Jason’s Stage 2A Classical Hodgkin’s Lymphoma Story
Jason F., Hodgkin’s Lymphoma, Stage 2A
Symptoms: Itchy legs, bloated face and “upper trunk,” slow-healing wounds, asthma worsened
Treatments: Chemotherapy, radiation
Jason’s Stage 2A Classical Hodgkin’s Lymphoma Story
Jason shares his stage 2 Hodgkin’s lymphoma story and details of his treatment: ABVD chemotherapy and radiation therapy. Jason also highlights the importance of self-advocacy and taking care of mental health.
- Name: Jason F.
- Diagnosis (DX)
- Hodgkin’s lymphoma
- Stage 2A
- Age at DX: 39 years old
- 1st Symptoms
- Shortness of breath (already asthmatic)
- Itchiness on leg
- Feeling generally unwell
- Treatment
- ABVD Chemotherapy
- 6 cycles, 2 per cycle, 12 total infusions (outpatient)
- Radiation therapy
- 18 sessions
- ABVD Chemotherapy

- Video: Jason on How He Got Diagnosed
- 1st Symptoms, Scans and Tests
- What were your 1st symptoms?
- Your breathing test came back fine
- Describe the sudden symptoms changes that forced you to go to the ER
- What happened at the ER?
- Processing the possibility of cancer
- Spending the days waiting in the hospital “hallway medicine”
- How would you rate pain tolerance?
- Describe the biopsy
- Describe the ultrasound
- How were the scans?
- Describe the CT scan
- Describe the PET scan
- How did you pass the time in the hospital stay?
- What was the hardest point during this time?
- How did you tell your kids about the cancer?
- How old were your kids at the time?
- How did you process the cancer diagnosis?
- What were the first treatment decisions?
- Did you break the news to loved ones?
- Video: ABVD Chemotherapy & Radiation
- ABVD Chemotherapy & Side Effects
- How did the oncologist describe your treatment plan?
- Warning: you may get sick of your favorite foods
- Chemo nurses helped prep you for treatment
- Describe the ABVD chemo infusions
- Did you get a port or PICC line?
- Did you like the PICC line?
- How did you maneuver with the PICC line?
- Describe the ABVD chemo side effects
- What helped combat some of the side effects?
- Describe the hair loss
- Describe experiencing the bleomycin lung toxicity
- When did you learn you had no evidence of disease (NED)?
- Radiation Therapy
- Video: Jason's on Navigating Life with Cancer
- Reflections: Navigating Life with Cancer
- Being your own advocate as a patient
- How has it been dealing with survivorship?
- The physical recovery was easier than the mental health
- How did you move forward with your mental health?
- How did cancer impact your relationships?
- Your mom was diagnosed with lung cancer shortly after your diagnosis
- How did you process the grief as you went through treatment?
- Last message to other people dealing with cancer
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
I feel better than ever in some ways. Going through what I went through definitely put me on a journey to make sure my health is always now my number one priority in life.
Jason F.
Video: Jason on How He Got Diagnosed
1st Symptoms, Scans and Tests

What were your 1st symptoms?
It seems like a lifetime ago to look at that picture. It was on a family trip in the Bahamas with my then-wife and kids. I felt generally unwell. I had injured myself, scraped myself getting out of the pool, and it took about a month to heal.
It didn’t feel or seem right, not like anything I’d ever experienced before. Even in the way that it healed didn’t seem right.
I’ve always been a sufferer of asthma my whole life. During that time, I also noticed my breathing was getting worse. I’ve always been on inhalers and have always had to make sure I have my rescue inhaler with me in case of flare ups.
When we got back after New Year’s, for about 3 or 4 months, there was an intense itching on my legs.
It was to the point where I probably spent $200 or $300 on various types of creams to figure out what I could do to stop the itching. Nothing would stop the itching!
I chalked it up to my house being dry in winter, and I was in Toronto. The winters can be very dry and cold. I didn’t think anything of it. That’s the thing. It’s not something you’d piece together and think, “Okay, I’m suffering from something.”
In fact, in May I actually had a full breathing test done. It looked like my asthma was getting a little bit worse, so they increased the dosage on my inhaler.
Your breathing test came back fine
The day before I went to the ER, I was sitting in my office with my partner and laughing because I had just gotten the test results back from my breathing test. I said, “I guess everything’s fine.”
It was funny that that was the day before everything changed.
Describe the sudden symptoms changes that forced you to go to the ER
I was out for dinner with my son and a close friend. That was the night before the ER trip. We had a great time; we were joking. We walked back home, and I was swinging my son around. I didn’t notice anything.
I woke up the next day and realized that my chest, arm and face areas were all really swollen. When I say my arm was swollen, it was the size of Popeye’s arm. It was massive, 3 or 4 times the normal size of my arm.
Also, my skin was blue and tight. It felt like my skin was going to explode. First thought I had was that I had a blood clot or something wrong because the blood was pooling. I took a shower and then went to the hospital.
What happened at the ER?
That would have been around 6 or 7 in the morning when I got to the hospital. I was in the emergency room all day while they performed various tests.
They started with an ultrasound of my chest as the first test. Throughout the day, I’m not really getting any information. I remember they tried to take blood out of my swollen arm.
When I say my arm was so big, it felt like it would have popped if you put a pin into it. It was so stretched. They kept trying and trying. Finally they took blood out of my other arm.
Around 3 or 4 in the afternoon, they sent me for a CT scan. Then I got wheeled back into one of the emergency rooms again with the curtains drawn.
I noticed 3 or 4 doctors and some nurses standing nearby, looking at a screen. I didn’t know if the images were mine, but it looked like an upper chest area, so I assumed it was.
It was probably 7 at night by the time someone came over to talk to me. I was lying in the bed by myself, obviously with my mind going in a million different directions. I remember them saying, “We found a pretty substantial 10-centimeter mass in your chest.”
I didn’t know what that meant. I didn’t know if it was in my lungs, chest, where? I thought my life was over. It was the biggest gut punch I’ve ever had in my life.
Processing the possibility of cancer
One of the weird things is — and I’ve talked to another cancer survivor about this — at various points in my life, I always expected I would get cancer. I’m a bit of a worrywart and a bit of a hypochondriac. I can thank my mom for that.
I was lying there in the hospital saying, “This is it. This is what you expected would happen. Your life is over.” I’m a father of 2 children, who mean everything to me. All I could think about was them — not myself, just my children.
Spending the days waiting in the hospital “hallway medicine”
Because my arm and my face were so swollen and there was fear of a blood clot, which was there, I was at 11 at night wheeled up into the internal medicine department. They didn’t have a diagnosis for me in the hospital yet.
I spent the first 2 days there. Canada has great healthcare. It’s free. I didn’t pay a single cent for my treatment, but I spent the first 2 days in the hallway.
You can research hallway medicine and how it’s been a problem in Canada just because of the overcrowding. So I was in a hallway of the internal medicine department.
It was a bit of a nerve-wracking experience in itself, because there were a lot of older people who had had strokes and events like that, as well as mental health issues. There wasn’t a moment of peace. There was no privacy.
My wife had come to visit me. I don’t think anyone else came, including my kids. I was in the hospital for 13 days, from June 1 to June 13th. That was a rough time.
How would you rate pain tolerance?
Extremely high. I’m covered in tattoos; I have no problem with needles. I also had my hip replaced after my cancer experience, so I was already battling some pretty large pain at that time. I’m not a fan of taking any kind of pain management, so I just deal with it.
Describe the biopsy
Next day in the hospital, I had the biopsy. The pain wasn’t great, a 7 out of 10. It was maybe an hour of dealing with the uncomfortable procedure.
It felt like a meat skewer being stuck through my chest about 12 times and cutting little pieces out. They did it with a scan, and they put a sort of paper on my chest. They would scan me through and take tissue samples.
The problem was it took quite a while to get the diagnosis. That’s why I was in the hospital for so long.

Describe the ultrasound
The ultrasound is actually nice because there’s a gliding gel they slide over you, so it doesn’t feel like you’re enclosed in anything. They rub the gel on your chest, and that’s that. They press down a little bit, but there’s no real pain.
How were the scans?
The scans didn’t scare me. I think I was in a whirlwind of everything happening so fast and trying to understand what was going on. I feel like that’s the thing.
When you’re in it, it’s a lot different than when you step back and think about everything you went through. You just get into this mode of, ‘I’ve got to do this.’
You’re just surviving at that time.
Describe the CT scan
The CT scan is different. If you’re claustrophobic, that may be an issue, but it’s more lying flat and being moved back and forth automatically through the machine. I didn’t find that that big of a deal.
Describe the PET scan
There was a very weird feeling with one of the injections (the contrast dye) that they give you for your PET scan. The guy was younger. He warned me that it would make me feel like I peed myself, but not to worry. I wouldn’t pee myself.
He ran me through the scan, and sure enough, I felt like I had peed in my pants. I didn’t, but it’s a weird feeling you get. There’s also that metal taste you get in the mouth.
But again, there’s no real pain. It’s just obviously a little bit uncomfortable going through all of that. Short of the biopsy, that was the only real pain I felt.
How did you pass the time in the hospital stay?
I have always had a rule in life to never look online. Don’t self-diagnose. Trust me on that. I never did. The only time I looked online for the entire 2 weeks I was at the hospital was once I got my diagnosis. That’s only when I first researched.
There was a toss-up if I had non-Hodgkin’s or Hodgkin’s lymphoma, large B-cell, and they thought I might have that. I knew that was bad and it was worse than Hodgkin’s lymphoma.
I didn’t want to put myself in a situation where I was getting anything else in my head. I was stressed out enough as it was and scared out of my mind, so I didn’t look online.
I eventually got my own private room and was as comfortable as I could be, keeping in mind that I was also dealing with my arm. I couldn’t lift my arm above my head. It felt like it was 900 pounds. I’m feeling swollen, scared and many different emotions. The stay itself wasn’t bad.
What was the hardest point during this time?
I’ll preface this by saying I’m an emotional guy, so if you see tears during this interview, that’s who I am. I’m okay.
Something that haunts me to this day is the look my kids would give me every time they were at the hospital and were going to leave. The look they gave me each time haunts me to this day. Just thinking about my kids wondering if they’d see their dad again was not something a child should go through.
I know a lot of people say, “Oh, your kids will be tougher and grow stronger from this.” They didn’t need to go through this. Their innocence was robbed by having one of their parents possibly die.
For the period of time I was in the hospital without a diagnosis, that’s what made it really painful and caused all the damage that it has.
I have such a crazy bond with my kids, and having to go through that, I can’t say enough how grateful I am to have them. We still are picking up the pieces of the family from the fallout from that. There’s very much PTSD in some way.
»MORE: Read different experiences of a cancer diagnosis and treatment
How did you tell your kids about the cancer?
I can’t necessarily say what worked for me will work for everyone, but I’ve always been very open with my children. I’ve never sugarcoated anything.
I talk to my kids like they’re adults. I don’t baby my kids. We have a friendship, as well as me being their dad. I’m still their friend as well.

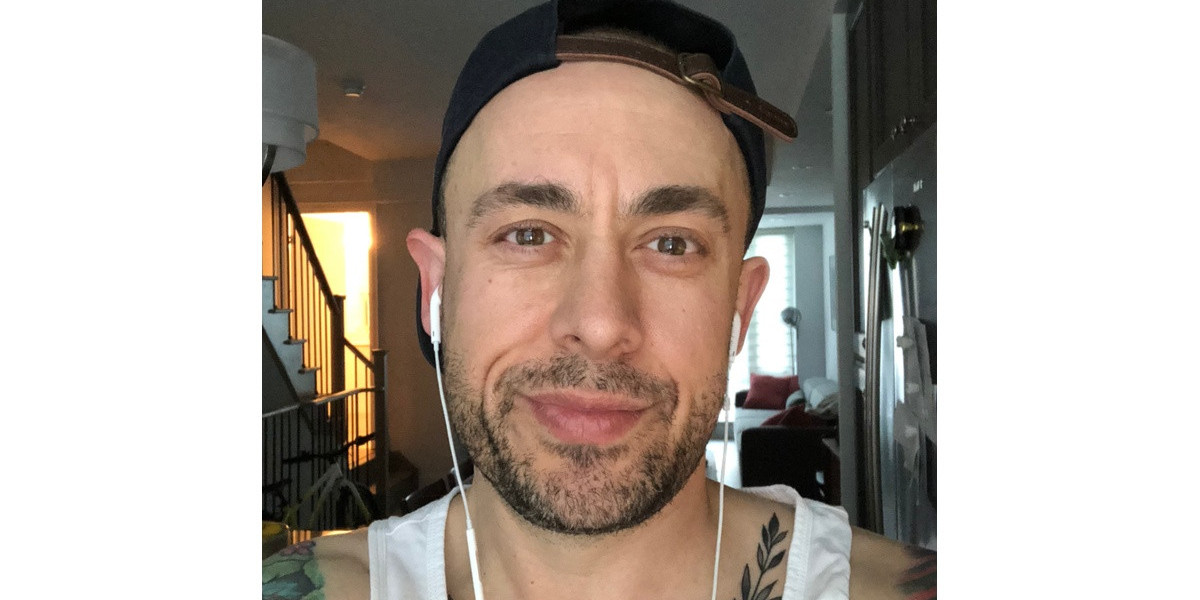
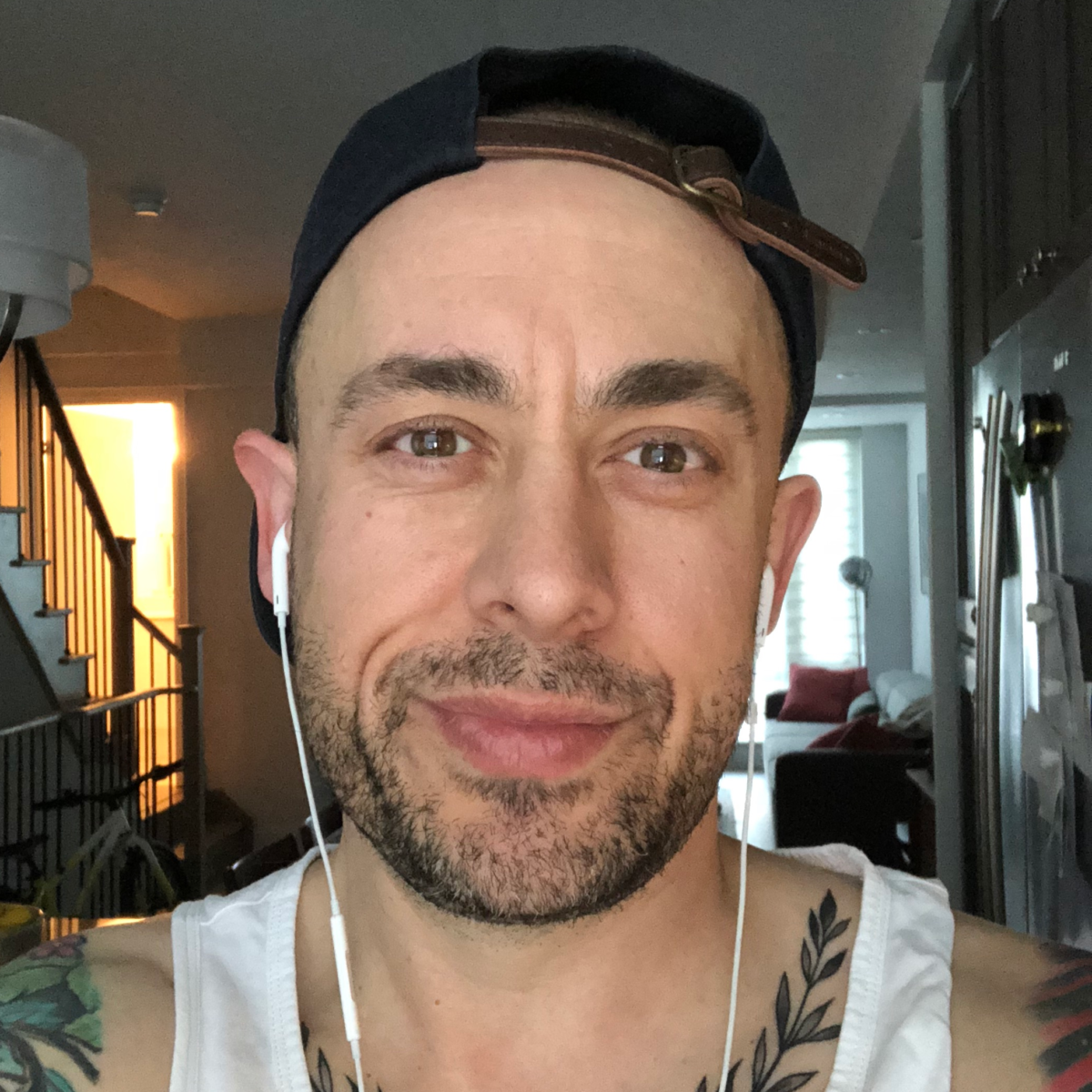
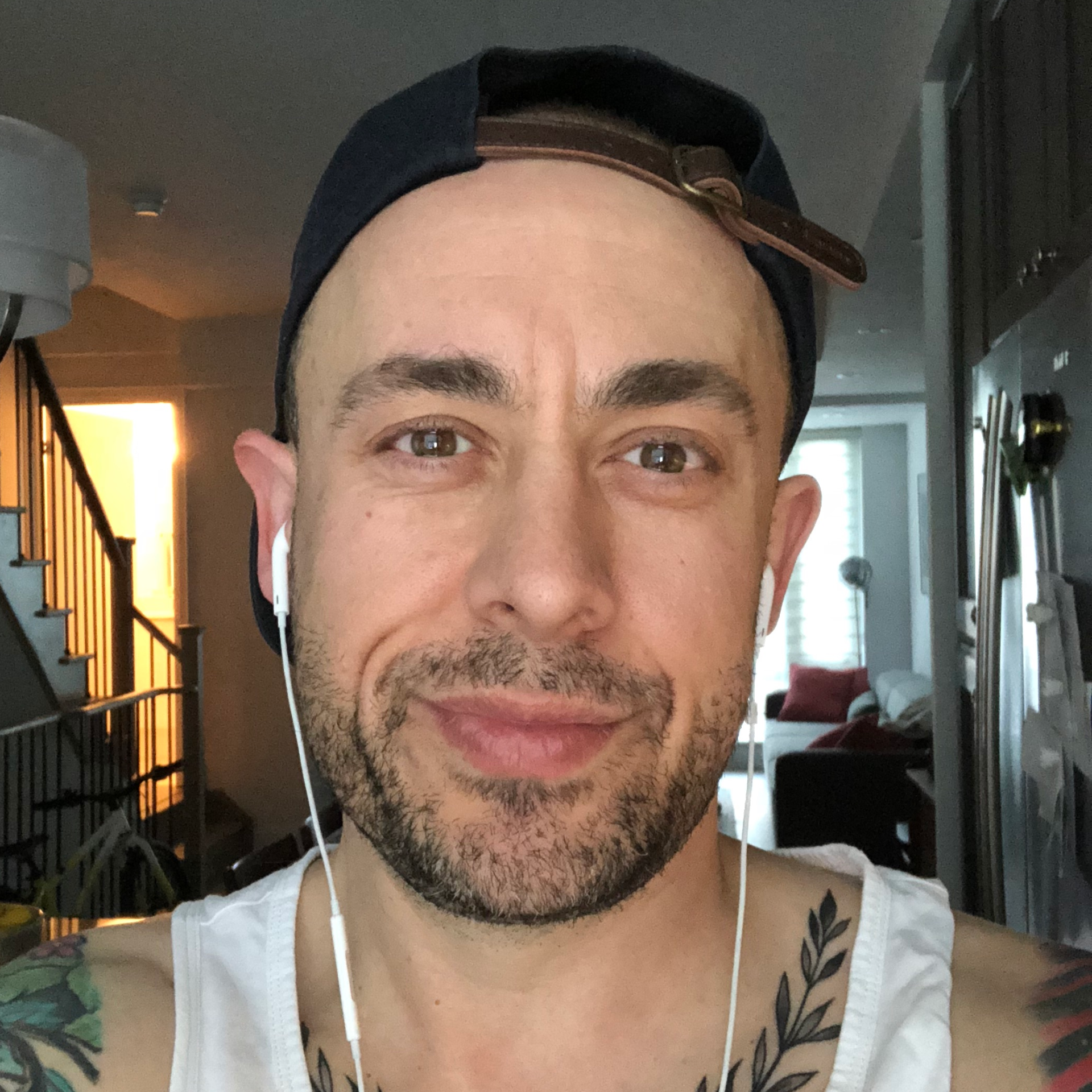
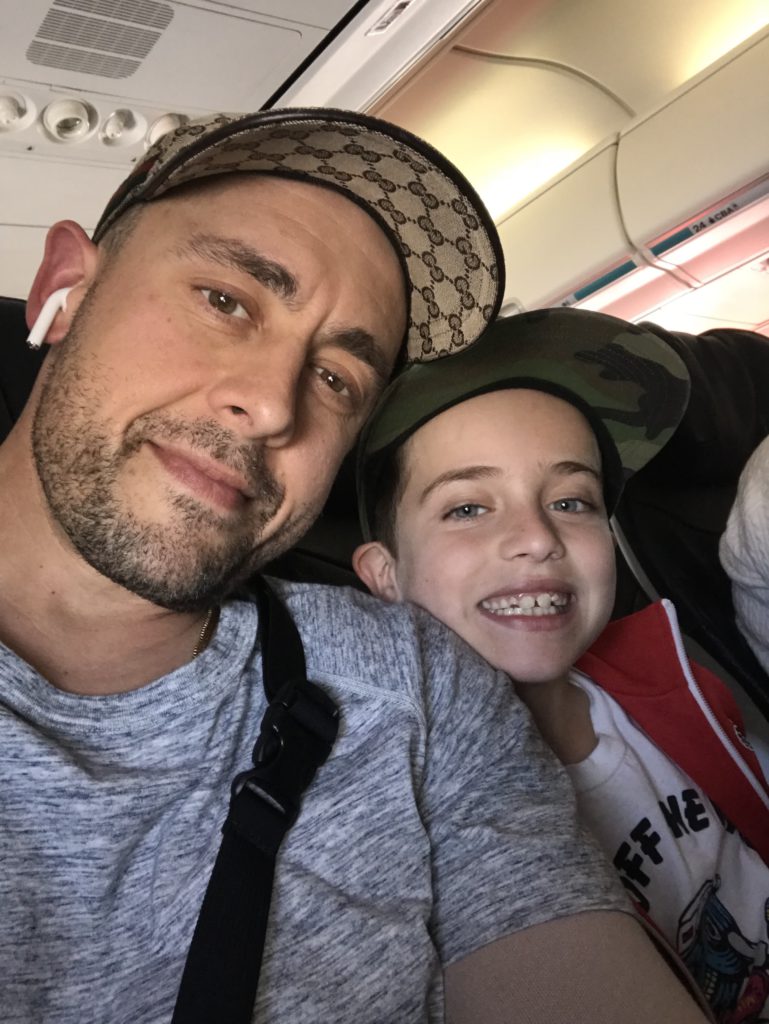
In this picture, you can still see the bloating of my face from the prednisone (steroids). I can’t say enough about these two. They were the sole reason I wanted to get better from all this. It was for the two of them.
I don’t know if there’s a right or wrong answer. I think from my perspective, with Hodgkin’s lymphoma you have such a high survival rate. I wanted to be open. They needed to know why I was in the hospital. They didn’t need to have to worry about anything anymore.
Once we had the diagnosis, I was fairly open with them on what was going to happen and what the treatment plan was, and that I was expected to get better and was going to beat this.
How old were your kids at the time?
My son was 7, and my daughter was 12 or 13. I had to remain tough as much as I could for my kids. I’m fortunate I have a great group of friends around me I was able to lean on.
Frankly, there were quite a few nights I cried myself to sleep in the hospital. I’m going to be honest about that. I was finally, for once in my life, not in the driver’s seat or in control of my life. That was a weird feeling.
How did you process the cancer diagnosis?
I didn’t look online, so I wasn’t as well-versed about the different type of Hodgkin’s. I knew the non-Hodgkin’s sounded worse. When I heard the news of the diagnosis, I’m a person who likes to research and understand. I was emotional but not surprised.
I knew I had cancer, so in some way, it wasn’t like, “You have cancer. Oh my god.” It was more like, “Okay, so this is the type of cancer I have.”
»MORE: Patients share how they processed a cancer diagnosis
What were the first treatment decisions?
I was taken from internal medicine to the cancer center that’s attached to the hospital. We’re very fortunate in Canada. In Toronto, there are two of the top cancer centers in the world, the Sunnybrook-Odette Cancer Centre and Princess Margaret Cancer Centre, which are two leading research hospitals. I was at Sunnybrook-Odette. Sunnybrook is the name of the larger hospital, and Odette is the name of the cancer center.
I was wheeled over to my hematologist, and she gave me the facts. I came out of that appointment with a simple, “All right, we know what we have to do to get this done.”
It was a sense of relief that now I had regained a little bit of the control. I knew what I needed to do. I was diagnosed. I had an 85% chance of survival. In my head, I was like, ‘You have to screw this up! Your odds are great. You’re going to get through this.’
That’s the only thought I had from that point on. I knew it’d be a bad, rough road, but I also knew there was going to be a light at the end of the tunnel.

Did you break the news to loved ones?
Anyone who mattered to me knew about the cancer diagnosis, including my friends and my family. I’m very close. I have a huge group of friends. I’m close with my family. Everyone close to me knew.
I was very open about that. I felt by putting it out in the open, it made me feel better. It kicked the elephant out of the room. Maybe it’s just something with having any level of control, but I controlled the narrative about what was going on. I shared information regularly with people, highs and lows.
I had several people who visited me in the hospital when I was here for the initial 2-week period. I shared everything with everyone.
There’s a lot of sitting and waiting around in the hospital. I can type pretty fast, so I was in communication with everyone on a regular basis.
»MORE: Breaking the news of a diagnosis to loved ones
Video: ABVD Chemotherapy & Radiation
ABVD Chemotherapy & Side Effects
How did the oncologist describe your treatment plan?
We talked more about the prognosis and how everything would work. I don’t think I got that great of detail about the chemotherapy treatments.
I think the pharmacist who was brought in gave me more of an update. They talked about the various medications I’d have to take and how they’d work for me. It was a bit of a surprise.
Warning: you may get sick of your favorite foods
The day before you go for your first chemo, don’t eat any food that you will ever want to eat ever again in your life.
There’s a certain restaurant in my hometown I loved. On Sunday night (before going to treatment), my friends picked me up for a bite to eat. The smell of that food, to this day I think I could probably get sick if I walked by and smelled that restaurant.
I know everyone wants to bring little snacks. If there’s something you enjoy eating and have for a long time, have your first chemo and maybe not bring that food around, just to make sure you don’t have an adverse reaction.
I’ve heard it’s similar to the way some women crave certain foods or don’t like certain foods when they’re pregnant. You could end up ruining certain types of foods for yourself, permanently.
Chemo nurses helped prep you for treatment
The doctor gave me a breakdown of the treatment. She didn’t really talk about how I would feel going through it. The chemo nurses did that at the hospital when I started treatment. They did a good job of explaining further details. I learned the most about the process from them because they were definitely more hands-on with that.
I’m young, and I like to chat. I try to have a positive attitude, so I developed a great relationship with the nurses. Every time I see them for follow-ups, I get a giant hug from them.
They remember me, and I remember everything about them. They were with me at some of my darkest times in my life. They’ll always have a piece of my heart.
Describe the ABVD chemo infusions
It was outpatient, so I’d usually have my chemo on Monday. On Friday before, I’d have to go up and get my blood work done just to make sure my levels were strong enough for me to be able to take the chemo. Then I’d usually be there 3 to 4 hours.
The weird part about it is this is supposed to cure you and make you better, but when they’re wearing rubber gloves and hazmat suits and can’t get a drop on you or them, it feels nerve-wracking. It’s a little scary.
I own my own business, and part of coming through the other side of this is that I realized how I needed to take a break and appreciate things in life, versus being a workaholic.
I was still working when I was getting chemo. I was working for the 2 weeks I was in the hospital, still not knowing what was going on with me. It was in my nature, unfortunately.
I’d just bring my iPad, and a lot of times I’d have friends who’d come sit with me. It wasn’t the worst. I developed some great contacts with people who were also sitting in the chairs. Each room in our hospital would have 4 chairs for infusions.
You just talk. You’re there for that long; you’re all fighting the same battle. I developed a great friendship with one guy who was having treatment with me.
You’re part of this group. Cancer impacts everyone. It doesn’t matter who you are, how much money you make, how old you are. Everyone can be impacted by cancer. It’s the most random group of people who are put together here.
It doesn’t matter what walk of life you come from. I’ve met all different types of people. Because I like talking, it helped pass the time talking to people.
»MORE: Read our comprehensive ABVD chemotherapy info page
Did you get a port or PICC line?
I was having problems with my veins. I didn’t have a PICC line until after the fourth chemo infusion, so a third of the way through I had one put in.
My veins were really hurting. I was getting a lot of pain in both my hands. I guess they couldn’t really find my veins in my arms, so they had to do it through my hands. It was starting to be really painful. I was bruising pretty badly.
I had a PICC line in, and the last treatment I went for, number 12, it was a new nurse. She pulled out the PICC line. I ended up having to get it done by IV again.
You can feel different temperatures of the drugs through the PICC line. It’s like they’re floating through. You can feel it from all the different drugs — A, B, V and D.
»MORE: Read patient PICC line experiences
Did you like the PICC line?
Getting needles is something that doesn’t bother me. I have no problems with them. With the PICC line, I had no problem with it. I did find it a little annoying. It was nice going through chemo not to get poked a bunch of times!
I found it was a bit of an inconvenience. It sped up getting the chemo every time, knocking a little bit of time off. It was just part of the process. It was all part of moving forward and getting better. So a bit annoying, but not the end of the world.
How did you maneuver with the PICC line?
An arm out the shower sometimes. I’d hang it out or put saran wrap around it. There are also full things you can get. I tried to tape one to my body. It was a million different things.

Describe the ABVD chemo side effects
Summary: Bloated/weight gain (steroids), constipated, fatigue, dry eyes (no eyelashes), runny nose (no nose hairs)
The prednisone kicked my butt. My entire body was completely bloated. Even in this picture, my face is bloated. I’m still dealing with the blood clot and some of the side effects. It’s funny to look at that picture. I don’t really see myself in that anymore.
Looking back at some of these old pictures bring back memories that, in large part, I’ve moved on from in my life. I think you walk out of the hospital feeling fine that first day. You feel a little spacey, almost like an out-of-body experience. It was a weird feeling.
I’m always amazed, and I appreciate when people are like, ‘I’m back at the gym or going for a jog.’ I was not getting out of bed at all. I was not getting out of bed.
There was the prednisone and then the medication and pills that then make you feel constipated, not great. The first couple of days I was home after the infusion, I was toxic.
That meant I had to use the restroom downstairs. When I brushed my teeth, I had to be careful I didn’t get my toothpaste anywhere, and I couldn’t kiss my kids or my wife.
I couldn’t do anything. I felt like I was toxic, which I was, but it was a weird feeling not to be able to hug my kids or anything like that.
I didn’t get any mouth sores. What I found was when I started to lose the hair on my body, my eyes got really dry and my nose wouldn’t stop running.
You’d be surprised how important nose hair is, actually, until you don’t have it. It can be difficult to not have nose hairs, that’s for sure.
Some of the other medication that I was on had other impacts on my body. I was on 2 really strong antibiotics for a while. They don’t just kill the infection; they kill all the good bacteria in your belly, too. It really messes with you and your digestive system. I’m not a big fan of antibiotics unless they absolutely need to be taken.
»MORE: Cancer patients share their treatment side effects
What helped combat some of the side effects?
Before I left the hospital, I started to make sure I took stool softeners. You have to be proactive and figure out what works best for your body, but I don’t think keeping yourself constipated is the position you want to be in. You’re already in an uncomfortable situation. You want to do what you can do.
Describe the hair loss
I didn’t even allow my hair to start falling out. I have a friend who is a hair stylist. The week of my first chemo, after I felt better, I went to his salon, and he shaved my head.
From there, this is my permanent hairstyle now. I know everyone talks about how great their hair grows back and how thick and curly it is. My hair never grew back, so this is my hairstyle for the rest of my life. Thankfully, my head is an okay shape!
»MORE: Dealing with hair loss during cancer treatment