Michele’s Acute Myeloid Leukemia Story
Michele G., Acute Myeloid Leukemia (AML)
1st symptoms: Bruising, tiredness, shortness of breath, itching
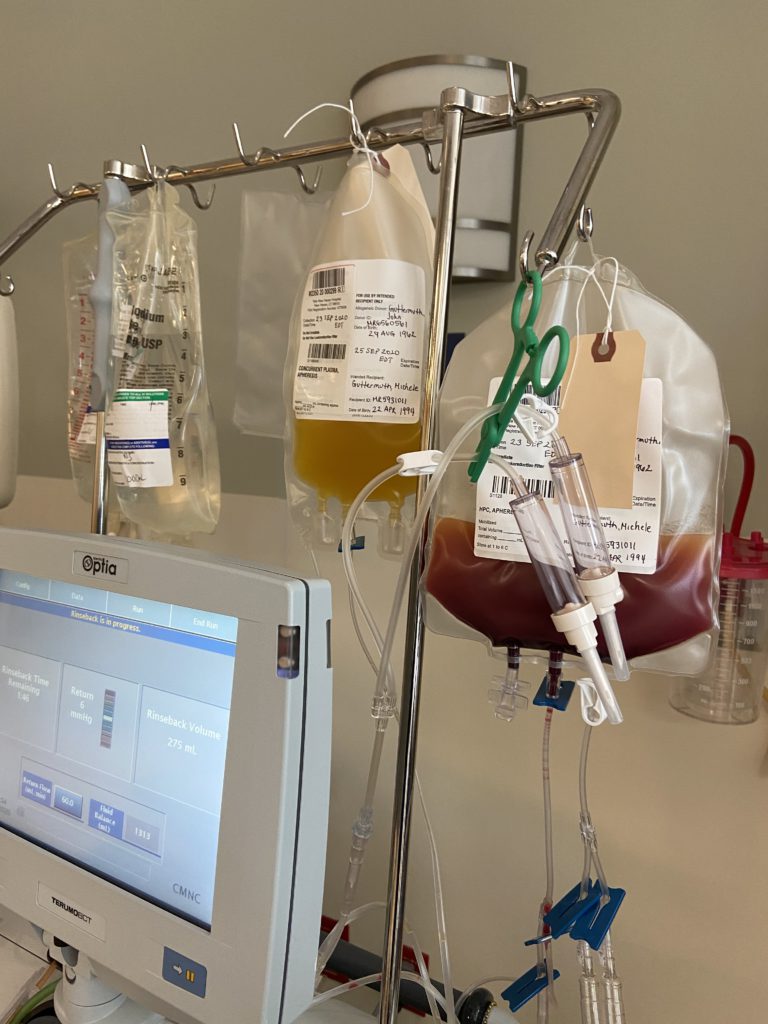
Treatment: IV chemo, 2 stem cell transplants, targeted chemo pill
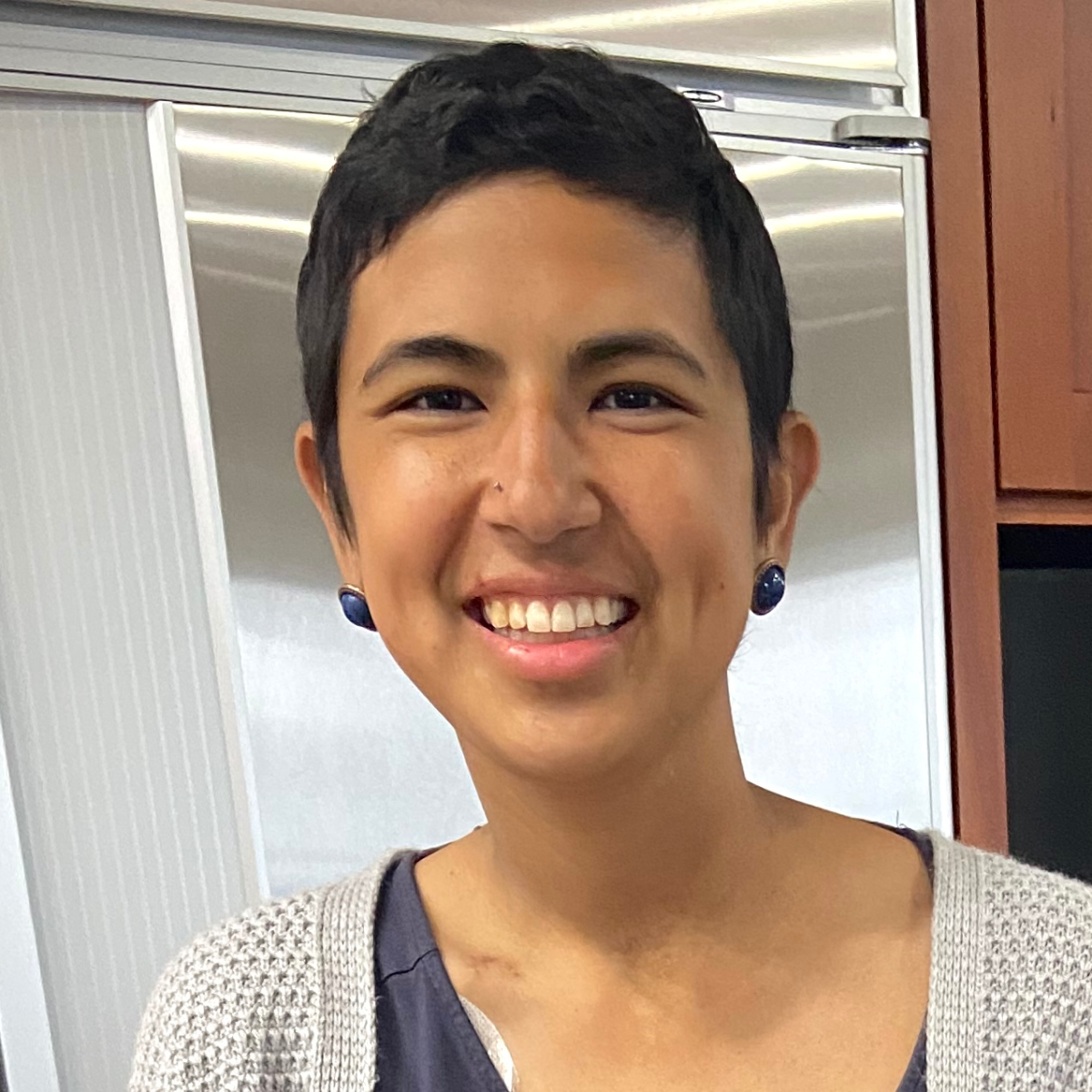
Michele’s Acute Myeloid Leukemia Story
Michele loved the outdoors and the beach. At 24, she was living a vibrant and active life until she was diagnosed with relapsed refractory acute myeloid leukemia.
In this video series, Michele shares her story of diagnosis, chemo and stem cell treatment, relapse, and the side effects she had to endure. Her continuing journey through AML is such a shining light of inspiration, especially for young cancer patients.
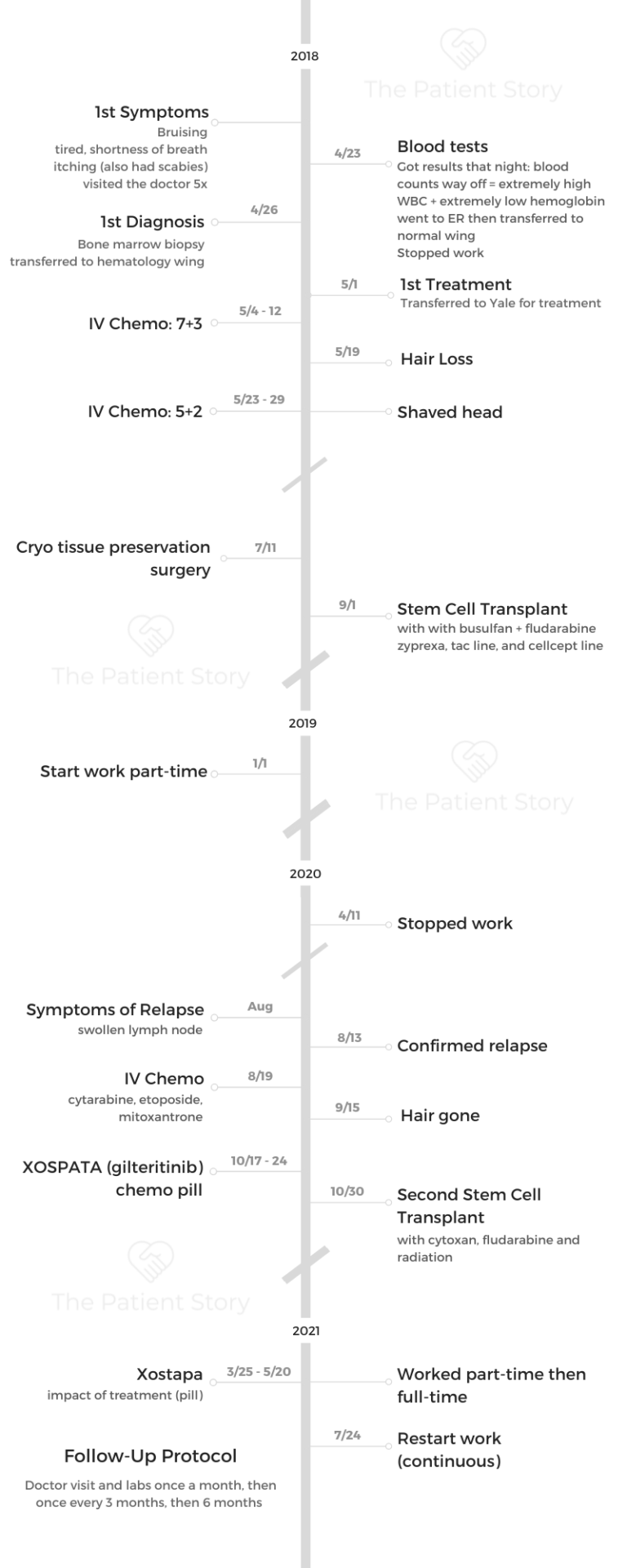
- Name: Michele G.
- Diagnosis (DX)
- Acute myeloid leukemia (relapsed/refractory)
- 1st Diagnosis:
- Age at DX: 24 years old
- Symptoms:
- Bruising
- Tiredness, shortness of breath
- Itching
- Tests for DX:
- Blood tests
- Bone marrow biopsy
- Treatment
- 2 stem cell transplants
- IV Chemo
- Targeted therapy (Xospata)
- How I Got Diagnosed
- Going Through AML Treatment
- Video (Part 2)
- What made you change hospitals?
- How did you decide which treatment to take?
- What did you get for your chemo infusions?
- Describe the bone marrow biopsy
- Describe your chemotherapy and side effects
- Tips on dealing with a long hospital stay
- What helped reduce the side effects?
- What helped gain back some weight?
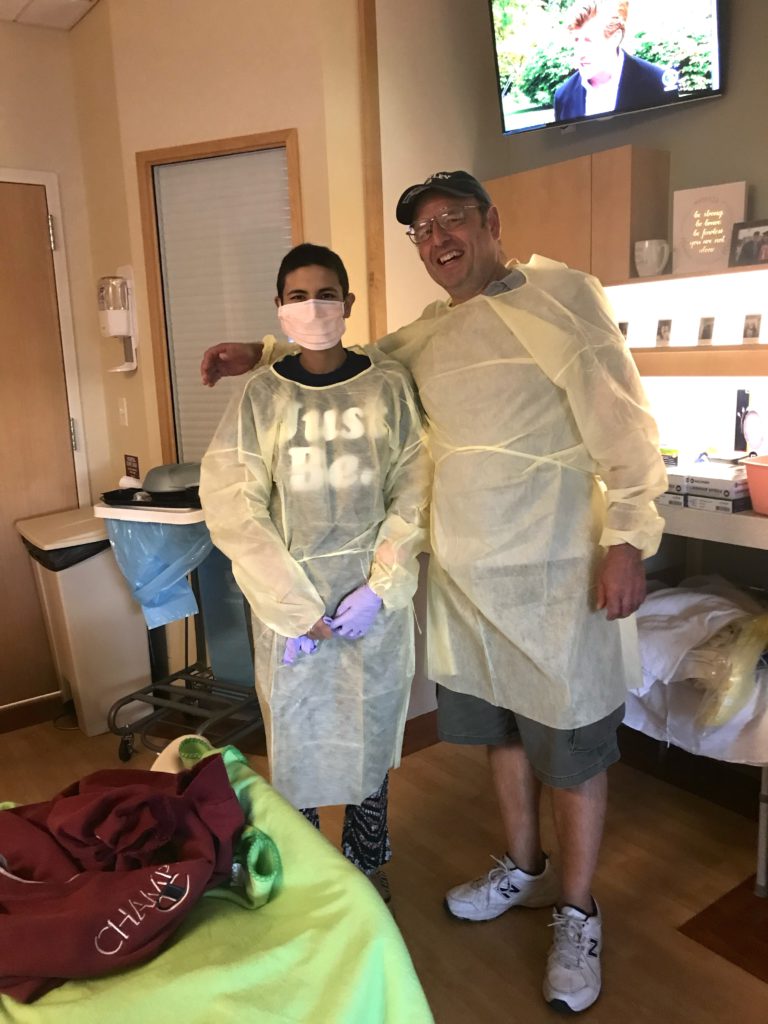
- The 1st stem cell transplant
- The medications taken post-transplant
- Describe the follow-up routine
- Managing anxiety before each bone marrow biopsy
- Relapse and Treatment
- Video (Part 3)
- Symptoms of the relapse
- Processing news of the relapse
- The benefits of meditation
- Describe your relapse treatment plan
- Differences between 1st and 2nd stem cell transplant
- More transplant side effects
- What was the radiation like?
- FDA Approval of Xospata (gilteritinib)
- Describe the Xospata and side effects
- Impact of taking a pill instead of getting an infusion
- Survivorship: Life After Diagnosis
- Video (Part 4)
- How to deal with the hair loss
- Deciding whether to stop or continue working
- The experience of being a young cancer patient
- The importance of fertility preservation
- The process of cryopreservation
- Perspectives learned from living with cancer
- The importance of self-advocacy
- Why I share my patient story
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
How I Got Diagnosed
Video (Part 1)
Michele tried to ignore the bruising, tiredness, and shortness of breath.
At 24, she was living an active and healthy lifestyle. Michele enjoyed playing sports and exploring the outdoors with friends, but the persistent bruises and itching prompted her to several doctor’s visits. Her labs eventually revealed she had acute myeloid leukemia (AML).
Here, Michele tells us how she faced and accepted her diagnosis.

About me
I’m from Connecticut. I enjoy just being outside. I love going to the beach, and also I love playing sports. I play basketball and soccer. I just like being active and healthy eating. I love to cook as well.
I recently got very into cooking tofu, which I know is very different. [It’s] something that doesn’t have a lot of flavors, but you can add flavor to it to make it delicious.
My AML symptoms
Throughout high school, even college, I never used to get sick at all. But a couple of months before my diagnosis, I started getting sick.
I had a lot of sore throats. I went to the doctor probably at least 5 times. They just would give me Claritin.

At the time, I’m just hanging out with friends, doing all these activities. I’m overworking myself. I didn’t really think anything of it. But when I look back, all the symptoms were there.
I had shortness of breath. Walking to my car, I’d be out of breath. I went to work one day, and I was there for an hour. I was exhausted, so I ended up going home and just sleeping that afternoon. Then I would get little bruises on my body. I thought I must have run into something, not a big deal, but I was itchy. Separate from the diagnosis, I ended up having scabies. But before I went to get my lab work done, I itched myself so much.
I was bruised all the way down my legs and on my back. That’s when I thought, ‘I need to go to the doctor.’

When I realized how serious this might be
It’s hard, of course, in retrospect. It’s easy to draw the lines and connect the dots afterwards. But at the moment, it’s so easy to explain away every symptom. I think so many of us experience that.
The itching on my legs and the bruising showing everywhere was the ultimate signal. I remember it was the day after my 24th birthday. I went to get my lab work done at Quest. They had it faxed to my doctor, and he said my counts are just completely off.
The white blood cell was 3 times the amount of a normal person, and my hemoglobin was 3 times below in the opposite. I think they don’t normally see the white cell go that high. That part was interesting.
I went to the emergency room that night. They gave me 2 bags of blood. They didn’t really know what was going on. I slept in the emergency room and then went up to a wing in the hospital to stay. They thought I had Lyme disease. They weren’t sure.
A couple of days later, I had a bone marrow biopsy. When the results came back, I got sent up to the hematology wing. Then I got transferred to another hospital to get treatment.
How I got through the “scanxiety”
When I was first diagnosed or when it was first happening, I thought this is minor because I never get sick. Like it’s not going to be a big deal.
When they mentioned Lyme disease, I thought maybe I got bit by a tick or whatnot. But when they did the bone marrow biopsy, I didn’t realize what even the test was for. My thought process is, “I just don’t know what’s going on, but I can’t imagine it’s bad.”
I still do remember him telling me I have leukemia. My mom was there. I didn’t even realize leukemia’s blood cancer. I didn’t know much about it, and it was hard.
The doctor actually treated my grandparents, too, but for a different form of cancer. It’s nice to have familiarity with him. Not that I was around that much, but he treated my loved ones as well.
I remember it as a little superficial. I thought I’m not going to have any hair. When I got moved from the normal wing to the hematology wing, it was just so much nicer.
I didn’t even realize then the impact of having cancer. I was told I had leukemia, but why is this also so much nicer? This probably isn’t a good thing. But my parents were there, and it was so nice to have them.
My mom wanted to sleep there, but I said no because she lives literally a half hour away. I don’t want her to sleep there. They came every day, which is super nice. My other family members came, too.
I also remember texting my friends. I think I was going to see them or something. I had doubts — should I tell them this?
A huge part of being sick for me is knowing the general reaction of people feeling bad, but I don’t want someone to feel bad for me.
I started to tell some of my friends, and they were super great about it.
When I was transferred to Yale to get better care, that’s when it became really hard. It’s far away from where I live, but my parents came to see me every day. Just the shock of it. I’m 24 years old, and I’ve never gotten sick. I can’t believe this is happening to me.

How my doctor broke the news
They were super supportive.
I remember there were residents or fellows around me, and then the doctor eased into it. She grabbed my hand and asked if I want to call my mom or anything. I said yes.
One of the residents around my age took my hand when I started crying and stayed with me. She was super sympathetic. We chatted about other subjects just to get my mind off things, too.
How can you tell someone something so hard? But his approach and having those people around me definitely made me feel comforted.
Recalling the moment of my diagnosis
I’m very much comfortable now with my diagnosis.
Thinking about it brings up the memories of what I had to go through or what I had to put my parents through. That’s the hardest part.
Back to telling new people, sometimes I have a tough time. That’s something I struggle with even today, just because I don’t want people to pity me.

Breaking the news to family and friends
Definitely in strides. It’s obviously a super heavy conversation to have.
My parents were the first ones to find out, and I had them tell my family. I was just so emotional even just to send the text that I was diagnosed. I only texted a handful of my friends. Others, I didn’t actually tell.
But they’d understand that I’m not responding back for days because I’m going through treatment, or I just can’t talk on the phone all the time because I was really tired.
I think taking it in strides and segmenting out my work friends, my family, and then having them tell each other so I don’t have to feel the need to tell everyone about my diagnosis.
Later on, as the weeks progressed, I felt more comfortable, and some came to visit me.
During the first week back, I texted my home friends who live around the area, and I told them it’s fine to tell everyone else. Some of them also came and visited me in the hospital.
It just made me happy. They were so supportive.

I do remember times when I would have 20 text messages on my phone. It almost felt like people feel the need to reach out to you even more, and it gets even more overwhelming.
It’s like a 2-sided stone. You have the benefits of feeling so much love, having everyone text me. But then again, I couldn’t respond at the moment.
I know they all care. It really does show you who really cares about you and who loves you. You are supported by a great family, set of friends, support system. It meant everything to me.
What is AML?
I didn’t even really know what type of cancer and leukemia. When they told me about it, they’re still doing tests.
There are different subtypes, different mutations. All that medical jargon, they went over and explained to me. They also talked about what could happen in the future. For example, fertility is a huge issue with chemo.
They talked about transplants, because not everyone who has AML gets a transplant. I also remembered them explaining maybe it was genetic for me.
I wanted more information, too. I thought it was extremely helpful just to understand.
None of my parents and grandparents have leukemia or blood cancer, but other cancers. The doctor described it as it’s almost like a car crash — you won’t know if it’s going to happen.
It was also helpful for your family to hear it right. I think one of the most emotional parts for me when I was getting diagnosed was seeing my dad get emotional wondering that very question: Was it because of the genes that my parents gave me?
Going Through AML Treatment
Video (Part 2)
Her life turned upside down, but Michele bravely faced AML treatments.
The IV chemo, stem cell transplant, and dozens of pills in her daily pillbox brought devastating side effects to Michele — physically, mentally and emotionally. However, she consistently and presently went through it all.
Michele tells us how AML treatment affected her.
What made you change hospitals?
It was the cryopreservation surgery. The hospital I got diagnosed with was a Catholic hospital, and they don’t do fertility preservation. I ended up going to Yale.
»MORE:Fertility preservation and cancer treatment

How did you decide which treatment to take?
As the thing about AML or any form of leukemia, as tests come up, the treatment differs.
What to expect next was definitely a question eating at me, because it was very uncertain.
The doctors would do rounds. During the first day I was hospitalized, I had 4 different people come in to greet me.
I got there at 7:00 p.m. I’d have 4 doctors in the next 2 hours, and then I went to bed. A lot of information was thrown at me, too.
That part, even though I do like knowing technicalities, was really a lot of information and definitely overwhelming.
I kept a notebook and would write everything down, any questions that I thought of during the day that I’d want to ask the doctor. My mom is in the medical field. Her boss, which is also a close family friend, would ask all the medical questions. It was a comfort for me to have that extra resource there.
I would ask even the nurses lots of questions. Since you see the same nurses, while you only see the doctor once a day unless something’s happening, it’s helpful to talk to them. The nurses were there for me the whole time, too, communication-wise — another line of support in general.
The hospital had a whiteboard. Since a big part of leukemia are blood counts, they would write my counts up there, too.
Definitely, there’s a lot of information and hard to organize, but having a nurse or being able to talk to someone you’re comfortable with — for me, it was my mom — helps.
That was like an affirmation that was I going through treatment.
What did you get for your chemo infusions?
I got a Hickman and a central line, as they would call it. I definitely had IVs in my arm before they put the line in. The hard part about this is I’m a tough stick, as they call it. You can probably still see a little bit of bruising or discoloration.
For treatment in general, it’s necessary to have it. They’re doing labs every day, almost round the clock, especially at first.
Until the Hickman is put in, you’re getting poked all the time, which takes up the veins as well.
That was probably one of the first procedures for major treatment event for me, aside from the bone marrow biopsy, which was a little scary, too.
Describe the bone marrow biopsy
I remember the first time because this was the scariest time especially.
At the hospital where I was originally diagnosed, they used something like a drill. That was the only time they ever used a drill. I remember the sound of it and my hands getting clammy. Honestly, it wasn’t that bad.
That time, I did have shooting pain down my leg, but all the other times no. Perhaps it’s the nervous reaction. Not from seeing the needle, but because the needle is huge, and they’re drilling a hole there.

The whole process is kind of nerve-wracking.
The residents were all there, too. I remember them being super supportive again, which made me feel nice.
Then when I got transferred to Yale, they had to do another bone marrow biopsy because it was a different hospital. It’s just been a week, and I had another one, so again, a nervous feeling. Now I’m very used to them.
I was trying so hard mentally to transport myself somewhere else. As it’s happening, I remember my then-fiancé asking me if I want a video or a photo. I said I don’t ever want to see what’s going on back there.

Describe your chemotherapy and side effects
For my first round of chemotherapy, it was 7+3 of cytarabine. It’s 7 days of 24-hour infusion. Then in the first 3 days, I have to take in another push drug.
Having a bag of chemo drugs carried around with me in the shower was just annoying. Then 2 weeks after that, they do another bone marrow.
That’s when they made the decision to do another round of chemo because it was greater than 5%.
I had 5+2 of the same drugs — 5 days, 24-hour infusion, and in the first 2 days are a push drug. Then they do another bone marrow maybe a week or 2 after the 5+2, and then it was under 5%. That whole time, I was down at Yale for 2 months.
It was definitely a long time. I didn’t get side effects until a week later because it just takes time for it to kick in.
The place was nice. They had a healing garden, which I loved to go to when I could manage. Some of my friends were able to take the train in, which is super nice of them. My parents came every day. I definitely had the support system while being down there.

I did make a friend, too. Most people with my diagnosis are white male, age 60+. Obviously, being biracial and being young and female doesn’t hit any of those categories. When I was down there about a month in, I met another girl who was just about 18. We would go on walks together. We’re going through the same treatment. She’s still a friend today
It was nice to go through something together and ask those kinds of questions that I didn’t know anyone else around my age asks. Like, why me?
It was a huge emotional impact on me, and having someone else around the same age group gave me a little more affirmation. It was nice to make a friend.
Tips on dealing with a long hospital stay
I would definitely go on to the wing itself. I would go on walks a lot. I’d do laps. I believe physical health does help mentally as well. The little walks help, too. It’s just nice to be outside and get some fresh air. They have little trees and a little waterfall in the garden.
Then I would wave if there are other people walking, or the nurses would talk to me.
I remember the royal wedding was happening when I was diagnosed, and one of my nurses said, “I’m only going to do this for a couple of minutes.” Then I said, “Stay and watch the royal wedding with me!” She stayed for a little.
I made really good friends with nurses. That definitely helps pass the time and helps emotionally as well.

I was in the hospital during COVID as well, so I did experience the difference between my first stay and second. There was a point when I was allowed no visitors at all. I would try to entertain myself, so I gained a lot of hobbies.
Before diagnosis, I knit a little, but after diagnosis, I knit a lot. I also watched lots of movies with great recommendations from friends. I still have a huge list today. I enjoy reading now, too. Puzzles were a huge one, too. Fun activities, too, just to keep my mind busy and have a little fun in it.
It’s really finding those little things that will make you happy.
»MORE: Mental and emotional support when leaving the hospital

What helped reduce the side effects?
Probably the worst ones were nausea. I can’t keep anything down. The chemo is just so intensive. There are medications that help alleviate it, like Zofran. The others are push drugs so that they react faster. But the nurses are great. You can just ring your call bell, and they’ll come.
Another worse side effect was feeling really tired. People are trying to visit, but I’m just so tired. My parents and friends would just then talk to each other.
Then the third one would be strength. The second time after my relapse and coming out of the hospital, I just couldn’t even walk. I was in bed all day.
I tried to be as active as possible, but my body mass decreased so much. I was not eating, and that’s a big one.
There are days when I’ve tried so hard to eat, but there are days I just couldn’t eat anything. I would try to take supplements. It’s crazy how little you can eat, and yet you’re throwing up. Even if you try to eat something, you just throw it up.
My parents would say, “Michele, just eat. Please, just another bite.”
All of that








