how I did it. I don’t know how I did it, but you just do. You realize how strong you are when you don’t think you are, and I hope to not have to do that again.
How did you juggle all the doctor’s appointments?
It was difficult. In 2016, the company I was working for closed in the spring, and that coincided with my health just taking a turn for the worst. Thankfully, I was not working. There was one week that I had 7 doctor appointments, but they weren’t all for me. I believe 5 were for me, 1 or 2 were for my dad, and I had to take the cat to the vet.
My whole week was consumed with doctor appointments. I was retired before my husband, and he would say, “What do you do all day? Don’t you get bored? Do you get bored?” “Never.” It was a busy time with appointments and sickness.
Ocular Disease
How did it start?
Especially at the end, I would say those last couple of years, my oncologist had mentioned several times, “I think it’s about time starting treatment.” I was kind of digging my heels in. I was supposed to start in the fall, and I said, “I want to wait until after Christmas.” I kind of wish I didn’t, because that’s when my whole eye thing started.
It was after Christmas. It was actually December 28th. I was in a restaurant, waiting for my friend to have lunch. I was very early because I had been at some kind of doctor appointment.

I’m waiting at the table, looking towards the door for when she comes in so I can wave and flag her to the table, and it was blurry. I kept taking my glasses off and looking at them, then putting them on and looking at the door. I just wasn’t seeing clearly. My friend came. We had lunch.
The next day, it was worse. I think on the 30th, my husband and I went for a walk, and I had on sunglasses. I did the same thing, kept taking them on and off. “What’s wrong with these?” Holding them up, I told my husband, “It feels like I’m like blind in my left eye or going blind.”

‘Nothing we can do, or anybody can do.’
If you don’t get answers or you don’t like the answers from one doctor, go to another one. Don’t just take their word for it.
Seeing the doctor
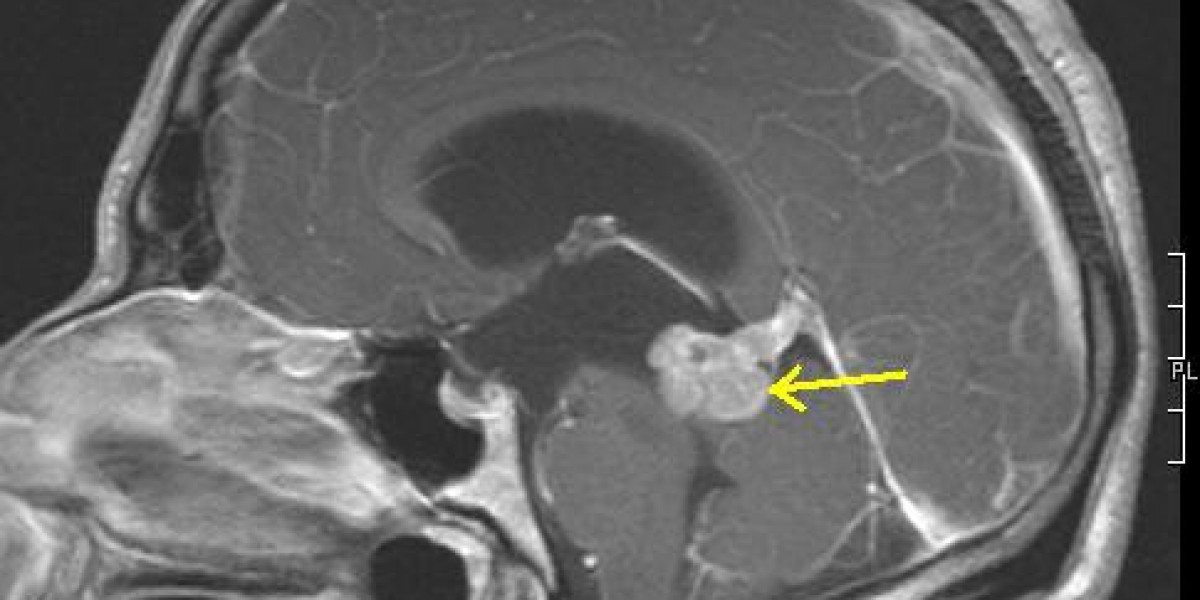
He goes, “Well, you better go to the eye doctor.” Here it is, the end of December [around] New Year’s. There were not a lot of doctors working. I was able to get in January 2nd, and the eye doctor confirmed that I had swelling and such in my eye.
That doctor said, “There’s really not a lot I can do or anybody can do. Just follow up with your regular eye doctor in a few weeks.” I don’t remember if it was that doctor or a different doctor that also ordered an MRI. I did have an MRI.
This was all happening so fast that my vision was changing daily for the worse. I made a follow-up with my doctor, and they were like, “You can’t get in for a week.” I’m like, “No, no, no, I have to get in.” I did get in, and that eye doctor didn’t say, “There’s nothing you can do.” That eye doctor said, “If it were my eye, I would see a retina specialist as soon as possible.” He gave me the information.
What did it feel like being told no one could do anything?
“Nothing we can do, or anybody can do.” This is something people should take away from this. If you don’t get answers or you don’t like the answers from one doctor, go to another one. Don’t just take their word for it. They’re a trained professional with a degree on the wall. No. Speak out for yourself.
Thankfully, that second doctor right away was very concerned. He said, “If it were me, I would see a retina specialist ASAP,” because there wasn’t anything he could do. Only a specialist could work with me. It was within a couple of days, and again I was on the phone saying, “No, I can’t wait a week or 3 weeks or whatever it was. I need to get in now.”

Seeing the retina specialist
My husband had to drive me, and it was about a half an hour away. [They] dilated my eyes. He did the test and showed me my eye on a graph on his computer with all the swelling and damage and ridges. He said that he suggested eye injections. I believe it’s a type of chemo medication.
Nobody wants to hear “eye injections,” but when you are going blind, you’re like, “Bring it on. Give me that injection. Start it now.” It wasn’t pleasant, but it certainly wasn’t the worst thing in the world. I ended up seeing him every few weeks and always had to have a driver because I really couldn’t even see after.
I’d get a headache. I’d be walking out holding on to my husband, really in rough shape. [I’d use] the hat and the magazine to block the sun