Donna’s Multiple Myeloma Story
Donna K., Refractory Multiple Myeloma
Symptom: None; found through blood tests
Treatments: Total Therapy Four, carfilzomib + pomalidomide, daratumumab + lenalidomide, CAR T-cell therapy, selinexor-carfilzomib
Donna’s Multiple Myeloma Story
Featuring Dr. Cristina Gasparetto
Donna K. was just 59 years old when she was diagnosed with multiple myeloma, a cancer that starts in plasma cells, one kind of white blood cell. There were no obvious symptoms — she discovered the myeloma through a blood test and went through one of the most aggressive treatment regimens of that time (“Total Therapy”).
In our educational series, this avid cyclist and grandmother details her 5 lines of therapy, from heavy chemotherapy with 2 stem cell transplants to many triplet combinations, including the selinexor + carfilzomib + dexamethasone combination she’s currently on.
Also part of this conversation is Donna’s oncologist and top myeloma specialist, Dr. Cristina Gasparetto. The Director of the Multiple Myeloma Program at Duke Health delves into the STOMP clinical trial that Donna is a part of and with which she has found success.
- Introduction
- Multiple myeloma diagnosis
- The relapse
- Treatment decision-making conversation
- 2nd- line therapy
- Cases for switching drugs and drug classes
- Signs of the next relapse
- Decisions on next lines of therapy
- Clinical trials
- Selinexor triplet clinical trial (STOMP)
- Deciding to try the STOMP clinical trial with selinexor
- A good triplet for patients who don't respond to daratumumab
- Selinexor's first and latest approvals
- Getting monitored on a clinical trial
- Your reaction to a new line of therapy
- Side effects
- The treatment regimen from the patient perspective
- Ways to manage through the side effects
- The power of setting expectations
- Do you pay attention to the next promising drug or combination?
- Living with multiple myeloma
- The STOMP Clinical Trial
These interviews have only been edited for clarity. Thank you to Karyopharm Therapeutics for its support of our educational program.
This is not medical advice. Please consult with your healthcare provider for treatment decisions.
Making Treatment Decisions with My Oncologist
Donna details her diagnosis through her first relapses, living with multiple myeloma, and the patient perspective of making her treatment decisions.
Her current oncologist, top multiple myeloma specialist Dr. Cristina Gasparetto of Duke, also shares how she helps her patients arrive at treatment decisions at each juncture and what patients should be asking their own doctors.
Introduction
Stephanie Chuang: Hi, everyone, it’s Stephanie with The Patient Story, and I am so thrilled to be introducing the people part of our conversation today, our guests.
Donna will be sharing her incredible story and what she’s gone through with multiple myeloma and the incredible spirit with what she’s done.
Her doctor, her myeloma specialist, Dr. Cristina Gasparetto, is the director of the Multiple Myeloma Program at the Duke Cancer Institute.
Welcome to you both. Before we dive in, there’s a lot to talk about. Let’s start with you, Donna. I want to just ask you to try and talk about yourself the way you would to someone new about who you are, Donna, outside of the cancer context.
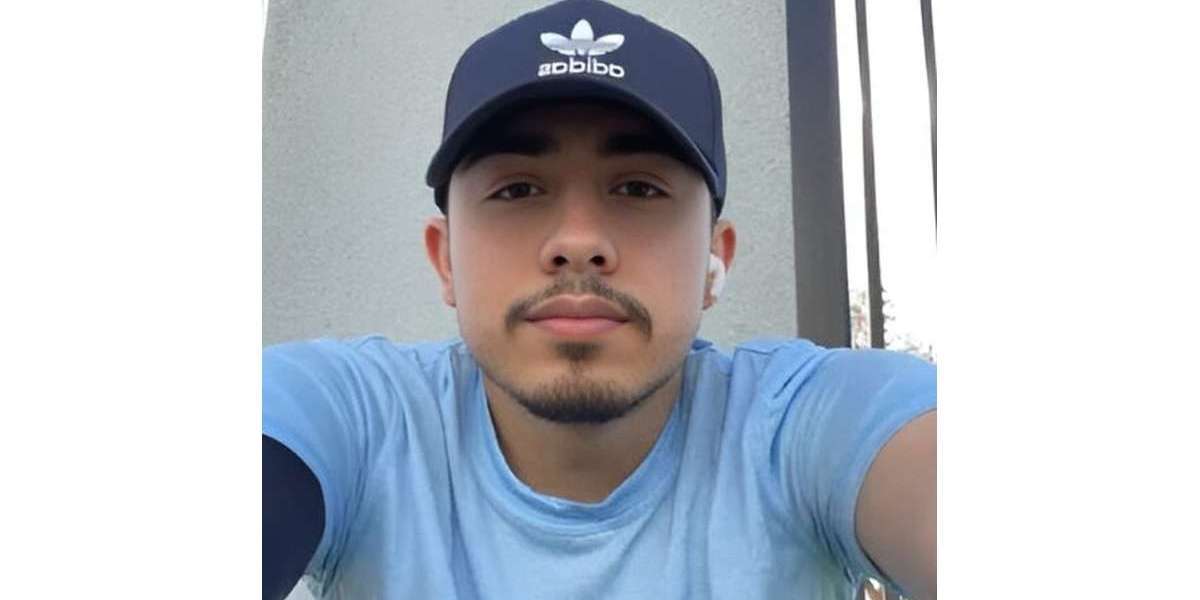
Donna K., Multiple Myeloma Patient
Donna K.: Thank you. Well, I am a grandmother, first of all, and an athlete. I like to go out and work out all the time, and I’m a former product line manager in a computer networking industry, where I spent most of my career. I’ve been retired for several years and have traveled most of the East Coast.


I spent half of my life with this disease, and I just want to help people. I just want to win.
Dr. Cristina Gasparetto
Dr. Cristina Gasparetto, Duke’s Dir. of Multiple Myeloma
Stephanie Chuang: Thank you so much for sharing that. Dr. Gasparetto, when I was first talking to Donna about her experience here, she said, “She’s a force to be reckoned with, that Dr. Gasparetto.” She also said just how indebted she was to the fact that you had called her in the beginning when she wasn’t sure whether to call you or not for treatment. That’s something else, because we know how busy you are. What drives you to do this for people?
Dr. Cristina Gasparetto: I feel like I spent half of my life with this disease, and I just want to help people. I just want to win. I don’t know if I can win the war, but a lot of battles with my patients. I want them to know that I’m there for them. It’s the only reason why I’m doing it. If not, there would not be a purpose.

Multiple myeloma diagnosis
Stephanie Chuang: Thank you for sharing that. I appreciate you both being here, so let’s dive right in. We’re not going to spend too much time with the first-line treatment. Donna, I think people will be interested in understanding how you discovered that you had myeloma, what it was and how you dealt with that.
Donna K.: I’m a fortunate person in that I discovered multiple myeloma before it had done any structural damage. I just discovered it through a blood test and rapid bone degeneration. It turns out one of my markers is in my blood, so it can be tracked and monitored by blood tests. I was lucky.

How did you decide where to get treatment?
Stephanie Chuang: At the time, you mentioned you had gone to a center that had touted — this is back in 2012 — that it got patients to 5 years. Can you describe that and what you were feeling as you went through your first treatments?
Donna K.: Anybody who gets a cancer diagnosis is in shock for a while, and I went into investigative mode and was directed through the friend of a friend to a place where she had gone, where they had the best progression-free period at that time, which was 5 years.
I went to Little Rock for 11 months of treatment. Actually, at the time, it was somewhat unique. It was a rough treatment, but fortunately, I was fit enough to deal with it.
Learning about remission
Stephanie Chuang: That was June 2012 to May 2013. You had undergone several different therapies. How did you find that you were in remission, and how did you respond at the time?
Donna K.: Unfortunately, I found out I’m in complete remission with a bone marrow biopsy, so it’s not a fun way to find out. It was 11 months when I was in complete remission, but I continued with a maintenance program.
It doesn’t end as soon as you get in complete remission; it’s just that I got to move back home. The bone marrow biopsy can determine if you’re minimal residual disease (MRD) negative, and it’s the quintessential test for the disease. The blood test just tells you whether or not it’s time to check the bone marrow.
Stephanie Chuang: Thank you for running us through that. What was the maintenance therapy you were on?
Donna K.: It was Velcade and Revlimid, so it was pretty intense for a maintenance program, and I had some bad reactions. I ended up discontinuing after 8 months because of the reactions.
Stephanie Chuang: What reactions were those?
Donna K.: Severe neuropathy, other stomach issues, other things.
What questions should patients ask about 1st-line therapy?
Stephanie Chuang: Thank you for sharing, Donna. Before we go any further, Dr. Gasparetto, I know you didn’t see Donna at the time, but what’s your general guidance? There are many different patient profiles, but when people are not going to a specialist, what questions might they need to consider asking that doctor about treatment for that first-line therapy?
Dr. Cristina Gasparetto: It’s a long discussion when we meet a new patient with myeloma. We go through the myeloma presentation, and every patient is different. So we spend a lot of time talking about the initial presentation like Donna’s.
Unfortunately, some patients will present with more symptoms. Sometimes they have to be admitted to the hospital because the severity of the symptoms. It is a very heterogeneous disease. We spend a lot of time about myeloma, what myeloma can affect, and then the treatment and the goal of treatment.
I like to talk with the patient about the expectation, because like Donna mentioned, you start and then you have to go on. She was at Little Rock for 11 months, then she immediately said, “But then I have to stay on therapy.” Trying to set up some goals, there is the light at the end of the tunnel.
We go from the intensity of the initial therapy. The achievement of the complete remission, like Donna mentioned, the minimal residual disease (MRD). Then we start the maintenance phase, where we hope to be able to control the myeloma for a prolonged period of time.
Of course, it’s not easy, and some patients will develop toxicity. Sometimes it’s what we call the cumulative toxicity because it can occur with time, with the continuation of treatment. I like to spend a lot of time about the disease and then the treatment journey that we embark on.
Stephanie Chuang: Thank you so much. There’s so many different kinds of people and, as you said, patient profiles. That conversation is so different depending on where you fit there. I know a big determinant, of course, would be like age, for instance, and other…
Dr. Cristina Gasparetto: Other diseases, other comorbidities. You can make your decision based on a lot of factors.
The relapse
Stephanie Chuang: Now we’ve set that landscape up. Donna, I know you didn’t have additional treatment through 2013 into the end of 2017, so about November. What happened at that point, when you realized you’re going to need to go back into treatment?
Rising myeloma markers (M-protein)
Donna K.: I’d been getting a monthly or a quarterly blood test. The longer you go without any evidence of the disease, the farther apart the blood tests are. The blood tests started showing an increase in my myeloma markers, so I knew something bad was happening.
Waiting for the right moment to restart treatment
Finally, in 2017, after monthly tests, it was determined that it was at a point where we needed to respond to it. What I found is that in general, my oncologists — and mainly I’ve had two, Dr. Barlogie and Dr. Gasparetto — they’ll let you enjoy your life fully until it’s absolutely necessary to start the treatment. If the myeloma’s just growing slowly, they’ll give you a chance at not having to be tethered to a hospital.
Stephanie Chuang: Which, of course, is a huge decision. I understand in talking to a lot of people, both patients and oncologists, it’s that balance of quality of life — being able to live life — and then making sure that there’s no progression or attacking the disease.
When do you restart treatment?
Stephanie Chuang: Dr. Gasparetto, in general, what are you looking at when you want to decide whether to restart treatment for somebody?
High-risk myeloma
Dr. Cristina Gasparetto: We take in account, again, a lot of factors. One of the most important is how long the duration of the first response was and how aggressive the genetics of the myeloma. If we are dealing with a patient with high-risk myeloma based on the genetics, we generally need to be a little bit more aggressive, and we can’t wait because the myeloma will cause more damage very quickly.
Standard risk myeloma
If a patient has slow progression with what we call the standard-risk myeloma several years after the initial therapy, sometimes we watch and wait a little bit longer because we know the moment that we start therapy, there is no way back. We have to continue.
We follow some patients. For example, some patients evolving a few years after transplant, 4 or 5 years, sometimes we don’t start therapy right away. We watch and wait. If we start to worry that the myeloma is progressing more rapidly, that is when we need to start.
That doesn’t apply to all patients. If we have a patient with aggressive myeloma from the very beginning, we probably will not be able to wait so long. Again, we take in account a lot of factors and the disease, the patients, the prior therapies.
Treatment decision-making conversation
Stephanie Chuang: Again, thank you, Donna, for coming out sharing your story so openly, because I think it’s a great thing for someone to be able to see an example.
Here we are. It’s Dr. Gasparetto and Donna, and you’re having this conversation. What was that treatment decision conversation like for the both of you? We’ll start with Dr. Gasparetto, and then, Donna, I’d love to hear from your perspective.
From the doctor perspective
Dr. Cristina Gasparetto: With Donna, she was able to remain in remission even without the major maintenance for a few years, a fair amount after the transplant. Her myeloma was progressing slowly, but then at a certain point you need to initiate therapy no matter what, so when you have the hint that the myeloma will start to progress.
Then you have to choose therapy based on the prior therapy received. Because Donna was treated at Little Rock, she went through the Total Therapy, and then she experienced a fair amount of toxicity with the Velcade, with bortezomib, with Revlimid.
You need to switch classes, you need to change, and you need to choose a drug that’s very effective but with a different type of toxicity. She could have gone back to the Velcade, but with the peripheral neuropathy, that was not an option. You have to modify the regimen again based on the prior therapy, along with the duration of the response and the toxicity.
Different factors in how patients respond to treatment
Stephanie Chuang: Wonderful. Normally, we don’t talk about age and things like that, but in this context, we do because we know that the median age of diagnosis for myeloma is somewhere like 69 or 70. Donna, may I ask when you were first diagnosed, how old you were? And then again at relapse?
Donna K.: You’re going to ask me to do math? It was 9 years ago, but what does that make me? 59. I was young. I mean, in terms of the lottery, I was young. I wasn’t the typical patient.
Dr. Cristina Gasparetto: Donna is very fit, and it makes a lot of difference. I always tell patients, “It’s not the age. It’s also your performance status, and that allows us to be sometimes more aggressive.”
We do have something in common, Donna and I. We still belong to the same cycling team. Being a cyclist, Donna was coming up in good fitness, and that’s the reason why she was able to cruise through the Total Therapy, with all the the aggressive therapy that she received. It makes a lot of difference.
Stephanie Chuang: That’s exactly what I was asking for, was the age and the overall fitness profile. Dr. Gasparetto, I’m just so glad you’re talking about that. Overall, for people just to understand, there has been a shift in terms of the paradigm, the philosophy. You’ve got to hit it hard to get that deep response or the best response up front.
Dr. Cristina Gasparetto: When Dr. Barlogie established the Total Therapy program, we didn’t have anything available, because even the thalidomide came out from his group or from his team. It was the first clinical trial in myeloma patients with thalidomide. It was published in 1999. Before that, we just had chemotherapy.
The idea of using the intensity comes from him. But now, 20 years later, we do have a lot of new drugs, new agents and new mechanisms of action.
Getting that diagnosis that it was back is so traumatic. It’s almost worse than the first time.
Donna K.
From the patient perspective
Stephanie Chuang: That’s so promising, and that’s part of why we do this, too. Thank you, Dr. Gasparetto. Donna, you had said that right off the bat when you were first diagnosed, you were 59, young, fit. You were ready to go, and you wanted the most aggressive approach. Then you went through this, even with the Velcade and the Revlimid, dealt with severe enough side effects with the neuropathy that you felt it’s a little bit too much.
Knowing all of that and with your experience with such an aggressive first-line treatment when this all happened, you’re talking to Dr. Gasparetto about how to attack the myeloma again. What was top of mind for you? What was most important? Were you thinking, “I want to be just as aggressive,” or were you thinking, “I also need to balance my quality of life”?
Donna K.: Getting that diagnosis that it was back is so traumatic. It’s almost worse than the first time. My first thought was I’m not going to even end the chemotherapy this time. If they want me to stay on maintenance for 20 years, I’m going to stay on maintenance, because it was so important to me to keep the beast asleep, if you will.
2nd- line therapy
Stephanie Chuang: Thank you for sharing that insight. I’m sure many people feel the same way you do. With that in mind, Dr. Gasparetto, what helped you decide on Donna’s next treatment of carfilzomib (Kyprolis), lenalidomide (Revlimid) and the dexamethasone?
Why choose carfilzomib?
Dr. Cristina Gasparetto: Donna and I started to talk a little bit after that. She was followed initially by another oncologist who was not super specialized on myeloma. We started to talk and have a conversation. The carfilzomib was the decision because of the toxicity that Donna had experienced with the Velcade.
Again, we are using the triple combination in a relapsed setting. At that point, she needed to go back to a triple combination. She was off therapy for a while, so she progressed off therapy. Circling back to the Revlimid made absolute sense. You could have gone back to the Velcade, but no, due to the toxicity.
The Kyprolis with the Revlimid and dexamethasone was a very important combination established. We have data from randomized phase 3 trials showing the effectiveness. The fact that it was effective and the durability of the response was quite impressive.
Again, the reason why we choose very aggressive combinations even in the relapsed setting was because we have learned with time that we can treat the myeloma suboptimally. The myeloma, unfortunately, will develop the resistance very quickly, so we want to go out of the gate very aggressively.
Cases for switching drugs and drug classes
Stephanie Chuang: I appreciate that, because again, it’s highlighting a different sort of shift here in the approach. We know we have different classes of drugs. We won’t go into all the names and everything, but if someone’s not responding well — whether it’s efficacy or side effects, it’s too harsh — do you replace that one?
Do you go to a different class of drugs in the combination, or can you use a different drug in that same class to see if it might be different for a patient?
What to do when patients develop resistance to drugs
Dr. Cristina Gasparetto: For a patient developing resistance, we like to make the class switch. They’ll go to the next generation. Like with the IMiDs, we go to the lenalidomide (Revlimid) to the pomalidomide, but we like to make what we call the class switch and try to attack the myeloma at a different level.
Switching treatments because of side effects
Stephanie Chuang: It makes sense to switch classes of drugs. One’s not working. If it’s not working with myeloma, how about with side effects? Is it the same?
Dr. Cristina Gasparetto: Every drug comes with baggage, right? We have learned with experience. It doesn’t apply to all patients, so it’s very interesting.
There are some patients doing phenomenally with a combination, and other patients that start to have toxicity from the very beginning. Sometimes we just have to try and then if it doesn’t work, we make the adjustments. Sometimes dose modifications is enough.
Sometimes we have to completely switch to a different drug. Again, it’s very subjective. It’s patient by patient, and we try. Even in a clinical trial, we follow the patient through when they discontinue due to certain toxicities — how many, do we have doses held or dose modifications? That is becoming part of treating patients with myeloma.
I have a phenomenal team at Duke. I have some incredible APPs (advanced practice providers), PAs (physician assistants) and nurse practitioners working with me. I call them my front line because they become so used to the drug.
There is a lot of education for the patients, too. We want them to be aware so they can come back to clinic and talk with us, so we can make proper dose adjustments.
Even with the Velcade that Donna experienced, when it doesn’t work, it’s not written in stone. We’ve learned that sometimes holding the Velcade, making those modifications, we can manage the neuropathy.
It doesn’t work for everybody, so it’s difficult to say, “I’m going to do this, and it’s going to work.” It’s not fair.

I think the side effects of chemo are like childbirth; you forget it so you can go to the next one.
Donna K.
Side effects
Stephanie Chuang: But it’s on the table as an option. Whether it works is up to the individual patients. Donna, at the time, you weren’t working with Dr. Gasparetto yet, but then you’re on what they call a triplet, right? There was a 3-drug therapy. It was from November 2017 until June 2018.
High level — I’m not going to try and make you remember everything, but this is your first foray back into getting treatment again — what was that experience like. and did you had a lot of side effects you were dealing with? If you did, what they were?
Donna K.: I think the side effects of chemo are like childbirth; you forget it so you can go to the next one. But yes, the first week when I was in chemo, I was just devastated and having a little pity party inside infusion.
By the second week, I had this attitude that me and my oncology team were going to fight this together. I adjusted to the whole concept of it, and I don’t remember the specific symptoms I was feeling. From a Facebook memory, I know that it was making me feel not as good on the day or 2 after, and not as strong.
But really the childbirth thing, I pretty much forgot all of the things that I didn’t like about it. What I did like about it is it worked for me. It knocked my cancer back. I started in 2017. By early 2018, my M-spike had gotten to zero.
Learning about remission again
Stephanie Chuang: You’d already had this resolve once, and then you’re hit again with myeloma years later. You go through therapy. You have that attitude of, “We’re doing this together,” which is great. When you heard that news of the M-spike hitting zero again, what was your reaction?
Donna K.: I was ecstatic. I was joyful. I believed I had a touch of invincibility and a heck of a lot of luck.
The longer you stay on maintenance, the longer the beast stays asleep. It’s hard putting it to sleep the first time, so you better keep it asleep.
Donna K.
What was the plan after remission the second time?
Stephanie Chuang: I was wondering about that just because you had gone through this experience before. What was it like the second time to be able to feel that? You had mentioned, “If they wanted me to be on treatment forever, I would be on maintenance forever.” What was the plan after that? That was about June 2018, according to your timeline.
Donna K.: In fact, I didn’t follow through with what I said. When it came to maintenance, as soon as I could travel, I did. I had one planned right in the beginning. By the time I was 3 months with MRD zero, I went off treatment to travel and to see things.
Today I think I would do that differently, just because the longer you stay on maintenance, the longer the beast stays asleep. It’s hard putting it to sleep the first time, so you better keep it asleep.
Stephanie Chuang: Thank you for sharing that. That’s great insight. I do want to go back to that, though, because you made a decision to to live life, which I don’t think anyone could feel badly about. That’s why we do this — to be able to do things in our lives. If you were to highlight the decision of what else drove you to do that, is there anything else you’d like to add?
Donna K.: This is relevant to the whole experience all the way up to today, but I realized that I don’t have to travel to Niagara Falls and Acadia National Park to live life fully.
One of the things I figured out this time around since I am tethered to weekly chemo, there’s a lot of stuff within a 3-mile drive from me. I’ve just made it simple for me to experience all of that without having to drive a long distance and live fully without giving up all that much, just different location.
Stephanie Chuang: What I’m hearing is, you figured out living life is really important. That’s the quality of life, tending to yourself and feeling very alive, but that you figured out how to do it without having to stop therapy.
Donna K.: Exactly. That was a big thing for me. I’m a slow learner. I just figured it out last June.
Stephanie Chuang: I’d say that’s fast learning for a lot of people, actually. We’re going to dive into that more a little bit later on, but I appreciate your candor and your honesty there, because a lot of people can learn from your experience.
The Power of Clinical Trials
What is it like being in a clinical trial? Hear in-depth details of the experience from Donna, as a patient, and from Dr. Gasparetto, as a doctor who fights for her patients to get in these potentially life-saving trials.
Donna and Dr. Gasparetto share more about the different lines of therapy, including the one Donna’s on (as of publication date) that’s gotten her back into complete remission: a selinexor + carfilzomib + dex combination.
Signs of the next relapse
Stephanie: Donna, you were then out of treatment from June 2018. Then November 2019 rolls around, so one year and some months later, you’re getting follow up. Did the M-protein spike happen again? What got you back into treatment?
Donna K.: Fortunately, it’s always the blood. I am so lucky that a simple blood test can say it’s creeping back up. I really am lucky because I know not everybody can just rely on a blood test.
Stephanie Chuang: What was the conversation between you and Dr. Gasparetto?
Donna K.: Before Darzalex, I had been getting guidance from Little Rock, and they were guiding someone who wasn’t a specialist in myeloma. She was only doing what they had said.
I just decided that they were doing just what everybody else was doing, and there was no reason to rely on Little Rock. That was about the time our mutual friend insisted that I contact Cristina. He kept insisting, and then one night I’m sitting on my couch, and it’s Cristina.
I was a little rock star enamored here. I couldn’t believe she called me, which is just amazing, and she’s done stuff like that since then. That’s when I switched. We worked the whole next path together through our mutual discussions.
Figuring out next treatment
Stephanie Chuang: Now we’re in November 2019. Donna, this is the third time you’re dealing with news that you don’t want to hear. First, how did you process it this time around? Then in talking to Dr. Gasparetto, what was your part of the conversation? What was most important to you?
Allogeneic blood or marrow transplant is when these stem cells are transferred from one person to another.
Donna K.: When I found out I was going through this again, I wanted an allogeneic transplant because I had this hope that I would get those 4 years or 5 years like I had after my stem cell transplants in 2012.
We talked about it, and you can’t just jump into an allogeneic transplant. It’s not covered by Medicare. There are all kinds of issues.
It’s risky. It might not work, but I kept that in the back of my mind because I wanted that time off, that time where I could forget I had cancer.
Decisions on next lines of therapy
Overview
Dr. Cristina Gasparetto: Donna went through the combination with Darzalex and then the CAR T-cell. We were putting a lot of money on the CAR T-cell. I’ve done allogenic transplants, and I believe in immunotherapy, but it’s not an easy decision.
Deciding if an allogeneic transplant is right for someone
Let’s go back to the question, ‘Would I do that for myself?’ I have done it (immunotherapy) in certain situations, but you are always thinking about the risks that you are taking. The allogenic is a big, huge decision for several reasons.
We do have some good data, but it’s very limited because in reality, we have not been very successful with the allogeneic transplant in myeloma.
Donna went through another couple of treatments. Unfortunately, I believe the Darzalex was not so successful for you with the pomalidomide, right, Donna?
Donna K.: It didn’t work at all. My numbers continued (going up).
Dr. Cristina Gasparetto: She was feeling that. Then we attempted the CAR T-cell, which was immediately before COVID. She was the last patient that we were able to enroll in the clinical trial because we shut down everything.
That was okay for a while, because Donna loves to live outside. The CAR T-cell gave her the other opportunity of coming off the therapy for a little bit, but it didn’t last much. You never achieved a complete remission with a CAR T-cell.
Donna K.: Never did.
Daratumumab + pomalidomide + dexamethasone
Stephanie Chuang: The Darzalex, Pomalyst and dexamethasone was the first triplet you went to. Dr. Gasparetto, just in terms of making that decision, why start off with that triplet?
Dr. Cristina Gasparetto: She was never exposed to daratumumab and isatuximab. The two CD38 antibodies are becoming so important. We’re learning that exposure earlier is becoming critical, and we’re able to achieve deep, durable responses.
The Darzalex (daratumumab) is now subcutaneous (a shot), so it’s quite convenient. The isatuximab is not subcutaneous yet, but also you go from the weekly to the every 2 weeks administration, so you’re going to the doctor office not very often. It gives us the opportunity to still monitor the patient, so we don’t dislike that.
With the Darzalex, eventually patients are able to go to the monthly. In terms of going back to quality of life, it’s becoming an important combination. It made sense that she was treated with carfilzomib (Kyprolis) and lenalidomide (Revlimid). We go to the next generation IMiD, and we switched classes from the Darzalex.
What factors are most important to you in choosing treatments?
Stephanie Chuang: Donna, you want the myeloma to go away, obviously. But also there’s the quality of life: side effects, how it’s given (infusion, shot, oral) and how often you’re having to go in. How do these things weigh for you?
Donna K.: Going in isn’t the issue. The effects of the chemo are the issue, because you go in one day. You lose one day of the week where you can’t do anything you want, but then I have nausea and I’m not hungry for the next 2 days, so I really feel like 3 days of my life are spent dealing with cancer.
Oddly enough, I can get to the point where for the next 3 days, I forget I have cancer. If I could take a pill and be checked every 2 weeks and keep this in at bay, I would be ecstatic. I would be happy. I wish Darzalex had worked for me, but my numbers just continued to increase. It didn’t slow them down. It didn’t stabilize them.
Clinical trials
CAR T-cell therapy
I think in the future, the CAR T-cell is going to be much more effective and hopefully more durable for a lot of patientsDr. Cristina Gasparetto
Stephanie Chuang: That’s why the both of you decided to talk about CAR T. Dr. Gasparetto, how did that come up for you?
Dr. Cristina Gasparetto: The CAR T-cell was not yet approved. It was in a clinical trial, and we had phenomenal results. The responses are incredible, and some of the patients able to achieve the minimal residual disease are doing quite well after the CAR T-cell. They don’t require additional therapy.