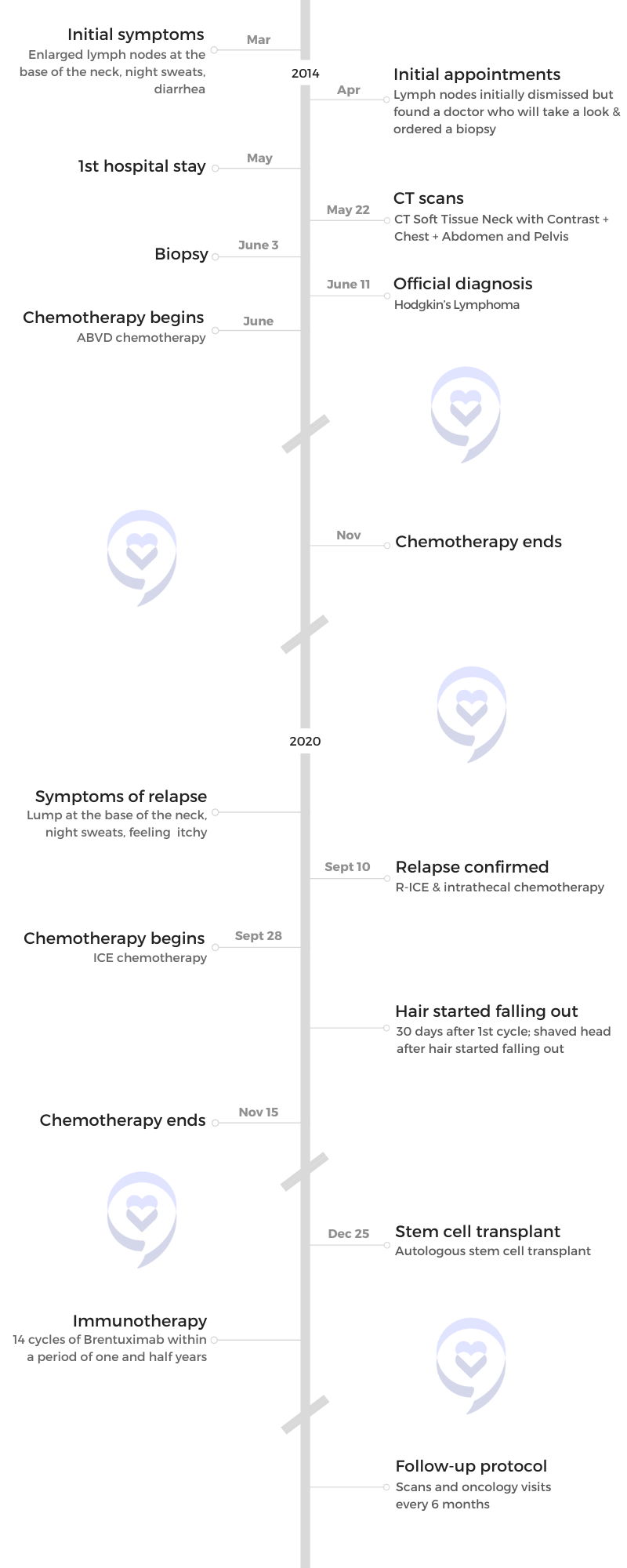
Emmanuel’s Relapsed Hodgkin’s Lymphoma Story
Emmanuel S., Relapsed Hodgkin’s
Symptoms: Enlarged lymph nodes
Treatments: Chemotherapy: ABVD, ICE; autologous stem cell transplant; Targeted therapy: Brentuximab
Emmanuel’s Relapsed Hodgkin’s Lymphoma Story
Emmanuel was diagnosed with Hodgkin’s Lymphoma at 24. After having his symptoms initially dismissed, he was finally able to find a doctor who told him to do a biopsy.
He shares his experience with relapse, doing chemotherapy twice, undergoing a stem cell transplant, and how his “go go go” attitude and positive mindset helped him.
- Name: Emmanuel S.
- Initial Diagnosis:
- Hodgkin’s Lymphoma
- Initial Symptom:
- Enlarged lymph nodes at the base of the neck
- Night sweats
- Diarrhea
- Initial Treatment:
- ABVD chemotherapy
- Relapse:
- Night sweats
- Scratchy and itchy
- Lump at the base of the neck
- Treatment:
- Chemotherapy: ICE
- Autologous stem cell transplant
- Targeted therapy: Brentuximab
[It’s] important to have something to look forward to. I had that and that saved me. It gave me all the power that I needed for the day-to-day battles to just get through it.

This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
The first thing that I thought was “Oh, this is cancer.” But I never said it out loud. I knew that could scare people.

Pre-diagnosis
Initial symptoms
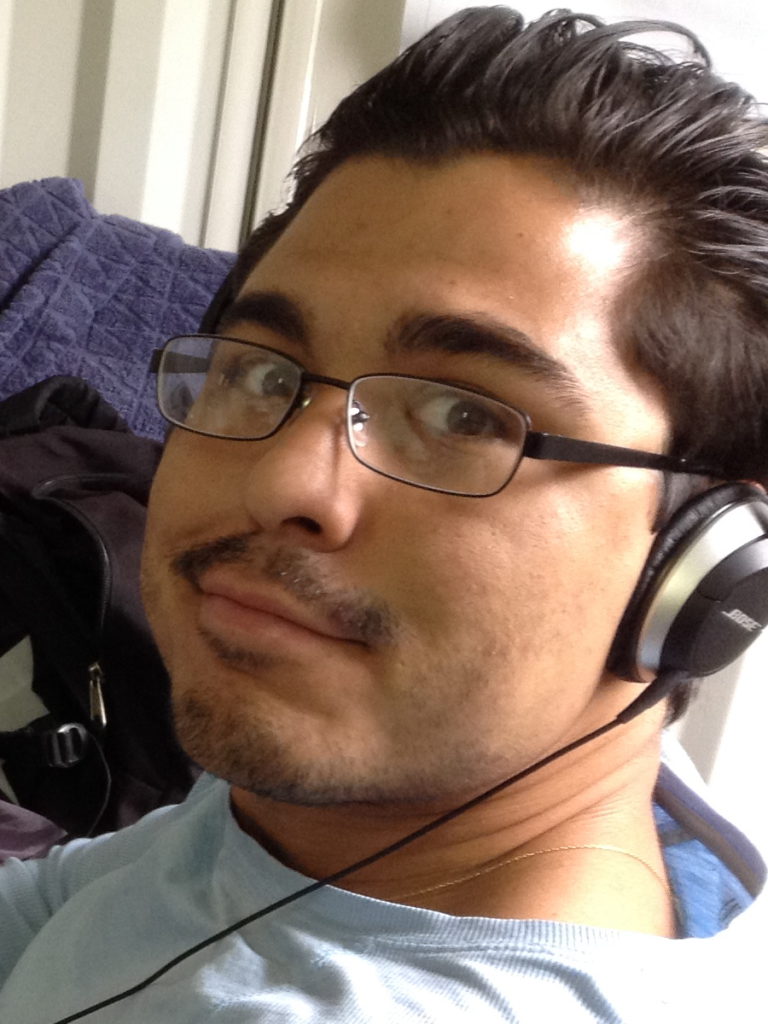
The first time I was diagnosed, I was 24.
I was in the mall and I put my hand [on the base of my neck]. “What are these three little balls? What are they doing here?” The first thing I thought was “Oh, this is cancer.” But I never said it out loud. I knew that could scare people. “I don’t know what it is. It feels weird.” But in my mind, I was [thinking], “Is this cancer?” I never saw anything about it, never researched anything about these lumps.
As time went by, I went to see a general doctor and they just blew it off. “Sometimes we get these lymph nodes that get swollen.” A few doctors later, [he] said, “Nodules at the base of the neck [are] no good. [Under the jaw] is okay, but the base of the neck is where you should be worried.”
Sometimes you see a few doctors and you think everything’s okay, but there’s always that one person [that] says check it out.
Deciding to get a second opinion
I came out of a really bad sore throat and cold. I also was having a lot of night sweats [and] a lot of diarrhea. All of that kind of put me in doubt. Sometimes you see a few doctors and you think everything’s okay, but there’s always that one person [that] says check it out.
Getting a biopsy done
The doctor told me to do [a] biopsy. I [initially thought] he just wants to [refer] me to his friends. I ended up doing the biopsy. It was a little nerve-wracking.
[It was] the first surgery that I had to do. I had to go under the knife. I had to go to sleep. It was funny because when I woke up, nobody told me anything.
My grandmother took me out to lunch and then she started crying. “What’s happening?” She’s like, “Oh, we don’t want to tell you.” [I thought it was] messed up. How can you not tell me?
They told me this at lunch with my grandmother and it was a bit of a shock for me. I [had] mixed feelings. She held it from me for [about] an hour. They said I wouldn’t have the results in a few days. That was a twist in the story.
I decided not to research too much. You can go online [and] find a lot of things.
Diagnosis
Finding out about cancer
I didn’t hear the word cancer at all. When you talk about Hodgkin’s lymphoma, people don’t say the word cancer. People stay away from it. I didn’t even know it was cancer until I was maybe a week into it.

When I actually started hearing the word cancer, I started getting more worried. Now I understand. This is cancer. From there, I just had to buckle up.
I also decided not to research too much. I don’t want to brainwash myself before I got started. I think that’s important also for anyone just to not get overwhelmed. You can go online [and] find a lot of things.
In the beginning, I [just wanted to] take it easy. There’s nothing you can do. Just swallow everything. Try to understand what’s going on.
But when I actually started hearing the word cancer, I started getting more worried. Now I understand. This is cancer. From there, I just had to buckle up.
Having to be emotionally strong
I’m the oldest of all of my brothers and everybody. I had to play it strong. I never showed my weakness to my mother [or] to anybody. I always had to show off like I was strong and it worked. I’ve been able to fool everybody since then… In a good way.
It’s hard to explain. As the oldest, you have to be strong in front of everybody.
As a guy, I guess I couldn’t show too much emotion. But that’s completely wrong, right? I should be able to cry and be sad.
The moment you get a diagnosis like [cancer], people don’t know what to do. They’re afraid to say something to offend you.
I took all this energy and [channeled] it in a way that I could just focus on what I had to do. At that moment, I had a big dream, which is to sail around the world. I have to finish all of this to sail around the world. That was the only objective. Nothing’s in my way.
In general, as a human, I feel like that was the first time I felt alone because it’s honestly like that. When you go into the hospital and you’re laying down to do a biopsy, you have nothing but the [hospital] robe. You don’t have a phone, you don’t have your wallet, you don’t have anything. You’re by yourself. They put you in that room and you’re just waiting there just to get surgery. This is it. I’m by myself.
This is like life. Come in by yourself, you go by yourself. I think that was the first time I felt alone and felt like this is my own problem. I hope people around me can make it easier for me.

How to talk to someone with cancer
It’s hard because the moment you get a diagnosis like that, people don’t know what to do. They’re afraid to say something to offend you. I’m an open book most of the time.
It’s hard for other people to understand how [to] approach someone. What can I say? Should I say cancer? Should I not say cancer? Even today, people say, “Can I say cancer?” Yeah, it’s cancer. It’s no big deal but I have to respect other people. It’s tough.
You have to have someone to talk to [and] open up [with]. You can also strengthen your mentality to go in a positive direction.

Getting emotional support
At the moment, I had a [life] coach so I think this helped me a lot. They could be a life coach, could be a psychologist.
Sometimes the male figures in our lives are not so present so we don’t have someone to talk to and normally the person who’s going to listen to us is a female — our mom or our girlfriend. Mostly, we don’t have the opportunity to open up with another guy.
They don’t also give us incentives to open up as well. If you told me, I’ll give a message to a young man, I’ll say, “Be strong and don’t cry,” because that’s what it is. I would tell him that because that’s what it is.
But at the end of the day, you have to have someone to talk to [and] open up [with]. You need someone to help you organize your thoughts and construct your reality. It’s super easy to base all of this information on a false reality, which is I’m going to die.
You can also strengthen your mentality to go in a positive direction. We’re here one day at a time.
Getting the official diagnosis
[In] the beginning, I was scared. I was really scared so I didn’t want to understand anything. I was like, “Alright, let’s just do it. You guys tell me what I’m going to do. I’m going to come here. What is it? Every week? Every other week? We’ll get it done and I’ll leave.” That’s it. I didn’t want to know.
Treatment
ABVD chemotherapy
I did IV every time. It’s tough because you’re going to get poked [and] sometimes they wouldn’t get the right spot. It’s not fun.
There [are] a lot of things that they told me I could do, which is having a cleaner diet [and] drinking a lot of water. All of this I was actually doing. I went full on with it.
I went on [an] alkaline diet. I started eating less meat, less sugar, [and] less milk — all of this stuff to help me. In my mindset, it made me stronger. I was able to go into chemo day [feeling] good [and] ready to go. It’s like a battle. I was ready.
Then there are some days that they just poke me the wrong way. It’s tough but it’s part of it. Just try not to anticipate the pain.

I just was so positive [about] everything. This is not it. I have so many things to do.

Side effects of chemotherapy
The first thing [usually] is hair starts falling out, right? All my hair didn’t fall out. That’s funny because I told the doctor, “Doc, all my hair is not going to fall out.” He goes, “Alright, let’s see. Let’s see.” My hair didn’t fall out, so I was happy about that.
I just was so positive [about] everything. This is not it. I have so many things to do. It’s okay. I’m behind. I got to go. That was my mindset. I was so strong in my mindset.
Mouth sores [are] a pain. But then through searching and looking at so many other people’s stories, I saw the Biotène toothpaste. They have a whole line of all the Biotène products, which is great. I don’t know if there [are] any other products that are more natural that can prevent cold sores, which is what was really helpful. I don’t even remember having the mouth sores until I saw a video that I filmed.
[I had nausea] all the time. It was horrible but it’s something you can get through. I remember the first chemo I did. I went back home and slept for four or five hours. When I woke up, I went downstairs and my stepdad said, “What were you doing?” I go, “I was sleeping.” He goes, “You better not ever do that again. You got to live your life normal.”
He’s right. What am I doing coming home and just crashing? I was exhausted and that’s okay. You can go home and take a nap. But he’s right. How am I gonna come home and just lay down and sleep?
I don’t remember [taking any medication for nausea]. I was trying to fight it off, just trying to be a tough guy.
I didn’t read anything. Again, I really was kind of ignorant. I think that was my only thing. If you can go back in time, just make sure. This is only for some healthcare professionals but not everybody is always on the ball and not everybody always knows what’s going on. These nurses have a lot of patients. Sometimes they can get confused. You need to be on top of your stuff. I know that I have to take this and I shouldn’t take this. I think that’s one of the things that I would have changed.
I’m a little bit eight or I’m 80. I’m kind of extreme. I should find a middle balance, maybe find out about some side effects. I did with the Biotène and certain things, but there [are] some other moments I should have learned a little bit more.
Adopting a healthier diet
On those days, I would buy water with more pH. I had this whole mindset that I got to drink water that has a high pH, drink water with lemon, and all [these] nuts and healthy foods. I was into that.
I didn’t have meat, sugar, milk, [and] alcohol. I literally cut all that out of my life. Every morning, I was doing these green shakes [with] beet juice, beets, carrots, celery, and kale. I had all that and I drink it every morning. Part of me [thought it] would help fight off nausea and maybe just fight off some of the cancer.
My whole life became focused on what’s going to go inside my body and what I can do to control it.


Taking care of myself
I compete against myself all the time. I’m always pushing myself. I’m highly dedicated and over passionate about everything.
When this became my full-time job, taking care of [myself] and just [making] sure [I] can see the next corner that’s coming up, I just [focused] all my energy on that [and] just trying to get better.
I really [focused] a lot of time, energy, and even money on food because food is expensive, especially going organic as much as possible on certain foods. I started doing a lot of research and then my whole life became focused on what’s going to go inside my body and what I can do to control it.
The day they told me, I was stoked because it was my dream to visit Antarctica.
Remission
Getting the all-clear
It’s tough because one thing they tell you is you go into remission. Once you finish, they don’t give you the cure label. They give you the remission label, which is horrible. What’s going on?
It’s like giving you a possibility of a window. Maybe something’s going to come back. Why? When people start saying things, I just disregard [them] entirely. “Oh, no, you could get cancer again.” Disregarded. I’m not going to take that. I don’t need that but it’s a possibility. I might as well just keep my mind clean.
The day they told me, I was stoked because it was my dream to visit Antarctica. My mother [said], “No, you’re only going to go to Antarctica if the doctor allows you to go.” When I asked the doctor, he said, “You’re good to go. You can go to Antarctica.”
I was super stoked because I didn’t want to miss the trip or the part of Antarctica. I didn’t want to get on the boat too late. That was a great experience. I think something to look forward to overall was really important for me.


There [are] a few places on the planet that I suggest everybody [visit]. One is French Polynesia.
You can buy a ticket once you’re done with your treatment two years out or a year out because it also becomes more feasible to buy such an expensive ticket or go somewhere that you’ve always dreamed of going.
I think that’s going to be something that could help a lot of people. Put it on a credit card or pay in installments and just make sure you have something to look forward to, like a really good trip.
I think that’s something important to have, something to look forward to. I had that and that saved me. That really did save me. It gave me all the power that I needed for the day-to-day battles to just get through it.
Relapse
I had to keep doing the CT scans for the first two years. Every six months and then after that, once a year. I was done with it but, at the same time, I still had to go back.
It was good because every time you go back, you confirm you don’t have anything.
I’m going to show the doctor again that I don’t have anything and that became my game. I’d show the doctor every time that I was good.
The sooner I found out that it’s something or it’s not something, the sooner I can be at peace or I can tackle what I have to tackle, which is super important because time is everything.
Symptoms of relapse
I started feeling night sweats. What was getting me was just getting scratchy and itchy during the week. I started working out [and] I started getting itchy but that’s also normal for some people so don’t freak out if you have this.
I also felt like I had a lump at the base of my neck. It was funny because it was like down, down below so only I could really feel it. Everyone, all the doctors, was like, “Oh, this is nothing. No, need to worry about it. Don’t stress about it.”
I don’t have the best history so I [thought] I should get this checked out. I insisted. I insisted so much that I ended up doing the biopsy, which is great.
What I realized was, in this case, the sooner I found out that it’s something or it’s not something, the sooner I can be at peace or I can tackle what I have to tackle, which is super important because time is everything.
There [are] some people who unfortunately pass away from Hodgkin’s and non-Hodgkin’s lymphoma because I think sometimes, they might be in a denial. They might think that it’s nothing. They might push it off, might be scared. But there’s no excuse for that. Get to tackle it as soon as it appears.


Finding out about the recurrence
I knew it, but I was in doubt. At that moment, I no longer played the positive game because I’m thinking, okay, now I’m screwed. Now, this is it. I’m going to have to do this again. If it is, it is. And if it isn’t, it isn’t.
I’m crazy [because] I think I smiled. I remember my wife, my fiancée at the [time], she was crying, breaking down. [I was thinking] let’s go. Let’s do this. When do we start? Thinking that also that this type of treatment was going to be the same as the first time, which I didn’t lose my hair, I had some mouth sores, and that it was about it.
The second time was two times harder and I had no idea about that. I was all excited [that] it’s going to be easy again. Not that it was easy, but I was happy. I wasn’t like happy happy. I just turned the beast mode on in my mind. Let’s go. Let’s kill this bug.
In the beginning, the first time I was diagnosed, I considered it a bug, like a bug in the program. My dad put that in my mind. You have this bug, you need to fix it. Get the bug out. That’s the way I thought about it. Let’s kill the bug and that’s it. For me, cancer was a bug.
Treatment
Autologous stem cell transplant
That’s where I was like, “Oh no, I don’t want to do any of this. It’s not fun. It’s no beast mode. This is not it. I don’t want this.”
Did I really wish this upon myself? That part was tough. When he told me that I had to do all these things, I was like, “Oh.”
[During] those moments of surgery, I started learning to become at peace with myself, accepting certain things.
Preparing for stem cell transplant
A blur. I don’t know why I don’t focus so much on all these details, but I remember that I had to get certain blood cells to go up. There [were] things that I had to get leveled out. I had to do injections. I had to do a bunch of things. They had to take out blood.
They had to install a different port that had two exits. It was horrible. It was really bad. I don’t think anybody likes the whole feeling of surgery and all that.
[During] those moments of surgery, I started learning to become at peace with myself, accepting certain things. Not death itself, but just this is it. Take it easy. We complicate life so much.
They install a port, connect it to a machine, [and] filter your blood. They collect a bag of your own stem cells [and] freeze that. They send you home. You come in back to the hospital. Then you do [an] official check-in and then that’s when they give you high doses of chemo [and] pretty much shut down your immune system. That’s what everybody gets scared about. But, again, I just put my stuff there with the lucky ones. Nothing can go wrong here. It’s going to be good. Let’s do it.

This was actually during Christmas and New Year’s, so I was really happy, I guess. My whole room was decorated with Christmas stuff. I got presents. I’m going to spend Christmas in [the hospital so] I’ll make it a whole thing, that was my perspective. I had a nice room. I was blessed. I had everything. I had everybody treat me really well. I really can’t complain.
I was in the hospital by myself for 21 days and nobody could go in with me because of COVID protocols.
ICE chemotherapy
When the doctor told me that I had to do ICE, he explained to me that it was going to be much more intense [and] that I was for sure going to lose my hair. I was going, “I didn’t lose my hair last time. Why would I lose my hair this time?” “Well, it’s a little bit different. Take it easy. We have to have you put a port, you’re going to have to do all this stuff.” I was like, oh my goodness, this is going to be a little bit more different. But other than that, my mindset was still the same. Let’s prove everybody wrong. Let’s not lose your hair and all this stuff.
Also, we had COVID going on so it was a lot more annoying because I got to keep doing COVID exams before going to the hospital. It was all good. I really can’t complain.
It was a little bit different from the other treatment. I had to go to the hospital and stay there for five days. I would go into the hospital, check in, do the ICE treatment for 3 to 5 days, and then I would check out. That was horrible because I also have to eat the hospital food and that itself is tough. And dealing with people coming [into] your room all the time.
There I started kind of feeling almost [like] a prisoner. I think that’s one of the toughest things that I felt. When I was doing the chemo, when I was doing the transplant later on, I was in the hospital by myself for 21 days and nobody could go in with me because of COVID protocols. I would look out the window. I remember I was like, “Man, you guys are lucky.” People are waiting, sitting at the bus stop. You can do whatever you want. You can stop and get ice cream. And I’m stuck in here. I can’t do anything. You become a prisoner and you didn’t do anything wrong. That’s tough.


Side effects of chemotherapy
The nausea was what got me the most. But again, I’m really lucky. I sailed around the world for two and a half years. Think of a person who’s used to having nausea because the boat’s always moving. I was so used to it. I thought it could be worse. Again, I’m








