Heather’s Stage 2C Epithelial Ovarian Cancer & Stage 1A Uterine Cancer Story
Heather M., Epithelial Ovarian Cancer, Stage 2
Symptoms: Extreme bloating, pinching pain in right side of abdomen, extreme fatigue
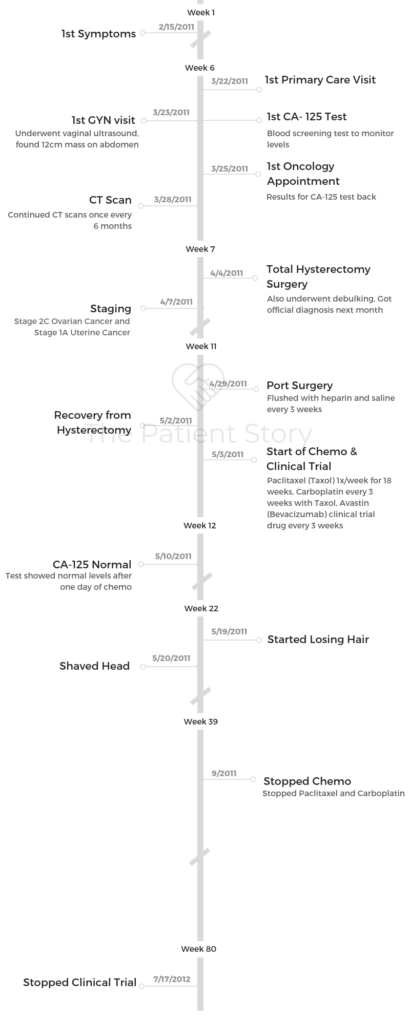
Treatments: Surgery (total hysterectomy), chemotherapy (Taxol once a week for 18 week, carboplatin every 3 weeks), concurrent clinical trial (Avastin) every 3 weeks
Heather’s Stage 2C Epithelial Ovarian Cancer & Stage 1A Uterine Cancer Story
Heather shares her story of stage 2C ovarian cancer, undergoing chemo, surgery, and a clinical trial with Avastin. She would eventually be diagnosed with stage 1A uterine cancer, which was removed by surgery.
As a former clinical trial program manager, she shares more on the process and what it entails. Heather also highlights important topics like how she paid for treatment, cancer’s impact on her sexual health, and how she parented with cancer. Thanks for sharing your story, Heather!
- Name: Heather M.
- Diagnosis:
- Epithelial ovarian cancer
- Stage 2
- Uterine cancer
- Stage 1A
- Epithelial ovarian cancer
- Age at Diagnosis: 40
- 1st Symptoms:
- Persistent bloating
- Pinching pain in right side of abdomen
- Pressure on bladder
- Pain during sexual intercourse
- How diagnosis happened:
- Went to doctor for separate issue (hand injury)
- Pelvic exam performed after telling doctor of symptoms
- Vaginal ultrasound shows 12-centimeter “complex” mass on right side of abdomen
- CT scan confirms mass
- Note: The official, full diagnosis with solid tumors cancer like ovarian require the surgical removal of the mass. Preliminary diagnoses are usually made before then.
- Treatment:
- Surgery (total hysterectomy and debulking)
- Chemotherapy
- Paclitaxel (Taxol) once a week for 18 weeks
- Carboplatin infused every 3 weeks (with the Taxol)
- Clinical trial
- Avastin (Bevacizumab) every 3 weeks
Those things that you beat into your brain as a mantra is extremely powerful medicine that you can do yourself. It’s setting you up to succeed, and that’s what we wanna do.
The doctors are fighting the fight with the medicines and all that, and you are fighting the good fight with your emotional medicines. Do try to do something like that, because I really felt that that helped me.
Heather M.

- Pre-Diagnosis
- What were your first symptoms?
- What was the catalyst that got you to go to the doctor?
- Describe the first doctor’s appointment
- What happened at the vaginal ultrasound?
- What procedures and tests came next?
- Describe the first visit to the oncologist
- You started having difficulty urinating
- What did they find at the ER?
- Tests & Scans
- Treatment Decisions
- How did you decide where to go for treatment?
- What did you like about going to a smaller treatment center?
- Did you get a second opinion?
- Did you research your cancer and treatment before starting?
- What’s your advice to patients and caregivers about to start treatment?
- Your doctor had great bedside manners
- Surgery
- How was the surgery prep?
- What do you remember about waking up from surgery?
- Describe the moment you heard that first official cancer diagnosis
- How was laparoscopic surgery described to you?
- How did you cope with the post-surgery pain?
- How long did it take to start recovering?
- Were there any post-surgery complications?
- The mental healing took longer than the physical recovery
- Do you recall the moment you got the staging?
- How did your loved ones react to your diagnosis?
- The debulking happened after. What is that?
- Chemotherapy & Clinical Trial (Concurrent)
- What was the decision-making to pursue chemotherapy?
- What was your first impression of the chemotherapy process?
- Describe getting the port(acath)
- Did you like the port?
- Describe your chemo regimen
- Describe what happened during and after the infusions
- You brought a “chemo buddy”
- You underwent your first clinical trial at the same time
- How long did it take to get the infusions?
- What helped you get through the infusions?
- Tip: tell your medical team about all side effects
- List of chemo side effects & what helped with them
- When did your hair start to fall?
- What helped most with styling your head?
- What helped with the hair loss?
- Were there side effects to the clinical trial (Avastin)?
- Getting into a Clinical Trial
- Work & Finances
- Support & Relationships
- Did you have to self-advocate through treatment?
- How did you talk to your kids about the cancer?
- You had to be more careful with germs
- Did you have to get outside help with the kids during this time?
- How did the cancer impact your relationship with your husband?
- Cancer's impact on the sexual relationship
- It’s important caregivers take care of themselves
- Ask people for support — they want to help
- Any last advice to people dealing with their own diagnosis?
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.

Pre-Diagnosis
What were your first symptoms?
- Bloating
- Pinching pain right side in abdomen
- Fatigue
I had just turned 40 years old. I have three kids; y kids were age 12, 10, and 4. I was very physically active. I was on a soccer team with my husband, a co-ed soccer team. I ran every day with my golden retriever. I felt like there wasn’t anything I was really, really concerned about.
I went for my annual checkups. As far as cancer in my family, my mother had had breast cancer and uterine cancer, but she was a survivor. I made sure to get my mammograms and things like that.
I noticed, though, that when I turned 40 in January, my pants started to feel snug. I knew that on certain days of the month, I would bloat like most women do, then I would de-bloat, and I could wear my skinny jeans then.
I remember thinking, “Oh my gosh, it’s snug down there.” I did more sit-ups. I tried to do more exercising. It still continued to be snug.
I also had a pinching pain on my right side in my abdomen, but I told myself it was just intestinal or something like that. It seemed to go away if I’d sit up, but if I sat down, I felt it.
As a busy mom of three, I just stood up more. I had this thing where I had the ‘three-strike rule.’
I was too busy to go to the doctor unless there were three things wrong with me. I hadn’t hit the three things yet.
What was the catalyst that got you to go to the doctor?
I noticed feeling always tired. What mom isn’t? What really spurred me to go to the doctor, though, was I was playing soccer, and this 200-pound guy kicked the ball as hard as he could at my face.
I got my hand up in time to block it, but we all thought my hand was broken. It was black and blue and this and that. I thought, “Oh my gosh, I really need to go to the doctor.”
Describe the first doctor’s appointment
I made an appointment the next day to go see my general practitioner, a woman who I had seen off and on for years. While she was looking at my arm, I said, “You know, I also think I’m gaining weight.”
At that point, I started to feel something may be pressing on my bladder. I had uterine tract infections before, bladder infections like that. I was going away to celebrate my 40th birthday with my girlfriends that coming weekend.
I asked if we could check to see if I had a bladder infection first because I didn’t want to get out to Asheville and then not have any fun.
She said, “Sure, we can do that.” While she was still looking at my wrist — my hand was fine by the way; it was just bruised — I said, “You know, I’m also gaining weight, I think. I’m bloated, and I’ve had this pinching pain on one side.”
She said, “Oh, well, that doesn’t sound right. Let me feel around.” She started to feel on the outside and said something didn’t feel exactly normal or right.
She wanted to do a pelvic exam, and I made fun. I said, “Oh, for a broken hand? That seems kind of a lot.” She said, “No, Heather, I really think that I should do that.”
I said, “Back in November, I had gone to the doctor for some spotting. They did a full pelvic exam in November. Said everything looked okay. Don’t know why I’m spotting. They said it was perimenopausal symptoms probably. I had never done that before in my life, and I just went home.”
I tried to talk her out of it. I said, “Well, I just had a pelvic exam several months ago, five months ago, and everything was fine.”
She said, “No, I really should do this.”
I let her do a pelvic exam. She said, “Heather, I can’t even get over to the right side of you. There is something blocking.”
Things started to happen very quickly then. She made an appointment for the next morning for me to have a vaginal ultrasound.
What happened at the vaginal ultrasound?
I had to drink a ton of water, which was not fun, so that they can see better on top of a full bladder. As I was trying not to go to the bathroom, the lady’s talking to me while she’s doing it. She was very sweet.
She was very chatty until she wasn’t anymore.
All of a sudden, she stopped and started to really take lots of recordings. Then she said, “Okay, I need you to sit here. Don’t go anywhere. I need to go talk to the radiologist.”
She disappeared, but she would come back in and call me sweetheart, offer me more blankets, offer me drinks, and all this stuff. It was starting to get to where I could tell there was something really not right.
My husband, luckily, had some sort of wisdom and foresight to have brought me. He was in the waiting room. Finally, they said I could get dressed, but not to leave.
We went and sat out there for another fifteen minutes until the radiologist came out and said, “There’s a mass, and it’s about 12 centimeters, which is about like this, on one side that looks like it’s your ovary, and it’s complex. You need to go right to your gynecologist and share these films with him.”
They had been trying to call the gynecologist for 15 minutes and could not get through. That’s what the holdup was.
What procedures and tests came next?
My husband basically took me and the films, loaded me in the truck, and drove me straight there. I don’t really remember much of that because you’re sort of like been slapped in the face.
He’s driving me there, and I know it’s a very busy practice. There’s tons of pregnant women everywhere. I just go up with my films to the receptionist, lay them down, and say, “Help. I have a complex, large mass, and I need to be seen right away.”
They got me back with somebody within five minutes. He’s looking at it. He did another exam. They took a blood test. He said, “Okay, it looks complex. I could remove this. This is a mass that should come out, but it’s complex.” I think that it had blood vessels in there.
He said, “I’m gonna send you to a gynecological oncology surgeon.” I found out later your number-one way of surviving ovarian cancer, which is what I had, is to have the right surgeon treat it like it’s cancer before they know that it’s cancer.
They took a blood test called CA 125, which I have had tons of since. It’s a marker test. There is no screening test for ovarian cancer. In the early stages, CA 125 can show a normal response even though you have cancer. They don’t like to use it, but it’s just another piece of evidence.
Luckily, they were able to get me into a really good gynecological oncology surgeon the next day, which was wonderful, except that I was supposed to be leaving with my girlfriends to go to the mountains.
I had to call them, and that was very, very emotional. It was very scary. You just don’t even know what to think, but I didn’t know anything at that point for sure.

Describe the first visit to the oncologist
The next morning, I went to the oncologist. She looked at it and she said, “Okay, it could be a benign mass, or it could be cancer. We will not know until we take it out, until we open you up.”
We scheduled the surgery for a week later. The CA 125 came back as slightly abnormal. The normal is below 35, and I was 42. I’ve known people who have had numbers up in the tens of thousands, so 42 was not something that would say yes, it’s cancer, so again, I was in limbo.
The whole weekend I was in limbo, but my girlfriends were all around me. The only advice I was given was, “Don’t rupture it. Whatever you do.”
Everyone made sure I didn’t run, I didn’t fall, [and] there was nothing that would cause it to rupture.
You started having difficulty urinating
I got back on Sunday, and on Monday, I ended up in the ER because I could not urinate. I drank a full chai latte. I’m a writer, so I went to write. I went to go to the bathroom, and nothing would come out.
About an hour into this, I’m in excruciating pain and being taken by my husband to the emergency room, where they drained almost two liters of urine out of me.
What did they find at the ER?
Come to find out that mass was pushing so hard on my bladder that it seized, and so it could not relax enough to allow me to pee. That was my first actual CT scan because they did that in the ER, and of course they came in and said, yes, it is a mass.
We said, “Well, can we cut it out now because we’re at the same hospital?” But they couldn’t fit me in, so I still had to wait until the next week.
We went to the hospital in the afternoon to have it out, and that was awful because I couldn’t eat or drink, so I was dehydrated and nauseous from hunger.
Tests & Scans
Describe the pelvic exam
With the pelvic exam they also do a rectal exam, and then they do palpitations around your abdomen. It’s like an annual pelvic exam where a woman is up in the stirrups, you have your heels in there, and they do need to enter the vagina.
They’re not doing a pap smear because pap smears don’t detect ovarian cancer (that’s cervical cancer), but what they did was push on one side and push on the other side.
Because I had a mass and they weren’t gonna rupture it, they pushed very gently to feel the edges, to feel it. It was really like a regular pelvic exam done at an annual gynecological physical.
They also then have to put a finger in your rectum because they can also feel it that way. They are very good about preparing you, telling you, making sure it’s not painful.
Usually what they do is they tell you to bear down like you’re having a bowel movement, and then they can go in there, you relax, and they can feel from that wall as well. Then just palpating on the abdomen is just like what regular doctors do, but they are gonna be real gentle if you have any type of a mass.
Describe the vaginal ultrasound
It sounds scary. It’s nothing worse than your pelvic exam except that you might have a full bladder because they tell you to drink a bunch of water usually so that they can contrast between whatever they’re looking for against the bladder.
The bladder is like a lit-up pillow or something, and they’re looking at things on top of it. That was the only uncomfortable part, and I told her.
I said, “I’m gonna pee on the table.” She goes, “You wouldn’t be the first.” She’s like, “It’s okay. Just try to hold on,” and then I put my feet in the stirrups again.
You’re in a shirt, you remove your bottom parts, and then you have a blanket or a sheet over you. You’re not just out there in the room. You’re covered, and they know what they’re doing. There’s a little flat paddle, and then they put lubrication stuff on it before putting it inside the vagina.
They’re going to take ultrasound pictures that way. It’s like getting the ultrasound on the belly, but with the transvaginal ultrasound they get a much better picture of your ovaries, uterus, and those parts of your body for a woman.
Describe the CT scan
I had the added difficulty of being allergic to CT dye. CT dye is put into your vein through an IV, and it helps light up whatever they’re looking at in the blood.
The first couple CT scans that I took, I had to drink a nasty-tasting something (as prep), and they would take some pictures.
It tasted terrible and I’m really bad about tastes, so I learned to ask to put it into my own drink.
I would bring a lemonade or something that I could drink because I didn’t like what they had, and they let me do that after a while.
Somewhere in there they stopped having me drink the stuff, but for that CT scan, I did have to drink this nasty stuff. In the scheme of things, it was okay. It didn’t make me sick; it just was really super sweet. I drank that down, then they took me back, and then they gave me an IV.
Because I was allergic to CT dye, which I knew from years ago, I had to take a bunch of prednisone (steroid) beforehand. When they had me at the ER and they did the CT scan, they did not do the contrast dye.
The contrast dye gives a better picture, but because I was allergic to it and they didn’t have time to prep me for it at the ER, they didn’t do it there.
Then they put you in this big, open donut. It’s not like an MRI where you’re enclosed; it’s just an open donut, and then they just lay you down and slide you in.
This machine tells you, ‘Breathe in. Hold your breath. Breathe out.’ Like that. That’s all you do. So you go in. You hold your breath.
If you don’t have any dye in you, you don’t even have to have an IV really. You can’t have anything wire on, so one tip if you’re getting a lot of CT scans done, wear a bra that does not have an underwire, and they’ll let you keep it on.
I learned to wear clothes that had no rivets in it, no snaps, nothing, and then I didn’t have to get into their little gowns or anything. So keep that in mind.
No jewelry, no underwire bras, and then you don’t have to undress. I keep my socks on because my feet always got cold. Then they just slide you in, you hold your breath, they take one or two pictures, and then that’s it.
How long did it take to get results for your tests and scans?
The CA 125 has to be sent off. The first one that I got, actually, they called me on my way driving to the mountains with my girlfriends. My girlfriends would not let them tell me what it was on the phone.
They made me ask them to call my husband and tell him. The nurse thought that was really odd, but they did not want me upset. They were really happy and this and that.
They took it on a Thursday, I saw the oncologist on a Friday, and then it was Friday afternoon when they were calling me, so it was only a day. It was 24 hours.
That time on, my nurse and I became really close. An oncologist nurse. She would track me down anywhere. She would tell me what my CA 125 is. It would go maybe a half a day to 24 hours at the most.
Once I started having them regularly, they wanted it done at the same lab all the time because it could fluctuate if I was changing labs a lot. I would always get the CA 125 drawn at the same laboratory after that.

How did you break the news to your loved ones?
From the ultrasound, we went directly to the GYN. Coming home from that, I remember pulling up in the driveway. My mother was watching my four-year-old. My neighbor was outside, and she came around. I was getting out of the truck, and she said, “What’s wrong?”
I just started bawling and just buried my head in her chest. I’m like, ‘There’s a mass. They think it could be cancer, and I have to see an oncologist tomorrow.’
I was just a mess. I don’t even remember how I got inside. Somehow I got inside, and my mother was there. She’s trying to take care of my four-year-old daughter, my other kids are there, and I can’t hide emotion.
That’s not something I ever will do with my kids necessarily. I mean, there’s some points where I did, but I never wanted to hide, and I couldn’t. I couldn’t hide being scared and worried and all that. It was my mom.
I gave her a quick rundown as quickly as I could. Then I remember my husband, he and I just went out and sat on the back deck by ourselves and just looked at the trees and the birds, and it was just really hard because we didn’t have anything to say.
We just held hands and said, “Wow, things can change like that.” One second you’re playing soccer, and the next second you’re in a doctor’s office and they’re telling you that it could be cancer.
I think they handled it really well. The doctors said, “Let’s talk about the elephant in the room. I don’t know if it’s cancer, but it could be.” It is a slap in the face, and it’s hard to breathe. It’s hard to just process it.
Then having to call my girlfriends, because some of them are flying in, to tell them, “Okay, I can’t pick you up from the airport because I’ll be with an oncologist,” and them trying to love on me over the phone as much as they can.
Of course people want to tell you that it’s fine. ‘It’s gonna be fine. It’s gonna be okay.’
That’s all great, and that’s what people do when they don’t know what to do, even though I knew that it could be not okay. You just stare, and you just breathe.
My husband was a trooper, and he fought as hard as I did. It could have gone the other way because his mother died of breast cancer when he was nine years old. He was now suddenly faced with a wife, with three kids, and he didn’t know what he was gonna have to deal with, which leads me into what he had to deal with when I was in surgery.
It just knocks the breath out of you. It really does because you don’t know, and it’s horrible for anybody, but when you’ve got a four-year-old who’s climbing on you, you get more scared about what’s gonna happen to them, your kids.
»MORE: Breaking the news of a diagnosis to loved ones
Treatment Decisions
How did you decide where to go for treatment?
It worked out to where my GYN said, “I want to send you to a gynecological oncology surgeon.” I live in North Carolina in the Triangle area, so University of North Carolina Medical School and Hospital is a really good one, and Duke University Hospital is another really good place.
It just so happened we thought my insurance might work better with Duke, and they had an oncologist available the next morning, Dr. Paula Lee, who was fabulous. I can’t say enough good things about her and her team.
I went there, and when I spoke with her the next day, she had me come to a small location. There’s a big Duke Medical Center with their Cancer Center, which is beautiful. There’s meditation rooms, all sorts of stuff.
I went to a small offshoot of that. She felt that I might like it better there. I think I did because it was smaller, more intimate. I didn’t have to pay for parking. She worked there half the time. She did her surgeries at big Duke, but she could do it at the smaller location.
What did you like about going to a smaller treatment center?
I’d seen people go to big Duke. I had gone to talk with people in chemo there, and that’s great. A big hospital is great. There are lots of things, but it’s also a really long distance to walk. They have wheelchairs and stuff, but it’s just huge, so I personally felt like I got very good service at a smaller branch.
I think I would probably recommend that over going to a huge hospital unless that’s really your only choice. There are perks for that, like the meditation room and things like. Music therapy. They had someone playing the grand piano in the foyer and things like that, but I personally liked the smaller campus.

Did you get a second opinion?
Because it was all happening so fast and because I agreed with her that whatever it was it needed to come out, I did not feel like I needed a second opinion.
I went under not knowing that I was going to have a total hysterectomy and my ovaries gone and everything. Dr. Lee spent a lot of time right before I went into surgery explaining [scenarios] to me.
“If this happens, this is what I’ll have to do, and if this happens, this is what I’ll have to do. I need you to sign off that you are okay with me doing all these different things if this happens.”
I went under fully understanding, but I didn’t know what was actually going to happen.
Did you research your cancer and treatment before starting?
The first part, I was just too engrossed in getting the surgery to go online. Actually, my husband wouldn’t let me go online. I think he went online, which was probably not good either.
But I know after I was diagnosed he spent a lot of time online, and the more he was on there the darker circles that were under his eyes, because you get doom and gloom on the internet. You get a lot of doom and gloom, and you don’t get a lot of the uplifting, hopeful stories.
Anybody who goes online to do their own medical research and stuff with diagnosis and stuff, just take that knowing that it tends to not show you an even good and bad.
It tends to show you bad, bad, bad, and so I was told that I shouldn’t do all of that, especially because we didn’t know what we were dealing with.
The nurse told me months later that Dr. Lee actually went in thinking that I did not have cancer and that she was very angry on my behalf when she realized that it was indeed cancer.
Again, she was a very experienced oncologist surgeon, and just looking at the CT scan and ultrasounds, she could not tell for sure that it was cancer until she went in.
What’s your advice to patients and caregivers about to start treatment?
Make sure whoever is going to be sitting in that waiting room while you’re in surgery has support, because you don’t know what’s going to happen.
My husband was all by himself and my surgery was only supposed to be an hour and a half. They said, “If it’s cancer, we’ll come out at an hour and a half and let you know things are going well, but it’ll be a little longer.”
At two hours, they came out and said, “Things are going well, but it’s going to be a little longer.” It was five hours. He lost his mom to cancer when he was nine, and he was by himself, so think about it.
Not to assume the worst, but if you have someone waiting in the waiting room, have them have some support or a friend if it is going to be bad.
Your doctor had great bedside manners
I love doctors and nurses, oncologists especially. I don’t know if you notice this as a patient, but they tend to walk into rooms and shut the door quietly. She would move quietly, she would move gently, and she would talk to me gently. Nothing was rushed or fast.
Now when I go visit her, she’s like, “Oh, how are you?” It was always calm and gentle. I even told her later, “Do they train you to do that? Because that was really good.”
Because you are in a state of shock. You are still in a state of shock. You just need this buffer around you, people to be kind, and people to smile, be helpful, not scare you, and not tell you their horror stories. But also not give you false hopes. Not too many false hopes, either.
Surgery
How was the surgery prep?
It’s hard. I know that they asked me how I was feeling, and I just said, “I’m nauseous because I’m so hungry and dehydrated.” Because they wouldn’t let me drink anything.
They said, “Well, we have to set up the IV, and we’ll give you fluids so you’ll feel better.” That was sort of a little carrot dangle. “You’ll feel better if you let us put the IV in.” [I’m scared of needles.] I gave birth to three babies, and the worst part was getting the IV.
My husband was back there with me and held my hand through getting the IV. I breathed and tried to think of happy thoughts. I learned later how to think of happy thoughts and come up with a happy thought.
It’s very, very important to have a happy place that you can retreat to in your mind. I did not, at that time, have one. But over the subsequent 15 months of chemo, I did come up with one.
That was the second of 108 sticks I had in one year. By the end, I no longer fear needles. I have a healthy respect for needles, but I don’t fear them anymore.