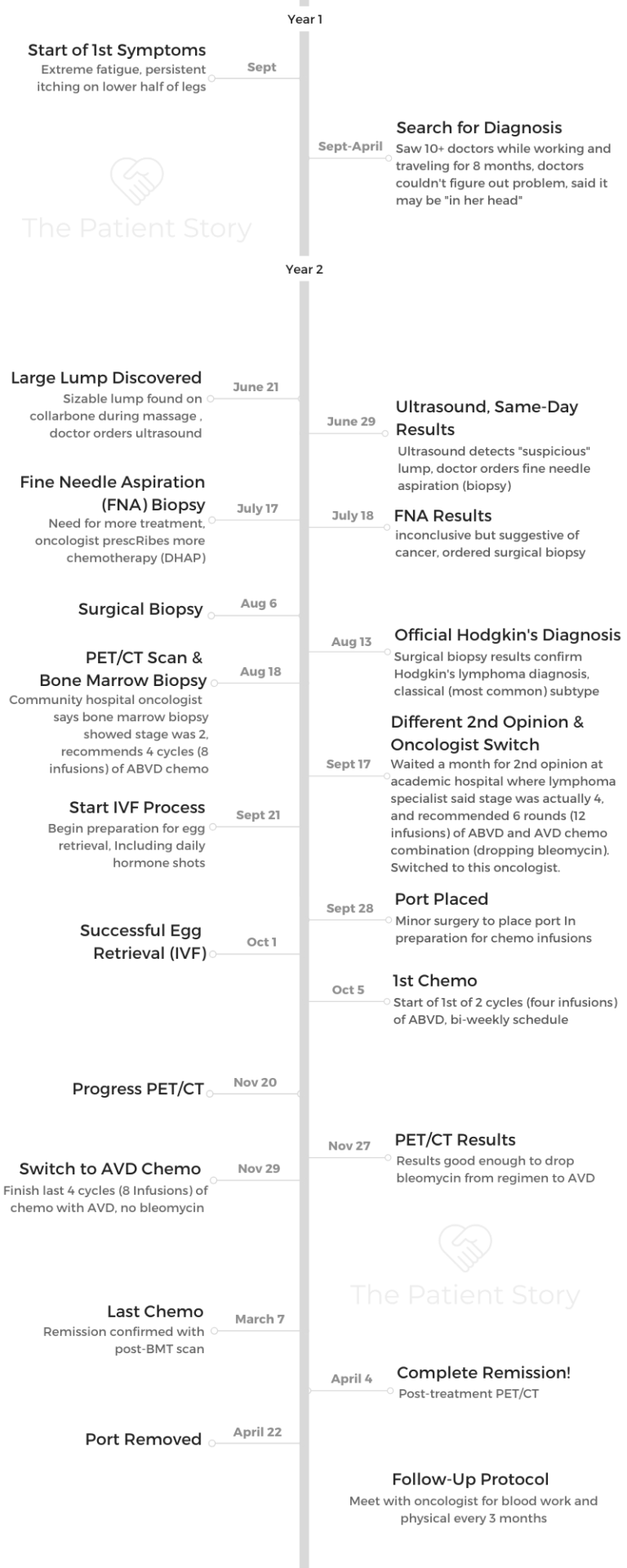
Nicole’s Stage 4 Classical Hodgkin’s Lymphoma Story
Cancer details: Staged 2 then 4 after second opinion
1st Symptoms: Extreme fatigue, persistent itching on lower half of legs
Treatment: 6 cycles (12 infusions) chemo, ABVD then AVD (dropped bleomycin)

Nicole’s Stage 4 Classical Hodgkin’s Lymphoma Story
Nicole shares her stage 4 Hodgkin’s lymphoma story, one that began with 8 months of no diagnosis and her determination to self-advocate for answers. She describes undergoing chemotherapy — ABVD then dropping bleomycin to AVD — and managing through side effects.
In her story, Nicole also highlights how a second opinion changed the course of her treatment, turning to integrative medicine to fight side effects and taking care of her mental health.
- Name: Nicole M.
- Diagnosis (DX):
- Hodgkin’s lymphoma
- Stage 4
- Age at DX: 26
- 1st Symptoms:
- Extreme fatigue
- Persistent itching on lower half of legs
- Treatment:
- 1st Symptoms & Search for Answers
- The Path to Diagnosis
- Describe the ultrasound
- Describe the fine need aspiration (biopsy)
- Next steps: surgical biopsy
- How did you get the initial cancer diagnosis?
- A family of medical experts
- Describe the surgical biopsy
- When did you get the full, official cancer diagnosis?
- How did you process the Hodgkin's lymphoma diagnosis?
- How did you break the news to loved ones?
- Treatment Decisions
- Chemotherapy and Side Effects
- Integrative Medicine Practices
- Turning to holistic treatment for side effects
- What was the plan the integrative medicine doctor gave you?
- Describe the personalized nutrition plan
- Acupuncture for fighting nausea
- The mind-body connection
- Using guided imagery
- Additional holistic practices are part of your routine
- What was your follow-up protocol?
- Hair Loss
- Quality of Life Reflections
- Describe how you approached fertility preservation
- Describe the IVF egg freezing process
- Were there moments you had to advocate for yourself?
- Taking care of your mental health
- How important was it having caregivers?
- Were you able to keep working through treatment?
- How has it been navigating survivorship post-treatment?
- What's your last message to other patients and caregivers?
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
1st Symptoms & Search for Answers
How did you know something was wrong?
It was September, and I had begun a 4-month trip in which I planned to travel through Europe before settling in Rishikesh, India, to volunteer for 3 months.
My first symptom began as a slight itch on the lower half of my legs and feet. After just a few weeks, the itching grew more intense. Following the advice of numerous doctors and pharmacists, I treated it with over-the-counter topicals, but nothing seemed to work.
By month 2, the itching was almost unbearable. It kept me up all night and consumed me during the day. I was desperate for relief. I visited a local doctor, who performed a thorough examination and ordered numerous blood tests.
He ultimately attributed the itching to scabies, for which he prescribed me the gold standard treatment.
Unfortunately, no matter how many times I applied this harsh medication, the itching remained. It wasn’t scabies.
You turned to holistic medicine for answers
Frustrated that I had no answers, I decided to pursue holistic medicine options. I was in Rishikesh, after all, also known as “the yoga capital of the world.”
I worked with a yoga teacher, met with a healer and tried various ayurvedic practices on a weekly basis. I learned a lot about holistic treatments during this time, but unfortunately, nothing worked to rid me of my discomfort. I was miserable.

The search for answers
Upon returning home from the trip, I immediately dove into the daunting task of searching for a diagnosis. I visited at least 10 different doctors and specialists, sought advice from friends and family in the medical profession, and spent an inordinate amount of time researching my symptoms on the internet.
I prepared a thorough 3-page document listing all of my symptoms, the timeline of their onsets, and included photo evidence of everything visible. I brought this document with me to every appointment, hoping that if I could provide the practitioner with enough information, they would be able to diagnose me.
Unfortunately, after countless appointments and being told repeatedly that I was fine, I was still without a diagnosis. I was crushed and discouraged.
I finally gave up my search after one specialist told me that my symptoms were likely in my head. I decided instead to shift my focus to learning how to live with my symptoms.
In an effort to move on with my life, I accepted a temporary work opportunity in Tulum, Mexico, where I planned to spend my free time pursuing a healthier lifestyle that I hoped would help me to cope with my symptoms.
After a couple of months in Tulum, I went for a deep tissue massage. It was after this manipulation that a massive bump surfaced near my clavicle. It was alarming and prompted me to immediately book a flight home and schedule another visit with my primary care physician.
Describe the visit with your primary care physican
Upon meeting with him, it was clear that he was concerned. He informed me that the bump was actually a lymph node, and he said that he could feel at least 2 masses.
His tone had changed drastically since the last time I had seen him. It was during this appointment that I finally felt heard by a doctor and validated in my concern for my symptoms.
It was here that I realized the importance of becoming my own fiercest advocate.
I finally understood the hands-on role I would need to assume in my own diagnosis, which began with vowing to never silence my body or my instincts again. It wasn’t all in my head; something was very wrong.
The Path to Diagnosis
Describe the ultrasound
The first test ordered by my primary care doctor was an ultrasound of my lymph nodes. This was a quick and easy procedure, and to my surprise, I got my results back the same day.
Unfortunately, I still didn’t have any answers. Rather, these “results” indicated that I would need to undergo a fine needle biopsy of the largest clavicular lymph node.
Describe the fine need aspiration (biopsy)
This procedure was also quick, but not as easy as the ultrasound. It was more painful than I had expected, and it took the technician multiple attempts to get a good sample. The area was sore for 4 to 5 days.
Before I left the appointment, I was told I would receive my results in a week. This timing was perfect because I had a 1-week vacation to Cabo San Lucas scheduled for the next day and was looking forward to a break from this stressful experience.
However, before boarding my flight, I received a call from my doctor informing me that the results of the needle biopsy were inconclusive but indicative of a “more serious issue.”

Next steps: surgical biopsy
He urged me to schedule a surgical biopsy as quickly as possible. I pressed him for more information. He finally informed me that the results indicated that it could be cancerous, but that I would need a surgical biopsy to know for sure.
Hearing this was shocking and terrifying. I immediately called to schedule a pre-op appointment with my surgeon. The earliest opening wasn’t for nearly 2 weeks, so I decided to still go on the trip with hopes that it would take my mind off of this uncertainty.
I didn’t feel that my doctor was being totally transparent with me, so I signed a medical release form before departing the country, which authorized my mother to pick up copies of my test results.
How did you get the initial cancer diagnosis?
3 days into my trip, I received a call from my mom. With my permission, she had shared my fine needle biopsy results with my uncle, a neurosurgeon.
His interpretation was less ambiguous than my doctor’s had been. “Uncle Barry says it’s Hodgkin’s lymphoma,” she told me over the phone. “He says you’ll definitely need the surgical biopsy for a full diagnosis of the subtype but that the pathology is pretty conclusive.”
That was how I learned that I had cancer. From my mother, while on vacation in Mexico.
A family of medical experts
To many people, this might seem like a strange way to find out that you have cancer, but it actually felt fitting to me, especially given my family’s history.
My grandfather was one of the top physicians of his time, and many of his children and their children went on to become doctors, too. My extended family includes a neurosurgeon, an oncologist, a radiologist, 2 psychiatrists, a general surgeon and 2 primary care physicians.
This was a huge blessing and gave me the invaluable advantage of always having someone capable and willing to double-check my doctors’ work. Their support was truly invaluable.
However, coming from a family of medical doctors also led to some harsh realizations. I learned rather quickly that doctors do not have all the answers. Yes, they may be in charge of your care, but they do not know everything about your cancer, about your treatment, about your body or even about the side effects you will inevitably face.
I was made painfully aware of this when neither my personal physicians nor my family members could answer many of my most pressing questions about my diagnosis:
- How did this happen?
- Why did this happen?
- How can I change my lifestyle to make sure it never happens again?
- What is the optimal diet to best support my recovery?
- Will acupuncture help?
- Will holistic medicine hurt?
My mind was reeling and full of unanswered questions. Realizing and accepting early on that doctors don’t know everything allowed me to take ownership of my healing journey and motivated me to seek my own answers, answers that would help me make sense of this nonsensical thing.
This mindset helped me tremendously throughout my treatment and further reinforced the need to be my own fiercest advocate.
Describe the surgical biopsy
Upon returning from the trip, the days leading up to the surgical biopsy felt surreal. It was as though I was going through the motions of someone else’s life.
I was living in limbo and felt completely paralyzed from making any sort of forward progress.
When I arrived at the hospital on the day of the biopsy, I had a defeated mentality because I already knew what the outcome would be. During the biopsy, they removed an entire lymph node from my clavicle.
For the next 3 to 5 days, I slept about 18 to 20 hours every day — more than I had ever slept before. Removing that single lymph node resulted in a level of fatigue that I couldn’t have even imagined.
When did you get the full, official cancer diagnosis?
5 days after my surgical biopsy, on August 13, 2018, I received my official diagnosis: Classical Hodgkin’s lymphoma, nodular sclerosis subtype.
That same day, I got my first PET-CT scan in order to determine the stage of my disease.
How did you process the Hodgkin’s lymphoma diagnosis?
Initially, I was in complete and total shock. All I could bring myself to do was sit on the couch and watch reruns of the television show “Friends,” because my brain was unable to process how a healthy, active, 26-year-old like myself could suddenly develop cancer.
It certainly didn’t help that society’s interpretation of the word “cancer” is both dire and alarming. I quickly found myself questioning my mortality and all of my life choices.
Was there something I could have done to prevent this? It was all very overwhelming and felt like an impossible emotional mountain to climb, so I didn’t. I just sat on the couch and watched “Friends” until the shock wore off.
Surprisingly, there was also an element of relief. For 8 long months, I had been suffering from this intractable itching. It drove me crazy, adversely affected my mental health, and prevented me from living any type of normal life.
Not knowing what was wrong with me was much worse than knowing I had cancer. Because of that, I actually found gratitude from my diagnosis.
Yes, I had cancer, but at least my pain now had a name. At least no one thought it was all in my head. It was real, and it was treatable.
I realized that my circumstances could be worse in so many ways. With that profound realization and newly developed gratitude, I found hope.

How did you break the news to loved ones?
Breaking the news to all my loved ones was an extremely exhausting process, both emotionally and physically.
By the time I received my full diagnosis, fatigue had become a major symptom, and I found that each emotionally draining conversation I endured would physically exhaust me as well. I began the process of telling my loved ones but found that each conversation was more tiring than the last.
Repeating myself over and over, while simultaneously trying to address the fears and concerns of my loved ones, became extremely daunting. Eventually I realized that I needed to stop.
After the most important people knew, I shifted my approach to waiting to tell people whenever they happened to reach out to me. Surprisingly, this experience taught me a very important lesson in how to protect my energy.
The more I expended my limited energy on emotionally difficult conversations, the less I was able to conserve and utilize on my own internal healing.
I learned to honor my energy levels and the limitations that they presented.
Treatment Decisions
How did you decide where to get medical care?
Based on the recommendations of my doctor and surgeon, I met with a highly regarded oncologist who worked at a publicly-funded hospital in the suburb where I grew up.
During our first visit, after reviewing my PET/CT scan, she determined my cancer to be somewhere between stage 2 and stage 4. She explained that in order to get a definitive staging, I would need to complete a bone marrow biopsy. I agreed to the procedure right then and there in her office.
Describe the bone marrow biopsy
I underwent the most painful procedure I had ever experienced. She had certainly downplayed what I should expect, and I resented her a bit for that.
The good news was that results of the bone marrow biopsy came back negative, resulting in a stage 2 diagnosis.
What was the stage 2 treatment plan?
The oncologist then presented me with the following treatment plan:
- First, 4 rounds of ABVD chemotherapy
- Next, a PET-CT scan to determine if I had achieved remission
- Finally, possible radiation afterwards (depending on results of the PET-CT)
Did you get a second opinion?
I was quite thrilled with the stage 2 diagnosis and relatively short treatment plan laid out by the oncologist, because I was terrified of chemotherapy and wanted as little of it as possible.
However, it was very important to my family that I get a second opinion, so I used every resource available to me and was lucky enough to secure an appointment with one of the best local specialists.
Unfortunately, because he was in such high demand, his first available appointment was a month away. I decided to delay treatment and wait for the appointment because my research informed me that Hodgkin’s lymphoma is a slow-growing cancer and that a 1-month delay wasn’t cause for concern in a stage 2 case.
The diagnosis changed from stage 2 to stage 4
By the time the second opinion appointment arrived, I was feeling sicker than ever and eager to move the process along.
After his team reviewed all the same test results and scans ordered by my first oncologist, they definitively determined that I had stage 4 cancer.
This came as a huge shock. I found myself trying to argue my way into a stage 2 diagnosis, but the doctor remained firm. In his opinion, it was an absolute stage 4 despite the negative bone marrow biopsy, and his reasoning was thorough and well founded.
In fact, he believed that the bone marrow biopsy had been an unnecessary procedure altogether, and he apologized that I had to endure it. Stage 4 wasn’t what I expected or wanted to hear, but he was confident and firm in this diagnosis.
I now had 2 highly regarded oncologists offering me 2 very different paths. The new diagnosis was 2 stages higher, and the treatment plan was 2 months longer than that of the first oncologist.
Despite how badly I wanted to take the easier route, I didn’t. This was primarily due to the unique and dynamic treatment plan proposed during my second opinion appointment.
He wasn’t simply following the status quo of how most doctors treat Hodgkin’s lymphoma. The thoughtfulness of his plan made me more confident in what laid ahead, so I switched oncologists immediately.
Without a doubt, I believe that delaying my treatment by a month in order to get a second opinion was the best and most significant medical decision I made during my entire cancer journey.
Describe this different treatment plan
Regardless of staging, nearly every case of classical Hodgkin’s lymphoma is treated in the same way: the ABVD chemotherapy regimen and possible radiation, if necessary.
The ABVD regimen has been the standard first-line course of treatment for Hodgkin’s since the 1970s. Unfortunately, there have been few medical advancements made in the 40 years since then.
What impressed me about my new oncologist’s unique approach to this standard treatment was its dynamicity.
It involved a mid-treatment PET-CT scan to determine if it was possible to downgrade the chemo regimen from the classic ABVD to a less intense AVD, thereby dropping the “B” (bleomycin) after just one of the 6 cycles.
His reasons for using this approach were scientifically founded and backed by recent studies. Additionally, they were logical to me, the layman.
Bleomycin is one of those “nasty” chemo drugs that can have detrimental long-term effects on your lungs. The less of it your body has to endure, the better, and his treatment approach was very mindful of that.
He felt the same way about radiation and informed me that it was his intention to avoid using any radiation during treatment unless it was the last remaining option. It was clear to me that he was extremely knowledgeable about the negative effects of Hodgkin’s lymphoma treatments.
As such, his treatment plan balanced the important task of destroying the cancer cells with the additional goal of avoiding as many long-term chemo side effects as possible.
»MORE: Read more patient experiences with bleomycin
How was your medical team?
Unlike the first oncologist I met with, the one I ultimately chose worked at a university research hospital. Being a patient at a research hospital meant that my medical care team had expanded.
It wasn’t just me and my one doctor anymore. I now had an entire care team assigned to my case, which included my primary oncologist, an oncology fellow, a symptom nurse, a pharmacist and a psycho-oncologist.
The entire team was located in the same office, which also housed the chemo infusion center and the blood analysis laboratory. It was a one-stop shop, and the team-based approach gave it a much more collaborative feel than that of the publicly funded hospital.
Chemotherapy and Side Effects
Describe getting the port pre-chemo
Having a port inserted in my chest was one of the pre-treatment procedures required by my oncologist. Initially, I tried to convince him otherwise, because I wanted to avoid any unnecessary procedures. My prior oncologist hadn’t required that I have one.
However, he explained that 6 months of chemotherapy involved a lot of IV insertions, and the small veins in my arms would likely become weak over time. I hesitantly agreed.
Inserting the port was a more difficult procedure than I was expecting, primarily because I was not fully sedated. Towards the end, the medications had worn off completely, and I was fully awake as the doctors applied a great amount of physical force to move the port into the correct position.
I was sore for 3 days following the procedure, and it took me several weeks to get used to having a foreign device under my skin.
With that said, over the next 6 months, I grew to genuinely appreciate my port.
I believe it made every individual experience at the infusion center more pleasant not only for me, but also for the nurses who were responsible for inserting my IVs.
Getting the port removed 8 months later was a very simple and painless procedure, not at all like the insertion procedure.
All in all, I would recommend getting a port or similar device for anyone facing a lengthy chemotherapy treatment.

Describe the ABVD and AVD chemo regimens
My first ABVD chemo infusion was on October 4th, nearly 2 months after my diagnosis. The plan was for me to undergo 6 cycles over 6 months, which totaled 12 individual infusions, 1 every 2 weeks.
My chemo day was Thursday. For the first 2 rounds, I received the ABVD chemo regimen. Then I did an interim PET-CT scan, which luckily showed that the treatment was making enough progress to downgrade my ABVD regimen to an AVD regimen for the last 8 infusions.
»MORE: Read our comprehensive ABVD chemotherapy info page
What were the cycles like?
In the beginning, I didn’t know what to expect, and Google was no help. I approached the situation feeling unprepared and emotionally unstable.
However, the first infusion surprised me in a couple significant ways. First, I was shocked to realize that the itching symptom, which had been tormenting me for 13 long months, was suddenly gone. It disappeared that quickly, after just 1 infusion.
Experiencing this relief helped shift my perspective from ‘chemo is poison’ to ‘chemo is medicine’ for the first time.
The second surprise was that I didn’t feel the effects of chemo right away. Upon returning from the first 6-hour infusion day, I felt tired and a little nauseous, but I was otherwise okay.
However, this didn’t last long. The next morning, I could feel the side effects getting worse, and I was overwhelmed with nausea and other discomforts. These side effects continued to worsen in the days following.
Eventually, the side effects peaked about 3 to 4 days after the infusion and then progressively got better. About a week after each infusion, I would wake up feeling ‘recovered,’ which I referred to as ‘climbing out of my chemo hole.’
It was the best part of every round because it left me with approximately 7 blissful days of feeling “normal” before the next round began

What were all the different side effects you felt?
My side effects came in waves and got progressively worse over time. My primary side effects were:
- Extreme nausea
- Stomach pains
- Fatigue
- Sensitivity to light
- Shortness of breath
- Strong aversions to certain smells
- Mouth sores
- Disorienting dizziness
How did you combat the side effects?
After the first infusion, I began to experience extreme nausea, stomach pains, fatigue and sensitivity to light. I combatted the nausea with acupuncture and by preventatively taking anti-nausea medications around the clock, before the nausea even began.
I decreased the stomach pains by following a strict diet and supplement plan. I addressed the fatigue by sleeping as much as possible. I dealt with the sensitivity to light by wearing extremely dark oversized sunglasses whenever light caused me discomfort, including inside.
»MORE: Read other cancer patient experiences with chemotherapy
By the second infusion, I was immunocompromised, which means that my immune system was compromised. I had to be extremely careful not to catch a cold or flu, because my immune system did not have the strength to fight off even the tamest of invaders.
I protected myself by wearing masks in public, applying hand sanitizer regularly, and limiting the number of people I came into contact with. I also developed shortness of breath, which was likely caused by the bleomycin.
By the third infusion, I was experiencing a nauseating metallic taste in my mouth and had developed an extreme aversion to certain smells. I sucked on ice cubes and sniffed essential oils to combat these discomforts.
I also developed a strong aversion to saline, which is the fluid the doctors inject patients with every time they insert an IV prior to starting a round of chemotherapy.
Though most people can never taste or smell saline, the aversion made me feel instantly nauseous every time I was injected with it. Strangely, I could even taste it in my mouth as it was being injected into my port.
Sniffing essential oils while the saline was being injected helped tremendously with this, although initially I made the huge mistake of only using one scent, lavender. Because of this, I slowly developed an aversion to lavender.
Even to this day, too much lavender can make me feel nauseous. After developing the lavender aversion, I realized that rotating essential oils was the best way to handle the saline aversion so that I wouldn’t develop any more new aversions in its place.
By the fourth infusion, I was experiencing mouth sores and had begun to feel dizzy whenever I stood up too quickly.
Following my dentist’s instructions, I used Biotene mouthwash for the sores and switched to a dentist-prescribed sodium fluoride toothpaste.
As for the dizzy feeling, I simply had to learn to get up very slowly. The more mindfully I moved, the less disoriented I felt. The yoga, meditation and breathwork practices helped me tremendously with this.

Did the cycles get better or worse?
By the end of the first 2 infusions, or the first cycle, I began to notice a pattern occurring in each 14-day round. Every round seemed to be similar, though more intense, than the last one.
By figuring out this pattern, I realized I could proactively work to decrease certain symptoms before they arrived.
This was when I began to build a holistic treatment plan with the intention of preventatively combatting my chemo symptoms. The goals of this holistic plan were to:
- Decrease the severity of my chemo side effects
- Keep my immune system strong throughout my 6-month chemo journey
- Remove all miscellaneous toxins (i.e. sugar, alcohol and stress) for the duration of my treatment to allow all of my healing energy to be focused solely on combating the cancer cells and coping with chemo
I followed my holistic treatment plan closely and mindfully, and I truly believe it made a significant impact on the outcome of my journey.

Integrative Medicine Practices
Turning to holistic treatment for side effects
Establishing and following a strict holistic treatment plan was the method that helped me the most, but building the plan was a journe








