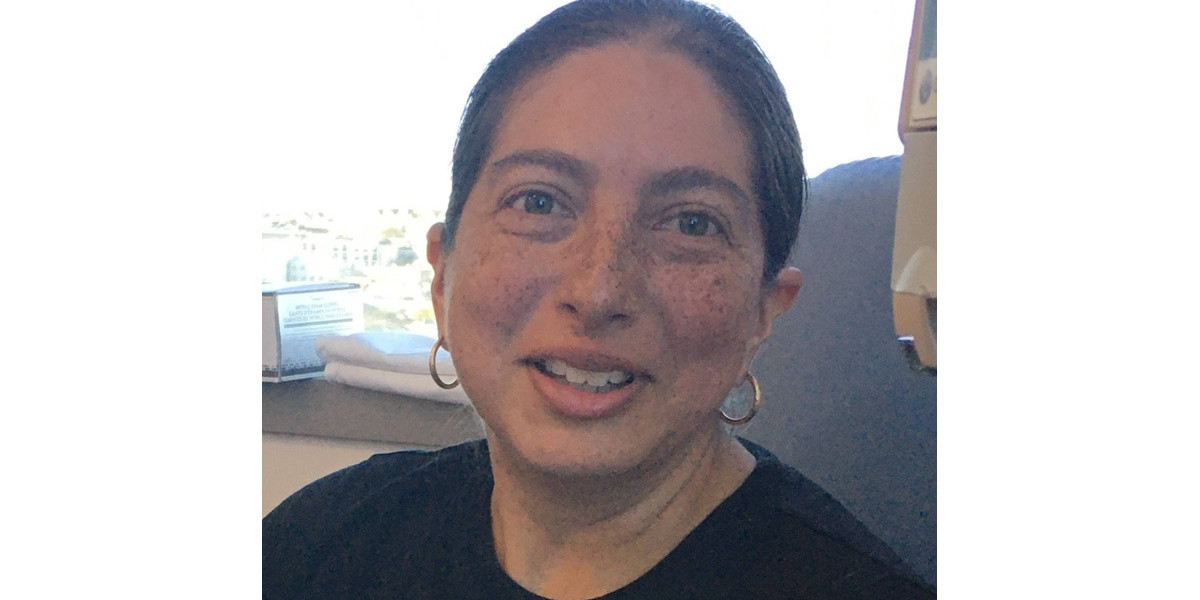
Erica’s Stage 3B Classical Hodgkin’s Lymphoma Story
Cancer details: Staged at 3B
1st Symptoms: Intense itchiness, fatigue, night sweats, weight loss
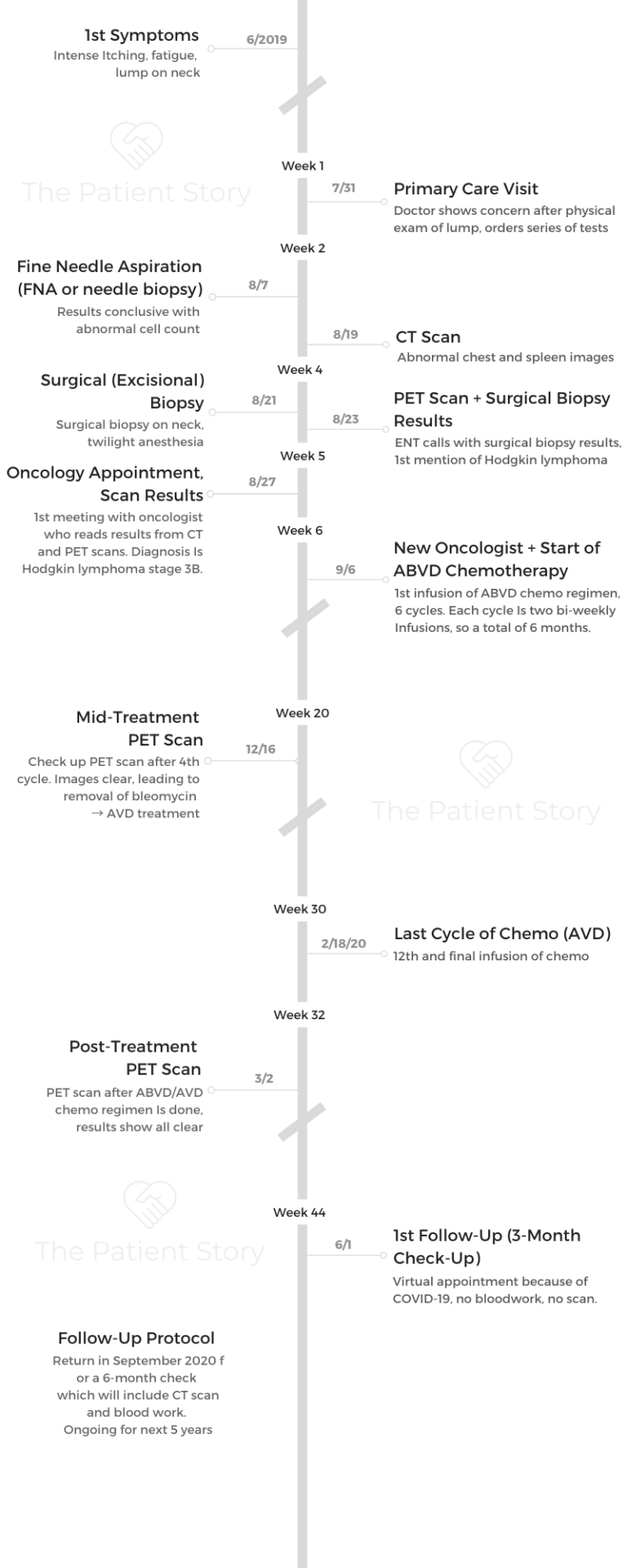
Treatment:ABVD chemotherapy, 6 cycles (12 infusions)
Erica’s Stage 3B Classical Hodgkin’s Lymphoma Story
Erica was 36 when she got her stage 3B Hodgkin lymphoma diagnosis. She details her journey through ABVD chemo and hair loss, dealing with financial toxicity and advocating for herself as a patient.
- Name: Erica H.
- Age when diagnosed: 36
- Diagnosis:
- Hodgkin’s lymphoma
- Stage 3B
- 1st Symptoms:
- Growing lump on side of neck
- Itchiness
- Severe night sweats
- Weight loss
- Tests & Biopsies:
- Needle biopsy (fine needle aspiration, or FNA)
- Excisional biopsy
- CT scan
- PET scan
- Blood work before every treatment
- Treatment:
- ABVD chemotherapy regimen
- 6 cycles
- Each cycle = 1 month, biweekly
- Total: 12 infusions
- 6 cycles
- ABVD chemotherapy regimen
- Tests and Scans
- What were your 1st symptoms?
- What was the series of tests and biopsies you had to undergo?
- Describe the fine needle aspiration (FNA)
- When did you get the FNA results?
- Describe the surgical biopsy procedure
- What were the surgical biopsy results?
- How was the CT scan?
- Warning: you’ll feel like you’re going to the bathroom with the contrast dye!
- How long did it take to get the CT scan results?
- Pushing for the PET scan (self-advocacy)
- Describe the PET scan
- How long did it take to get the PET scan results?
- Diagnosis
- Treatment Decisions
- Chemotherapy
- Quality of Life
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
I know a lot of people I met didn’t want to talk about it, and when they didn’t, it left me feeling isolated. As a result, I just want people to know that people do want to help.
It is a traumatizing experience to think back and live through, but I also found a lot of people who were willing to help.
The community I surrounded myself with, whom I trusted, was also willing to help me find those things when it was hard.
Erica H.

Tests and Scans
What were your 1st symptoms?
Initially, physically, I noticed a change in my neck. My mom had thyroid cancer 2 years ago. She was able to have surgery. She recovered within a couple of months.
When I found a lump right here on my neck, I didn’t worry too quickly. I knew to schedule an appointment, which I did.
Then I talked to my primary doctor, who right away showed some concern and started to schedule me a series of tests.
Initially, it was a physical lump, but after that physical appointment with my doctor, I did start to have more symptoms, some of them a lot more challenging.
The itchiness is one. It was in a sensitive area, where the itchiness just got worse and worse. I started to have severe night sweats, where I lost a lot of sleep and lost a lot of weight because I wasn’t able to eat full meals.
In July, when that physical lump hadn’t worried me, a week after that physical and the few weeks after, I started to experience some of the more severe pain and symptoms.
What was the series of tests and biopsies you had to undergo?
The first appointment happened at the end of July of 2019. Then because she was concerned that it might be something more serious, she scheduled an ultrasound a week after, maybe 5 days after. Then she scheduled the biopsy 2 or 3 weeks later.
All the series of tests took a little over a month, and no one was able to tell me anything. There was the stress of that unknown. It was really starting to preoccupy me and make me much more aware of the symptoms.
I think I tolerate physical symptoms pretty well. The anxiety caused me to get more nervous and feel everything much more intense as I went through the series of tests, waiting for an answer.
I went go get a CT scan, and I had to go get a PET scan. I had to go to an ear, neck and throat doctor, who was a quick moment in time. She was really caring and led me through the biopsy test.
I had a needle biopsy and then a surgical biopsy. She walked me through, but she was such a quick moment that I don’t remember her name.
She’s the one who made the call to me to let me know the results of the surgical biopsy. She said over the phone, “I’m pretty sure it’s cancer, but I’m not an oncologist.” That’s how she ended the conversation. I was like, “What! What will make it more conclusive?”

Describe the fine needle aspiration (FNA)
I ended up going by myself because it was going to be a quick test. I’m very scared of needles. I never dared to have lab results done unless told by my doctor, because needles scare me. It’s part of the fear and reason that I never gave blood. I never was a blood donor because of the needle.
Going into that appointment, I knew what was going to happen, but actually seeing how big the needle was really freaked me out. I was by myself because I was like, “I can do it.”
The doctor I had was understanding, and she said to me that a lot of patients actually have a fear of needles. She walked me step by step through what was going to happen, how they were going to numb the area so that I wouldn’t feel it.
[They stuck the needle into the area of the lump with a long, thin needle.] It was a quick prick. The numbing sensation was much harder to deal with. It was so quick.
And I wanted the answers, so I pushed all my fears aside because I needed to get this done to get answers for myself.
It was a very, very quick process. I don’t know if I was there more than 20 to 25 minutes.
When did you get the FNA results?
It was a Friday afternoon, and I was fishing to have answers right away. I think I got the results back on a Monday or Tuesday of the following week.
The ENT was the one who gave me the results. She said it was inconclusive. She said there was still concern and wanted to do the surgical biopsy.
Describe the surgical biopsy procedure
I walked into it not doing a lot of research. I’m really good about doing research, but I figured they’ll me when I get there, just like they did the needle (biopsy).
When I got there, I got nervous when I had to sign some release papers because I didn’t realize it was a surgery since over the phone they said, “You’ll be out within an hour.”
When I signed the release papers, that’s when I started asking the questions of what exactly I was going to go through, because being unaware of that for myself got me nervous. I realized they’re probably going to use some anesthesia, and I’m going to be out for the count.
That was not the case at all. It is surgery because they did have to have it open where I had found my lump. They numbed it, but I wasn’t under, so I was aware of what was happening, but I couldn’t feel anything.
They took a piece of what was there out and were going to send it to the labs, which is why I had to have surgery — so they could cut open and take a piece.
Because I was aware of what was being said, I remember the doctor who was doing the surgery say something like, “This feels like…”
When he was done, I brought up that conversation I had overheard. He said, “I can’t say anything conclusive now, because nothing’s conclusive unless it’s in the lab and we can study it, but it feels like what most cells under certain cancers feel like.”
It was making me more aware that it was a high possibility, but because nobody could be 100% conclusive, I still sided with hope that this was nothing.

What were the surgical biopsy results?
After that, they gave me the results back that Friday when the ENT doctor called me. That’s when I knew it was something serious, and I would have to go through treatment.
I didn’t have the idea of cancer, not being familiar with any other type of cancers, only those exposed from the media and with some family, who didn’t have a pleasant experience.
She called me on that Friday, and she said, “This is serious. I can’t tell you everything about what it is, but it’s very likely a Hodgkin lymphoma.” That was the first time [I heard of Hodgkin lymphoma].
What she did do was say, “You have to schedule an appointment with an oncologist.”
I was like, “I don’t have that readily available.”
Immediately after that, I sent my primary care doctor an email because I was getting frustrated with so many people not wanting to be 100% conclusive about what was happening.
Knowing there was something there, but they weren’t fully telling me what that was. Maybe it was a point of caution, protecting me from going down a path by myself or whatever. I just wanted it to be conclusive, so I called my primary care doctor.
How was the CT scan?
It was my first time. I knew they had to put some dye, and there are so many different variations of how CT scans [are done]. That is something I did Google: “What is a CT scan?”
Before the appointment there, I called and asked, “What kind of CT scan is this? Should I not eat anything?”
The person who made the appointment didn’t tell me everything I should do prior to the appointment. They said, “No, just come in.” At my hospital, it’s in a trailer. I noticed that a lot after that appointment. I noticed a lot of hospitals are putting their CT and PET scans in trailers because of the radiation and outside the facility. So that was a different experience, getting walked from the waiting room into a trailer.
It was quick. They put a needle in you to put the [contrast] dye in, and you lie on this bed. Then you go inside a half-tube, so it’s not an MRI where you go in fully. It’s a half tube. You lie there as still as you can until they have enough images of you for themselves.
I’m not nervous, not claustrophobic, and because I’ve learned to meditate over the years, I found myself meditating as I went to do that.
They walked me through it, saying, “Hold your breath. Now release your breath. Hold your breath. Now release your breath.”
This may sound weird, but because I don’t like needles, I appreciated this kind of test, when I wasn’t exposed to long needles or anything.
It’s just a little prick on the arm to get the dye in me, feel a little heat sensation and be done with it. I didn’t find it as scary as some of the others.
Warning: you’ll feel like you’re going to the bathroom with the contrast dye!
It’s a weird sensation! They warn you. The technician administering it will say, “You’re going to feel this sensation. Don’t be alarmed.”
How long did it take to get the CT scan results?
It took them a week. I didn’t even get to see the results until the oncologist appointment. It was very surreal because I was going through one test after the other. I don’t remember exactly when they talked to me about that, but I do remember them bringing it out for my oncologist appointment.

Pushing for the PET scan (self-advocacy)
I pushed for that to happen more quickly. What I’ve learned about PET scans is that they’re very hard to administer because there are so few of them in hospitals. Looking back, I would recommend for a person advocating for themselves to push to see if a PET scan is needed and to make sure it happens.
A CT scan happened for me, and then when I was told I should get a PET scan, I asked a lot about why I didn’t have the PET scan right away. When I was trying to schedule it for myself, nobody was scheduling it for me. It seemed like it was going to be months out.
They were like, “You can’t have a PET scan until September.” I was like, “No, no.” I think what helped me get it earlier was I had said from the beginning that my husband and me had a vacation planned, and I needed to know whether or not to take that trip because I was starting to get worried. When they said September, I said, “That’s in the middle of the vacation.”
Putting that urgency in them helped them find a hospital that did have a PET scan earlier than what they were offering me. I actually had to drive about an hour and a half away from where I live to go to that hospital facility to get the PET scan.
I was exhausted from all of the tests, and they assured me that this would be the last test, where they’d be able to be more conclusive about what I had.
So I went with my husband, and we made a trip out of it. We went with enough time. I met this wonderful woman in the waiting room, who saw how anxious I was and just sat with me. That was one of the most soothing, most calming conversations I’ve had.
I was like, ‘An hour and a half drive to have this conversation is probably my destiny.’ When I went into the PET scan, I felt almost relieved that this might be the last test so that they could just conclude what was happening.
Describe the PET scan
The technician was wonderful. They put a sugar substance (glucose) in (through IV), and you have to wait an hour before you go in to get a PET scan. When he put it in, the technician told me to just take a nap for an hour.
Similar (to the CT), but different because of the hour-waiting period beforehand. [With the] CT scan, you go straight in, they put the IV in and scan you. The PET scan, they put it in, and you wait an hour for (the glucose) to go through your entire body before they do the scan.
The PET scan only took about 20 minutes. So it was waiting an hour, 20 minutes for the full scan, 5 minutes to close out.
How long did it take to get the PET scan results?
Because I had pushed all these conversations, I had my first oncologist appointment the following Tuesday, which is when the PET, CT and all other tests were put in front of me.
Diagnosis
Trying to get answers from the beginning
I was at Kaiser South San Francisco. I only say that because South San Francisco doesn’t have all of the tests (and equipment) you need. They don’t have a lot of doctors to administer these tests, so it was taking them a long time to coordinate.
With so many patients, I found myself needing to prioritize myself.

It’s like the doctor wants to help you, but there’s a line that you’re in. I was not willing to wait in line, for better or worse, because I had this trip, and I needed to know whether or not to take it.
I sort of aggressively said, “I get there’s a waiting period, but I need to have some of these tests done faster, or I needed the results faster.”
I just really wanted to know. I had planned a vacation with my husband. I was pushing for more answers so that we could decide whether or not we were going to go on that trip. When she said, “I’m pretty sure, but it’s not conclusive,” that’s when I pushed my primary doctor to coordinate all the pieces together for me.
In late July when I had met with my primary care doctor, the medical system had pushed me to do all these tests with other people, and now I was hearing from the ENT, “I’m pretty sure, but…”
So I went back to my primary care doctor and said, ‘I really need an answer. If this is something that looks like cancer, I need to know.’
That’s when they finally scheduled me with an oncologist at the medical facility, and I finally heard about a month and some weeks later, yes, 100%, this is what they had now diagnosed as Hodgkin’s lymphoma.
The diagnosis at the oncologist appointment
I’m with my husband. I knew at this point, and I wanted to be with someone. I had felt pretty sure that I had Hodgkin’s lymphoma because so many people had said it was likely. My husband, I think, did not have that full understanding yet.
I bring him up because my doctor came in the room, he walked me in, and he said pretty matter-of-fact, “You have Hodgkin lymphoma. Stages don’t matter, but we name it because of where it’s located in the body. For you, it’s in the spleen, so it’s stage 3B. Based on your symptoms and where it’s located, that’s how we can understand what treatment to give.”
Processing the diagnosis
My husband went white pale. He was so pale compared to the wall. The doctor didn’t recognize at all. He just kept going through the motion and diagnosing me, telling me the next steps.
I had to ask my husband if he was okay, which gave him permission to leave the room really quickly to catch his breath.
It was really upsetting because I wanted the doctor to acknowledge that it’s not just me getting the diagnosis. It’s both of us. We’re going to have to both go through this.
I obviously have to go through the treatment. But I remember just losing focus a little for the rest of the conversation and not necessarily processing all the other details.
He gave me a handout to say, “This is the standard treatment that you’re going to have, ABVD. This is what it is.” We concluded the appointment with him walking me through the infusion center because it’s right next door.
We walked through. He introduced me to a nurse and said, “Okay, we’re going to get started as soon as possible.”
I just remember walking out, and I was angry that I had to wait again, because I thought getting the diagnosis was great. At least I had some clarity in it, because then I could move forward. But again, that weighed on me knowing that this could possibly be the doctor I worked with. I wasn’t going to have that. It wasn’t a great first appointment with them.
It was a relief to finally receive the diagnosis, when for the past month I had only heard, “I’m pretty sure,” or, “I think it is,” or, “Maybe.” When you hear the, “Yes, it is, 100-percent sure and this is the treatment that is given,” it was that weight that lifted from me.
»MORE: Processing a cancer diagnosis

How did you get through the 6 weeks of waiting for answers?
I call myself a lifetime runner, and any challenge that I’ve ever experienced in life, I would run. I would run around my neighborhood. I would take different trips around the Bay Area to different hiking trails to go on a run with my brother. I’m still amazed at what the mentality of how you handle certain anxiety can get you through.
I was having very severe symptoms at that point. I was having night sweats, maybe getting 3 to 4 hours of interrupted sleep, and yet I was still running because I needed that for my mental state.
It wasn’t fast running. I noticed I was slowing down, but I would push myself to go outside and think of what my body’s capable of, despite the stresses of what was happening.
Looking back on it now, there’s a race I did with a runner’s club I’m part of here, and it was a 3-mile run. At the time, I’m like, “Definitely, I could do 3 miles.” But it was a lot of hills I wasn’t expecting. I still did it.
[At] the race, they took pictures of you, and there’s a picture of me at the finish line. As I look at that picture, I think, “Whoa, I was going through all of these unknowns, and my body was inflamed and feeling hot, uncomfortable. Yet I’m there, finishing.”
It was finding those moments to be really proud and amazed at what my body could handle, which got me through the waiting period.
Even when I received the diagnosis, I’m like, ‘This body is really strong, and whatever treatment I have to go through, I trust that it’s going to be strong enough to handle.’ At least that was my hope.
I was also amazed with the community I had surrounded myself with. I’m spiritual and religious. I found myself going back to praying devoutly and with my father, who I hadn’t prayed with in a really long time.
He lives close by, fortunately for me, so I stopped by my parents’ and said, “I’m going through this and need us to pray.” So praying with my parents and my husband really helped me mentally know I have this community of people who are going to care for me as well.
And I have myself. As strange as that sounds, it was like I have my community that’s going to support me, and I have myself. Those 2 things really helped me get through this really stressful waiting period.
Treatment Decisions
Getting a second opinion and more information
It prompted me to look at a second opinion and talk to other people. I do appreciate you putting this together, because I did go online to look for other support organizations with Hodgkin lymphoma to gather all my facts for myself, rather than one doctor telling me this was it.
I was looking for people who’d been diagnosed with Hodgkin lymphoma, trying to find out if it was the standard, because hearing that it’s the only option was annoying to me. I wanted to know, is this treatment it?
I wanted to talk about nutrition because I’d read that nutrition helps with treatments. I also wanted to explore that, but the first oncologist was unwilling to talk to me about that. He said, “This is it. This is what you have to do, and it will go away.”
I refused to believe that, so I did seek a second opinion at Stanford. It was an online doctor, I later found out. I thought I was going to have an appointment. Being vulnerable in that moment, I saw Stanford’s online second opinion.
I thought I was going to meet a doctor there, and it wasn’t that at all. It was me submitting my results for a doctor to look at and having one of their nurse practitioners call me to make the same conclusion.
Looking back on it, it was helpful for me personally, but I don’t think I would have needed that if I had heard it differently the first time.
Getting another doctor
I talked to my primary care doctor because at the end of the day, she was my coordinator. I’d seen her for years, and she’s the one who prompted the tests.
I asked her if there was another oncologist on site because I didn’t feel comfortable. Her answer was a quick no. There’s no one else. This is all she knew of. I think she even ended the conversation with, “Good luck.”
But I know Kaiser is a big operation, and there are other hospitals. Because I live in San Francisco, I was encouraged by a friend to look at Kaiser San Francisco. Even while I was waiting for my second opinion, I had reached out to them.
I’m so glad I did because it was such a different world there.
I was able to almost back-to-back get the Stanford second opinion, and at the same time get a call from Kaiser San Francisco letting me know that one of the doctors were available and was able to see more patients. So they partnered me with him.
My first appointment with him was a little more than an hour. To be transparent, he was a fellow in the hospital. I didn’t care because I figured he’s working with other oncologists who had been there for over 30 years, so in fact, having a fellow partnered me with 2 other long-time, experienced doctors.
My first appointment, Dr. Neeman (the fellow) and Dr. Lopez (who is the overseeing doctor) came in and gave me a hug.
They said, “We’re sorry you’re going through this. You must be really stressed out.”
I remember starting to tear up a little bit because that’s all I had wanted — the acknowledgement that this was scary. They noted that.
Then they went through the logistics. They also told me about all the resources that are available at Kaiser San Francisco that I didn’t even think to ask, even through all my research, even in the initial appointment.
They let me know there’s a social worker on site, a nutritionist that’s available to help me with the eating piece, [and] a chemotherapy orientation available to answer all my questions about what that would look and feel like.
At the end, they left and said I was going to be fine. It was just a weight off my shoulders. Yes, this is all I wanted.
That acknowledgement, the support, and the other pieces of information, not just about the cancer but how to deal with it, which was really helpful.
Relationship with doctors
What has helped me with working with the doctors, because it is a community of people wanting to help you. I would have never said that had I gone through this, but I only say that because doctors don’t want to give you information that might not necessarily be true.
In the world of science, everyone needs 100% assurance before they move forward with treatment or interrupt your life. What helped me was just asking a lot of questions.
It wasn’t until that test (surgical biopsy) that I started, for unhealthy reasons, Googling a lot. But I wasn’t Googling, “possible diagnosis.” I was Googling, “questions I should ask my doctor” and reaching out to friends who work in the health field on what questions I should be asking.
As a patient, they don’t want to alarm you, but they also want you to take caution that this is something serious and you should move forward, especially as people have so many of their own myths and ideas of what cancer and treatment are.
Guidance on top questions for patients and caregivers to ask doctors
The important questions are letting them know everything you’re going through. Not just related to the physical, but sometimes where we go to.
I know when I would go to the doctor, I would only talk about the physical, but also the emotional piece and other pieces you’re concerned about.
Friends and family have always told me I’m a workaholic, so this interruption was obviously going to interrupt that. I told the doctors at that appointment, “What about work, and how am I going to deal with that?”
That’s when they brought up the social workers. They said they’re going to be available to you to help you through that. They’re the expert in it. I’m the doctor and I’m the expert in a, b, and c, which is really helpful because in organizing all of the things that you’re going through, it was easier for me to hear people say what they’re the expert in.
So, I’m the doctor, I’m the expert in treatment. This is how I’m going to work with you the next few months. I was able to put that in a notebook and say this is what I go to this doctor for, what I go to the social worker for, and whom I go to for what I eat. I used all of those resources.
When I didn’t find them, I would ask and the social worker became a huge part of my journey because she was so knowledgeable in everything else. She was someone who introduced me to the Leukemia and Lymphoma Society, which I had signed up for already just because they sent me a bag with a bunch of information. She was the additional push I had to attend some of their support groups.
Chemotherapy
Describe the ABVD chemo regimen
I had ABVD chemo administered to me every other week. The math is a little challenging but they consider two treatments one cycle, so I knew that I needed six cycles. I would have that spread over about six months so every other week.
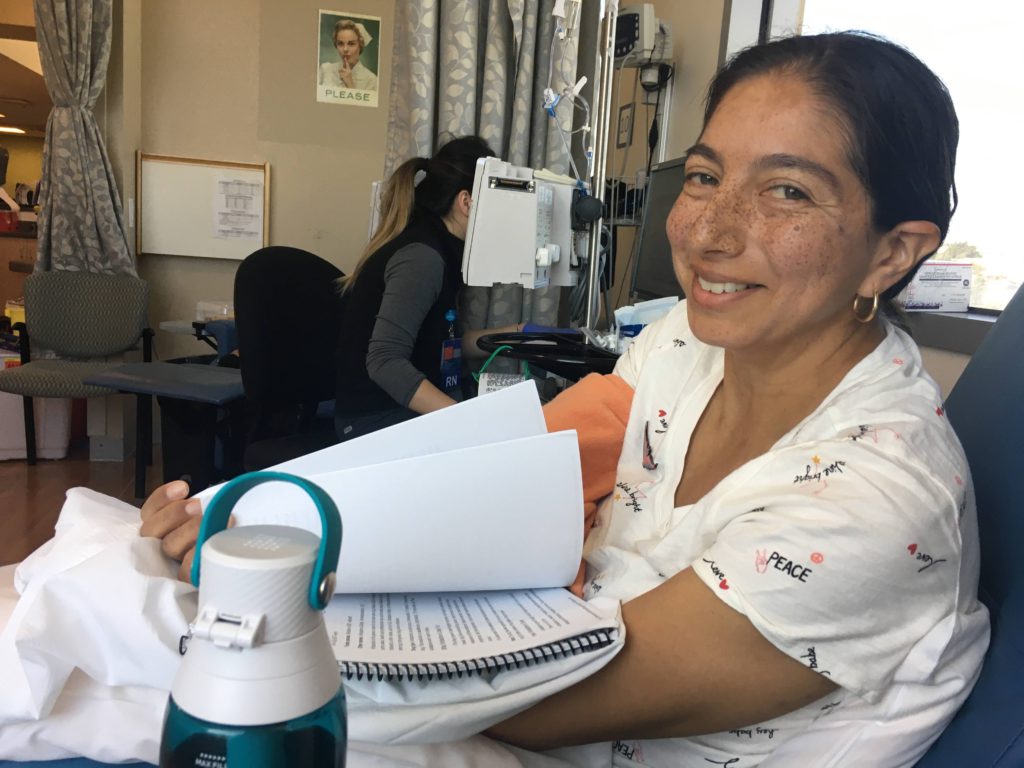
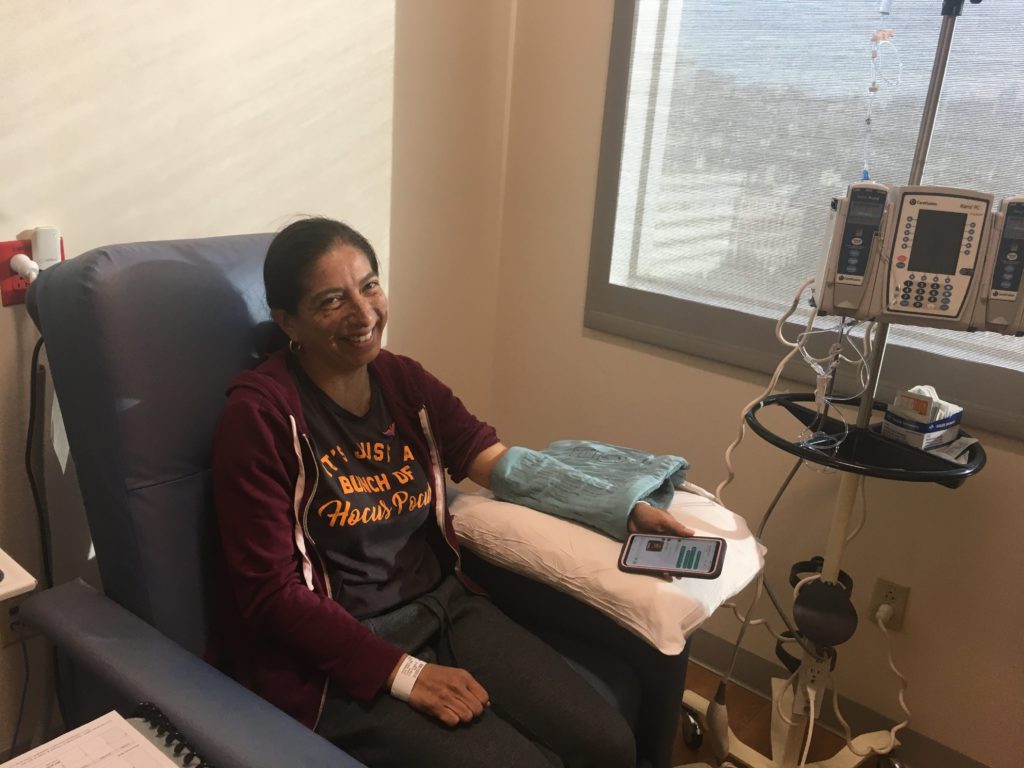
After four cycles, they would do a check for me. ABVD that first appointment, I was going to receive it every other week, and I didn’t know what to expect. It turned out to be only a two- to three-hour appointment.

Deciding to use IV in veins (instead of port, PICC line)
I didn’t choose to get a port, which is when they put in an incision to m