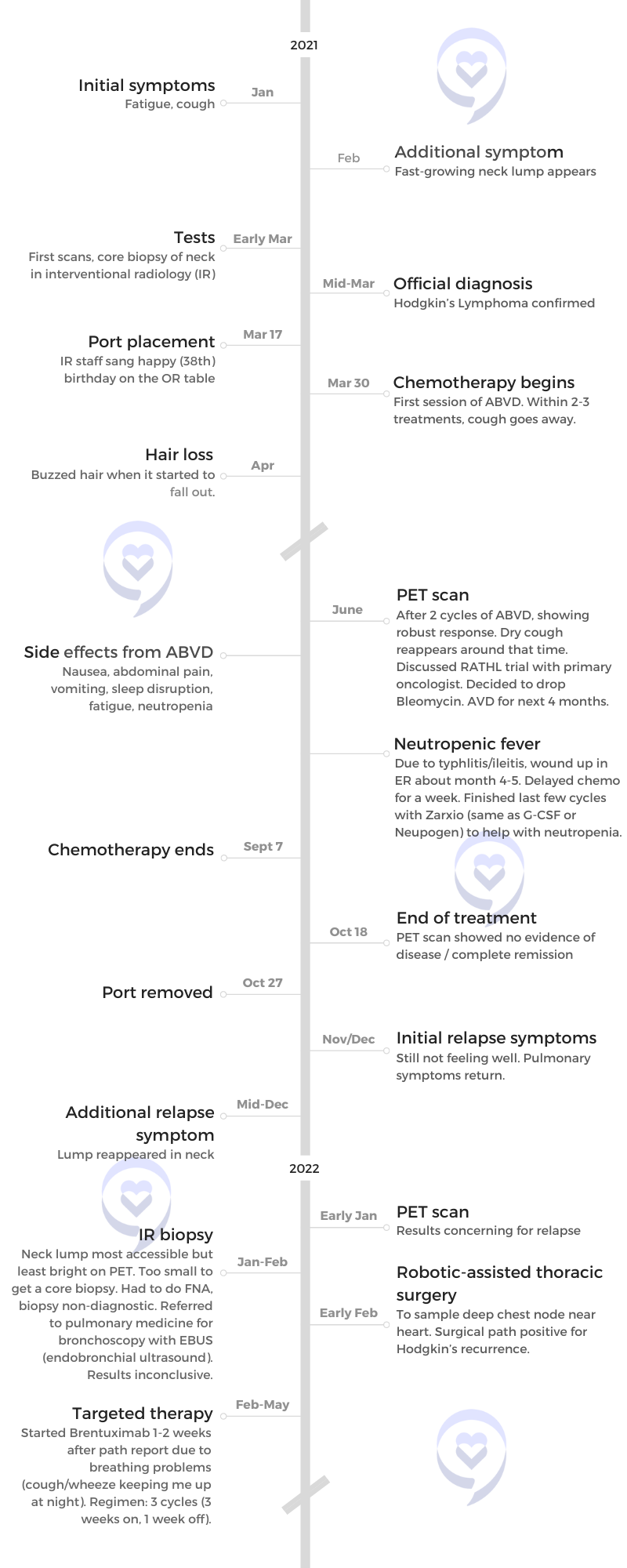
Sam’s Relapsed Hodgkin’s Lymphoma Story
Samantha S., Relapsed Hodgkin’s
Symptoms: Fatigue, cough, enlarged lymph node
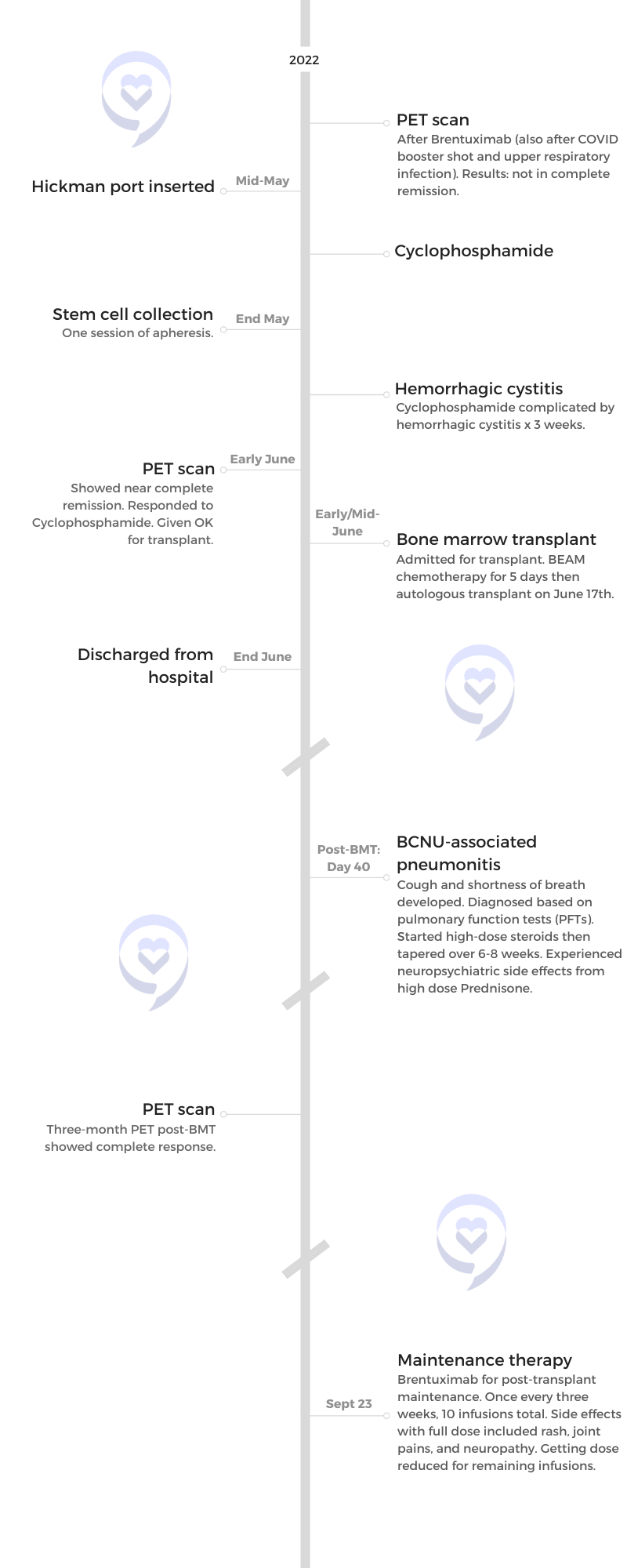
Treatment: ABVD chemotherapy (later changed to AVD), Brentuximab, Cyclophosphamide, BEAM chemotherapy, autologous bone marrow transplant
Sam’s Relapsed Hodgkin’s Lymphoma Story
Sam was diagnosed with Hodgkin’s Lymphoma at 38, which relapsed within a month after ending treatment.
She shares the complications of being a doctor-patient, the importance of being honest with your medical team and having clear lines of communication, and the delicate balance of advocating for yourself.
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
- Name: Samantha S.
- Diagnosis:
- Hodgkin’s Lymphoma
- Symptoms:
- Fatigue
- Cough
- Fast-growing lump above the collarbone
- Treatment:
- ABVD chemotherapy (Dropped Bleomycin after 2 cycles)
- Relapse Symptoms:
- Feeling unwell
- Pulmonary symptoms
- Lump reappeared
- Treatment:
- Brentuximab
- Cyclophosphamide
- BEAM chemotherapy
- Autologous bone marrow transplant
I love my doctors and my healthcare team, and I also need to be able to ask questions about my life

It was so tough in the beginning because it was one year into the pandemic. I was really tired… It was such a hard time [with] so many hats to wear so I just discounted my fatigue
Pre-diagnosis
Introduction
I am a mom of three adorable kids ages four, nine, and ten — almost 11. My husband is amazing. We’ve been together since before medical school. We’ve been buddies since the beginning.
I’ve been a long-distance runner for many years. I love jogging, running, baking, hiking, playing guitar, and painting. Some of those things I did later on when I had my transplant at Stanford Hospital.
I love being a doctor in my community, too, when I’m feeling better.


Initial symptoms
It was so tough in the beginning because it was one year into the pandemic. I was really tired, having trouble getting past 8 o’clock at night with bedtime and bath time, and then getting back to patient notes after the kids were sleeping. I thought, Every doctor is tired right now, especially doctor parents and even just parents that are homeschooling their kids during the pandemic. It was such a hard time [with] so many hats to wear so I just discounted my fatigue. That went on for maybe a month or so, maybe two months.
I also had a cough, predominantly at nighttime. There had been some wildfires in the area where I live. I had a ton of excuses for why I was coughing. I’d be coughing so hard that I slather myself in Vicks VapoRub and take steamy baths in the middle of the night to try and calm my breathing down, thinking, I must have some kind of asthma or reactive airway. All these justifications [for] why I wasn’t feeling well and have these symptoms.
I started getting a rock-hard, rapidly growing lump right above my collarbone. Then I knew. I even said to my husband when I started to feel it, “I think I have lymphoma.” I specifically said lymphoma. It was just so classic to me in my mind.
Shortly after, I put it all together — cough, fatigue, and this lump. This doesn’t feel like a benign lymph node. This feels like I have a rock that’s coming up above my collarbone into my neck area.
Within a week, there was a difference in [its] size. It just had all the features of a lump that’s concerning. A lot of people don’t have rock-hard lumps — they have more rubbery lumps — but I just knew I had to get it checked out.

Shortly after, I put it all together — cough, fatigue, and this lump. This doesn’t feel like a benign lymph node
The process of getting diagnosed
It was really scary. First, finding the time to get an appointment, doing the dance of, “Am I imagining these things? Is this really something worth taking time off work for?” I want to save my sick time for my family and things going on. Logistically, it was tough.
Being a doctor, I knew that I had a left supraclavicular node and I knew exactly which node it was — Virchow’s node. I was hoping that it wasn’t that.
One of my PCPs at the time ordered a thyroid ultrasound saying, “It could be a thyroid nodule; it’s probably [a] thyroid nodule.” In my mind, even though I thought this isn’t, I think they were hoping that it was a thyroid nodule and I was hoping it was, too.
I was able to get a thyroid ultrasound. When I was in the ultrasound suite, the ultrasound tech said, “Your thyroid’s normal,” and I could sense a “but” there. I said, “So what’s going on? Can you just give it to me straight?” She said, “I’m a tech. I really can’t diagnose you with anything but see these?” She turned the ultrasound probe. I looked at the screen and went, “Ugh.” It looked bad, like some kind of tumor or mass. Then I said, “That looks like tumors or masses.” And she said, “Yeah, it does, but I’m not a doctor.” She was very professional, given the situation. It’s so tough.
It looks like tumors…
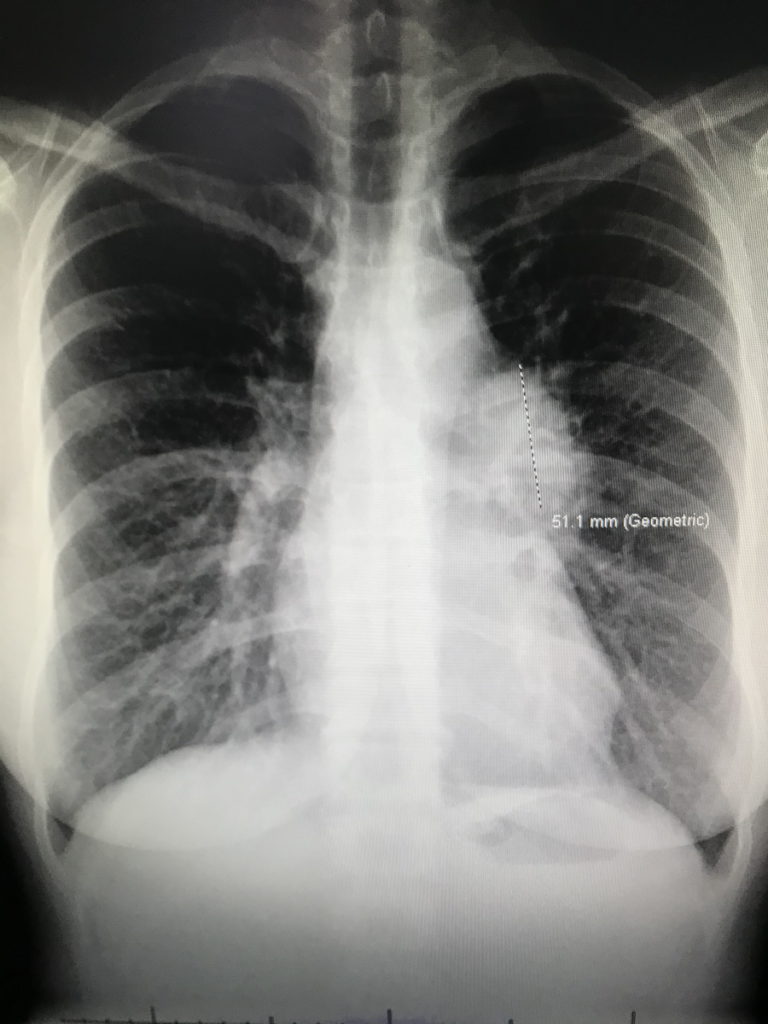
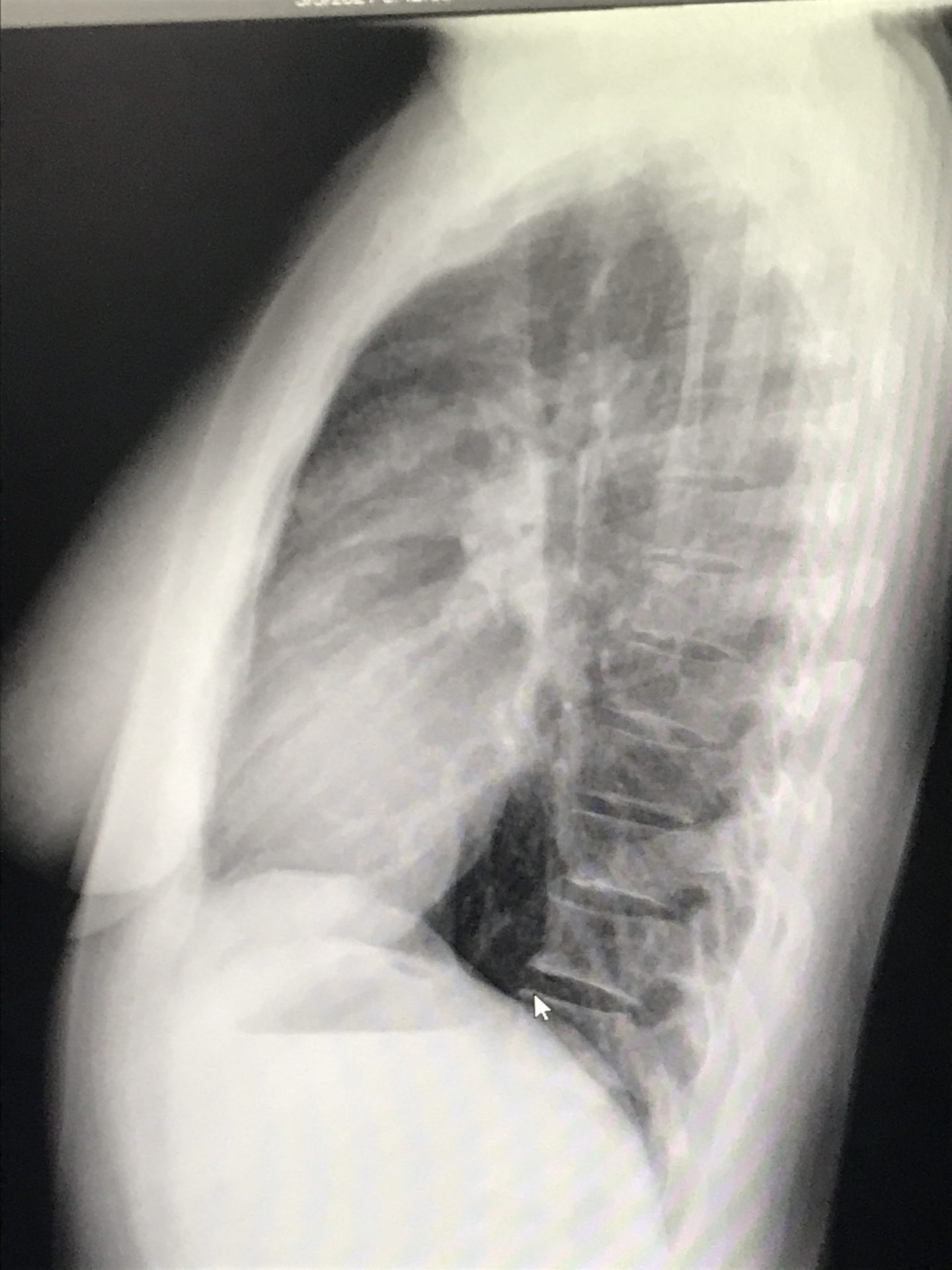
I called one of my friends at work — another doctor — crying on the way home, saying that it looks like tumors. She ordered a chest X-ray for me and I got the chest X-ray before my clinic day. I then went straight to my office, opened my own chest X-ray, and saw that not only were there masses near my collarbone but there were masses in my mediastinum — the middle of [the] chest cavity. It didn’t look right. It was like it was somebody else’s chest X-ray.
I was totally numb. I couldn’t even process that that was mine. I walked into my friend’s office next door — an amazing nurse practitioner — and said, “I think I have cancer. I just opened my chest X-ray and [there are] masses and I have lumps in my neck. I’m pretty sure I have cancer.” I said it with this blank look on my face. Then I said, “Okay, I’ll go see some patients now,” and just went on about my day.
I was completely in shock and happy to focus on everybody else and not myself because that was just terrifying. I saw patients all day and then over the weekend, things evolved. I decided I better take some time to figure out what’s going on with me. I probably shouldn’t be seeing patients while I’m going through this. And I’m glad I took that time during the diagnostic process.

I was totally numb. I walked into my friend’s office and said, ‘I think I have cancer…’ I was completely in shock.

Diagnosis
Getting the official diagnosis
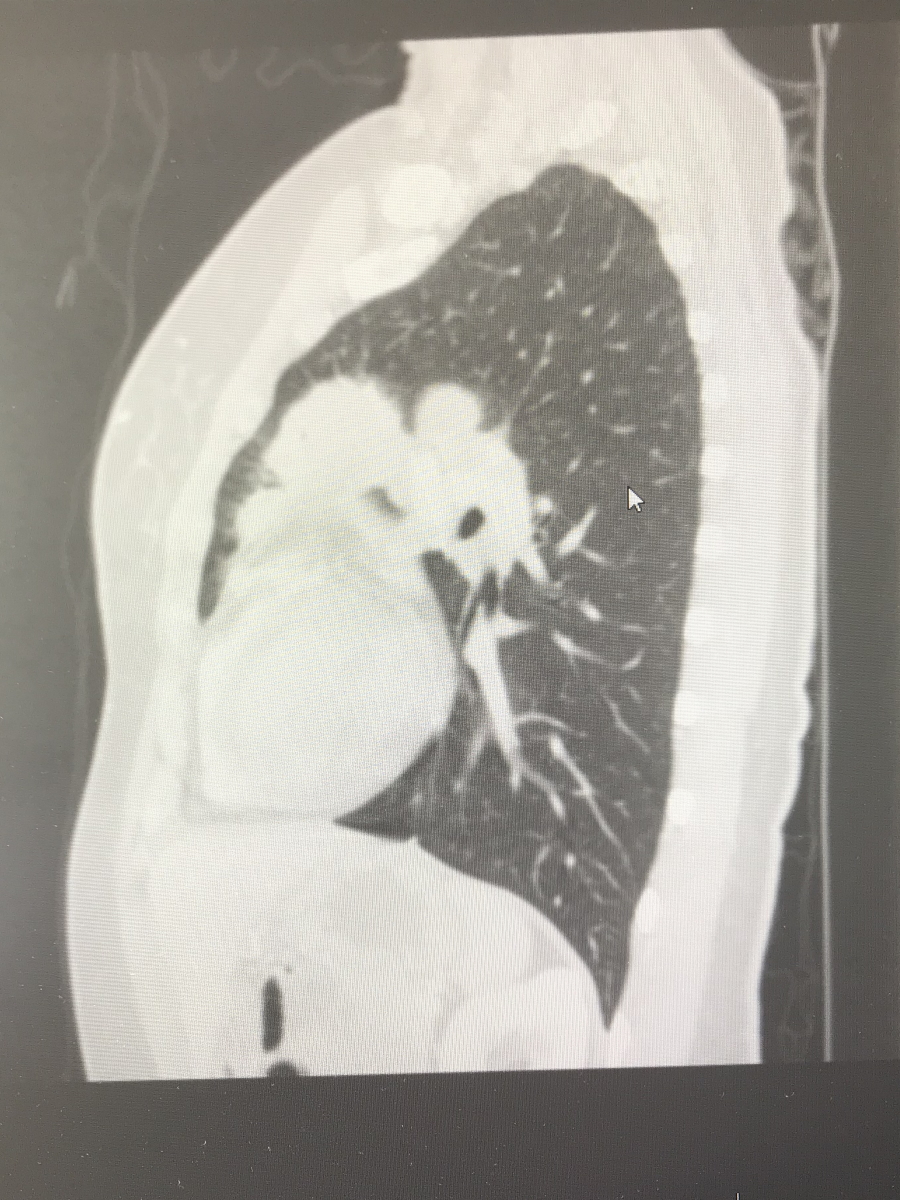
This is where my angst as a patient started, I think. After having that ultrasound and chest X-ray, I had some CT scans done that confirmed everything going on in my chest.
Next, you need tissue. [There are] generally two ways to get a biopsy in the head-neck area — interventional radiology [and] head and neck surgery. I was initially referred to head and neck surgery for a video visit to look at the scan and see if the surgeon [was] going to be able to biopsy or not. Was it reachable based on location?
I got on the video visit with my husband and the doctor said, “Hey, Sam, I saw your CT. I don’t think I’m going to be able to safely biopsy that because it’s too close to your carotid artery so I’m going to refer you to interventional radiology.” I thought, Okay, that makes sense. I wasn’t hysterical.
I had a three-year-old daughter that I had just finished nursing within the month or two before so I still had milk in both breasts and I guess it lit up on my CT scan. When I looked at my scans the weekend before the appointment, I wasn’t even concerned about what lit up in my breast. Then the next thing they said, without knowing a little bit more of my history, was, “I see something lighting up in your chest so I’m pretty sure you have metastatic breast or lung cancer.”
The doctor told me this and there was no pathology yet. I knew it was probably my breast milk. But that What if? part of my brain said, “A doctor’s telling me that I probably have metastatic breast or lung cancer.” I started hearing this high-pitched [sound] and the light drowning out everything. My husband sounds like he’s underwater and he’s right next to me. I started bawling.
I don’t even remember finishing the video visit. I think my husband finished it for me because I went nuts. My next vision was [of] my daughter at my bedside, giving me hospice care before I die. My mind flashed to a situation that could have potentially happened if I was a young person with those cancers. And that’s not even rational either because these days, people [with] late-stage cancers are doing really well and able to live much longer than before with all the new therapies. But I wasn’t thinking that. “Oh my god. He’s just giving me a death sentence.” That’s how I felt.
I was referred to interventional radiology and that doctor was amazing. My new PCP, my whole team, [and] all my colleagues were helping to expedite things. I was biopsied pretty quickly. They fit me in within a couple of days.


When I found out, my OB-GYN called to see how I was doing. She’s a colleague and a friend. While we were on the phone, she said, “Sam, your path just came back. Can I open your path report?” I said, “Okay, okay, you can do it. You can open it.” She opened it and said, “It’s Hodgkin lymphoma.”
I started bawling and was like, “Thank you, thank you, thank you.” At that point, there was so much whiplash and it was such a drastic swing from [when] it was a very different situation potentially. I was so grateful that this was Hodgkin’s lymphoma.
I just spent that weekend on a high. I was skipping around, “Okay, I’m going to live. It’s just going to be a touch of chemo.”
But it didn’t turn out that way.
Breaking the news to the children
My older two were eight and nine. We have gone through a lot of illness experiences with them. My husband is a liver transplant recipient and had a bout of testicular cancer in medical school and some health issues so we weren’t new to being on the patient side of things. In fact, I spent so many years as the wife in the waiting room eagerly awaiting any information. I know what that feels like and I always tried to remember that when doctoring people. Now it was me. It was such a shock.
When [my husband] was sick, initially, we would try to keep it from them because we thought we’re protecting them. Until there’s something that they can see visually, we don’t need to tell them. But kids are smart and they pick up that nervous energy, that tension.
Giving them some version of the truth that’s digestible developmentally at their age is really important.


When my husband was really sick one time — I thought we were keeping it all together — my four-year-old (who is 10 now and was nine when I first got diagnosed), his hair fell out. I took him to the doctor and she did all these tests. We were concerned about some illness and when we ruled everything out, she said, “I think his hair fell out because he’s really stressed. Is there anything going on?” I told her that my husband had just had a hemorrhage, we were waiting for a liver transplant, and he’d been in the intensive care unit.
She put us in touch with a child life specialist who guided us and said that kids see the visual, they feel the stress, and their minds fill in with the worst possible scenario. Sometimes, giving them some version of the truth that’s digestible developmentally at their age is really important.
We learned that earlier on and we knew that we were going to have to share this with the kids, at least the older ones. Things were about to get real with chemo and I was going to look really different pretty soon.



We decided to separate the older boys for the conversation. My older son said, “Wait, you? You’re sick? What are you talking about? Dad’s the one who we always worry about and you were just running 10 miles last week.” We told him and then we told our younger one.
The responses were really different. My older one was really mature and expressed his shock very openly. The younger one, the middle son, said something like, “Okay. Can I go play basketball?” He heard it, but he wasn’t ready to process anything. We didn’t tell our daughter until I had to buzz my hair and all that. She’s three at the time.
Treatment
There was some question about my staging because I had lung tissue involvement. Am I really 2AE or am I stage 4? The extra involvement of organs outside the lymph nodes can potentially be stage 4. When your lungs are involved, it’s somewhat controversial. If it’s continuous with the lymph nodes in that area, then you’re still 2.
What I understood at the time was that it would impact the length of chemotherapy because if you’re earlier stage, you might get two to six months depending on any number of things. But if you’re a stage 4, you’re almost certainly getting six months of ABVD.
They use the Ann Arbor classification and that’s the most classic one. Is there one group of lymph nodes above the diaphragm or two? Then once you’ve crossed the diaphragm to the other side, where your belly is, that tends to be stages 3 and 4.
[There are] other exceptions to those rules and different ways that you can come up with different stages and risk factors. Do you have anemia? Do you have elevated inflammatory markers? All kinds of other things can be taken into account that help put together a whole treatment plan, your true stage, and your prognosis with that stage if you have these other features on lab work.


ABVD chemotherapy
I think this is where I started becoming or at least feel like I was becoming labeled as the anxious patient because I had questions, [like] the lung involvement and what that meant. It started to feel like, “We’re going to discuss it and tell you what you are and what the recommendations are,” and really in a nice way. More like just let us take care of you and you focus on getting better.
For me, it didn’t feel that way. I want to be part of the conversation. I want to really understand what’s happening to my body [and] what the rationale is. Why not stage 4 or why stage 2? How did you decide that? I think physicians aren’t always used to getting those kinds of questions and I wasn’t asking anybody to defend the decision. I really wanted to understand. When I started asking those questions, I began to feel like, “Oh, geez, I’m a little too much right now.”
I was concerned from the get-go that I was really a stage 4, that it was more complicated, or that somehow four months of chemo wasn’t going to cover me. I just had that fear from the beginning. I don’t know why.
Would it be two months of radiation? Would it be four months? Would it be involved-field radiation? Some of the terms I had started reading about. I had to look them up, too, even though I’m a doctor. Would it be six months? When I started asking those kinds of questions and why this and not the other, that’s when I started to feel that things were taking on a certain vibe.
The answer that I got was, “Just start the chemo and then we’ll see what the two-month PET shows,” because that’s how it tends to go with Hodgkin’s. You get a PET scan after two months and see where you’re at. The response determines the rest of your outcome. Do you need more chemo? Do you need less chemo?
My second month PET scan was really good. The concern was just two more months of chemo, four total. I was concerned from the get-go that I was really a stage 4, that it was more complicated, or that somehow four months of chemo wasn’t going to cover me. I just had that fear from the beginning. I don’t know why.
I pushed for six months because I felt like I really want to slam this thing. I wanted just one and done if there’s any chance of relapse.
I don’t want to ever see this thing again. And for many people, that will be the case with Hodgkin’s.


By that point, even [after] four months, I started to feel really tired — that Mack Truck feeling is what I call it. I’d lay in bed for about three days after every ABVD. My mom called it the lagoon because I would just lay there with the lights off. The fact that I was advocating for more, I really didn’t want to do it but I thought if this [did] anything to positively impact my survival, then I wanted the more aggressive treatment.
I think they’re like, “Okay, she’s nuts. She wants two more months of chemo.” But I don’t want to ever see this thing again. And for many people, that will be the case with Hodgkin’s.
Side effects from ABVD chemotherapy & how to manage them

ABVD is a tough regimen. It was hard to figure out the toughness of things. Was it just the chemo? Was it the meds they were giving me to help with the side effects of chemo? That was hard to sort out at various times.
Nausea
Nausea was a big issue for me so I was on a lot of different anti-nausea medications — Zofran, Ativan, Phenergan. I was getting steroids. I also had Zyprexa one or two times, which is an antipsychotic medication. That was horrible. I was a zombie for days and couldn’t think at all — worse than the typical chemo brain. I really can’t put any sentences together. For some people, it’s an amazing drug and it works really, really well.
That’s one of those things. You’re trying different medications — some things are going to work for some people and other things are going to work for other people. It’s just important to know what’s out there so that you can ask for it.








