Jodi’s Stage 4 Epithelial Metastatic Ovarian Cancer Story
Jodi S., Epithelial Ovarian Cancer, Stage 4
Symptoms: Extreme bloating, extremely tight skin, changes in digestive tract, significant pelvic pain, sharp-shooting pains down inner thighs, extreme fatigue
Treatments: Chemotherapy (pre- & post-surgery), surgery (hysterectomy)

Jodi’s Stage 4 Epithelial Metastatic Ovarian Cancer Story
Jodi shares her stage 4 ovarian cancer story, from first symptoms to undergoing chemo and a hysterectomy, and also highlights how she navigated life with cancer.
In particular, Jodi describes losing her hair, including eyebrows and eyelashes, how important it was to have caregivers and support, and how she managed a cancer diagnosis and treatment as a parent. Thank you for sharing your story, Jodi!

- Name: Jodi S.
- Diagnosis:
- Ovarian cancer
- Epithelial
- Stage 4 (metastatic)
- Age at Diagnosis: 42
- 1st Symptoms:
- Extreme bloating
- Extremely tight skin
- Changes in digestive tract
- Significant pelvic pain
- Sharp, shooting pains down inner thighs
- Extreme fatigue
- How diagnosis happened:
- Felt body wasn’t right after birth of sixth child, insisted on testing
- Treatment:
- Chemotherapy, 4 cycles
- Hysterectomy
- Additional chemotherapy, 3 cycles
- Diagnosis
- Treatment Decisions
- How did you decide where to get treatment?
- Did you get a second opinion?
- How did you like your medical team?
- You've been to both a small and big hospital. Which was better?
- Did you understand the different players on the medical team?
- Describe each test and biopsy
- What were the results of the biopsy?
- How long did it take to get results?
- Describe the wait between appointments, tests, and results
- Did you undergo genetic testing?
- Treatment and Side Effects
- What chemotherapy treatment regimen did you undergo?
- Describe each cycle of chemotherapy
- How many bags of chemotherapy for each cycle?
- How were you feeling physically after each infusion?
- Did you experience any chemotherapy side effects?
- What medications and methods did you find most effective with the side effects?
- Did the cycles of chemotherapy get better or worse?
- Did you get a port or a PICC line?
- Describe the plan for surgery (hysterectomy)
- Describe the actual surgery
- How long did the surgery last?
- Any side effects after surgery?
- How was your second round of chemotherapy after surgery?
- Did you have the same side effects?
- What was the toughest part about treatment?
- How was your PET-CT scan after you finished treatment?
- How often do you have to undergo scans moving forward?
- Life Outside Treatment
- Describe the hair loss
- You also lost your eyebrows and eyelashes
- Were you surprised by your reaction to losing your hair?
- What helped you feel better about the hair loss emotionally?
- What helped you with the hair loss physically?
- You had to experience hair loss again after the second round of chemotherapy
- What helped you manage your thoughts and emotions?
- How did you manage your energy levels?
- Were there any big surprises during treatment?
- "Let yourself feel”
- You and your spouse had to work out a system in who would do the research
- How was the financial part of the process?
- Did you use alternative or holistic medicine?
- Support and Parenting
- What's your advice to people undergoing treatment for ovarian cancer?
- How important is it to have caregivers?
- Advice to cancer patients on how to ask for help?
- How many children do you have, and how old were they when you were diagnosed?
- How did you manage your emotions around the children?
- What are the extra considerations for a parent undergoing treatment?
- Any advice to other parents who are dealing with cancer?
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
You can do this. It will be hard, and there will be good days and bad days. I think it’ll be harder than the doctors portray it to be, but you can do it. Your body can do it.
Let people help you, let people love you, and really take care of yourself and stay on in a good, positive mental mindset. You can go to the dark places, but bring yourself back to the positive places.
I think you will be surprised at what your body can do. I have been.
Jodi S.
Diagnosis
How did you get diagnosed?
After I had my last baby, my belly just never went down. It just felt like it never got back to normal, even in exercising, I could lose some weight, but as soon as I got it off, I would just balloon back up. That was a concern, so I was talking to my doctors about that.
It felt, as time went on, it was getting tighter and a little more uncomfortable. Then probably about three months before I was diagnosed, it really started getting big and uncomfortable and tight.
I’ve been pregnant six times, but I never felt like my skin was going to open like that. When you’re pregnant, you just feel like you’re going to pop. I really hadn’t experienced that kind of feeling of explosion.
When that started occurring, I started having a lot of pain down in the pelvic region. When I would eat, I would have some sharp, shooting pains down my inner thighs. I had a very raspy voice. I wasn’t sick, but I sounded like I was sick. I sounded terrible.
You had to fight for the first doctor to listen to you
I think that was just me demanding, “This isn’t right. I don’t feel like this is a weight loss problem.” I think all the doctors wanted to help me lose weight, to get the tummy down. Just saying that I could feel something in my lower abdomen.
It’s going and saying I want all these tests. Test me. I think with ovarian cancer, a lot of patients are misdiagnosed with weight problems or digestive problems or things like that.
I just knew that I was really starting to lose my energy and having a hard time walking, so I knew something wasn’t normal. I just went in and cried until they did it.
»MORE: How to be a self-advocate as a patient
Describe your first symptoms
- Extreme bloating
- Abdominal pain
- Fatigue
- Changes in the digestive tract
- Difficult to walk
- Extreme loss of energy
I would really only notice [the abdominal pain] when I was laying down, usually after I ate a meal. I would think, “Oh, my ovaries hurt, or something’s going on.”
At first I thought I was starting to have menopausal symptoms, but when I would look that up online, my symptoms didn’t align with the menopausal symptoms at all. I just kept looking, and ovarian cancer was coming up a lot with my symptoms.
I started feeling like, “I think I have this. I think I should be tested, or at least my insides should be looked at.”
How did you convince the doctor to order the first CT scan?
Instead of saying, “I’ve got this big bloated belly,” I finally went into the doctor and said, “I don’t think this is weight related. There’s something wrong. I feel like there’s something in my lower abdomen. I want a pelvic exam; I want scans. I want anything. This big belly’s not normal, and it’s not due to weight loss.”
I had seen the nurse practitioner to my family practice doctor. I had never seen her before. She really was listening to what I was saying. She gave me the pelvic exam. During that exam, I could feel the tumors, and I told her, “I can feel those.”
She said, “They may be uterine fibroids.” I said, “I don’t think I feel good enough for this to be uterine fibroids.” She originally scheduled me to get an ultrasound and later that day just decided, based on that exam, to skip the ultrasound and head straight to the CT.
I think she knew I wasn’t going to leave without some sort of exam or some sort of test set up, but she was very sympathetic, really listened to what I was saying, and didn’t brush it off as a weight problem.
I felt so relieved she listened to me. It was just more relief and a little bit of fear that someone was finally agreeing with me. Her words were, ‘All of my little alarms are going off for you.’
I did have that little sense of fear, but I think I already knew that it was cancer, so I braced myself for it.
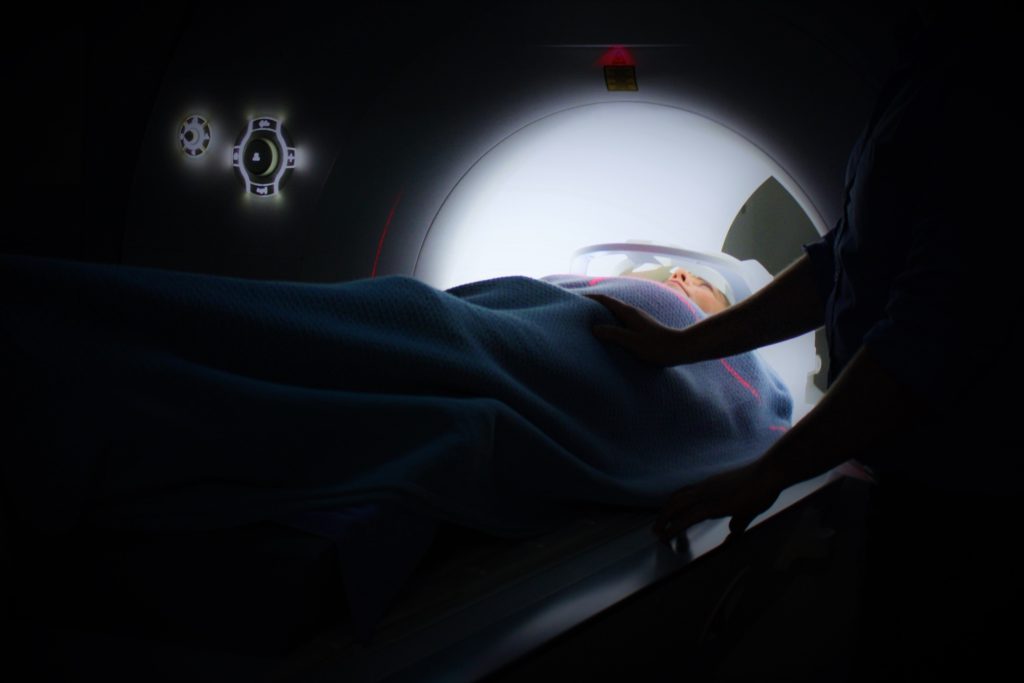
What was the CT scan like?
I just went in, drank some water. They put in an IV, put in the iodine, which is a really weird sensation. They tell you everything that’s going to happen. You’re not in the machine very long; you just kind of go in, breathe, and come out.
I didn’t have any side effects from the iodine. I felt pretty good, but a couple days after, I just felt yucky. I wouldn’t even say I was sick. I just didn’t feel right. I wasn’t hungry.
The bloating in my tummy was off the charts, but after a couple days, everything settled down. Every time I get a CT scan, for a couple days after I just feel a little off, but not really sick. Just not well.
How did you process the news of your diagnosis?
I was driving in my car by myself, and I saw my doctor’s office pop up, so I pulled over. I actually said to myself, “He’s calling to tell me I have cancer.”
I got myself to a good place where I could talk, and he was kind of beating around the bush, like, “This looked good on your CT,” and I said, “Just tell me the bad stuff.”
He said, ‘You’ve got some big tumors on your ovaries, and it’s looking like ovarian cancer.’
I was like, ‘I knew it!’
He said, ‘What?’
I said, ‘I just knew it!’
I felt almost a little excited. I was actually glad I was by myself when I hung up the phone. I was by myself, and I just had some time to collect my thoughts. Within the minute, I knew how I was going to approach it.
I had confidence in myself. I had this little plan for myself that I was going to listen to my doctors, I was not going to react, I was not going to Google anything, and I was going to listen to my gut.
»MORE: Processing a cancer diagnosis
How did you break the news to family?
I believed I was strong enough and could do this. That made it easier to go back and tell my husband and six kids later. I told my husband, and he was bawling. I was very composed and ready to move forward. He was bawling. Then I told my kids, and they were bawling, but I was okay.
It was when everybody went to bed — and I had never seen my kids that scared — that night when everyone went to bed, I got my turn to cry.
But I wasn’t crying because I had cancer, and I wasn’t crying for myself. I was crying because it was so heartbreaking to see my family like that.
»MORE: Breaking the news of a diagnosis to loved ones
Treatment Decisions
How did you decide where to get treatment?
I just got the scan at the local hospital near my home, just a small hospital. When the results came back and I went for a follow-up with that nurse practitioner, she had already scheduled me an appointment with the gynecological oncology department down at UCSF.
She was very excited to have gotten me in with that group and just real excited that she was able to get an appointment at all. I didn’t have to go and search. She set all that up for me. It felt like she was giving me the best.
Did you get a second opinion?
I didn’t because I loved my doctor at UCSF, and I just felt great about her from the first second. My husband really wanted a second opinion, so we went down to Stanford and had a great doctor down there.
She pretty much said they would do exactly what the doctors at UCSF were doing. It’s about an extra hour drive to Stanford from my house, so she didn’t think it was practical to come to Stanford. She knew my doctor at UCSF and said if I had that doctor, I would keep that doctor.
But I will say the thing about the second opinion is after meeting with the first oncologist the first time, we had some questions. Leaving and going home and really thinking about it, we had some other questions.
This doctor knew we were there for a second opinion. She was like, “Ask questions. Ask me questions, all the questions you can, and when you go back to your other doctor, you can compare and see.”
She was really good to answer a bunch of our questions directly knowing she wasn’t going to be caring for me. I think that helped my husband a lot.
I didn’t want to know a lot of the details, so I was out of the room for a while.
How did you like your medical team?
What we ended up doing with my treatment was I had a regular oncologist at UCSF. They’re part of an oncology group, so the group reviews everybody’s cases.
Doesn’t matter who your doctor is. They meet together. They go over your case file and all make decisions together on how they’re going to proceed. So I felt really good.
Even though I loved my doctor and I would have trusted anything she said, I felt really good knowing she wasn’t just going to be making decisions off the fly, that everybody sat down.
Maybe people with more experience, less experience — they were going to talk about my case, and they were going to come to a decision together. I always felt very confident that I knew my case was getting looked at very strongly.
For my chemotherapy, UCSF is quite a drive from my house, so they referred me to the Marin Cancer Center. I had a separate oncologist there who just took care of my chemo. My UCSF doctor was the one in charge, and she would tell him what she wanted done.
They would coordinate together. I liked that there were two doctors because they would tell me different things, and then they’d come to an agreement together.
I will say my chemo doctor was a little more willing to talk to me more straightforwardly, like, “If this doesn’t happen, then this,” or, “This is really not good.”
I would get a little bit worked up, but then when I talked to my regular oncologist, she would calm me right down. She just knew. She would say, ‘This is something that we don’t need to worry about right now. If it happens, we’ll address it.’
Back to that, just don’t tell me more than I need to know because there can be a lot of anxiety involved in worrying about the what if’s.
You’ve been to both a small and big hospital. Which was better?
I actually found that I liked UCSF much better, mostly because I was really in an oncology department. They were very sensitive to that. I think they’ve got several different locations where they’re doing the radiology stuff, so the radiology technicians do a lot of it. They’re very friendly, skilled, with good bedside manner.
When I went to the small hospital, they had actually told me the wrong appointment time. When I came in, they said, “You missed your CT scan.” I said, “I’ve got my little card right here.” They had scheduled it wrong.
The nurse practitioner was like, “Whoa, look at that size of that belly! We’ve got to get you in today. Let me call and get you worked in!” I remember feeling a little nervous when she said that.
I was so grateful that she was squeezing me in and she was being sweet, but those kind of things set off little alarms in you.
I remember feeling nervous, and I never felt like that at UCSF. I just think at the department down at UCSF, they’ve been trained to be more non-reactive to the different things.
I felt they were all very professional. Since it was a teaching hospital, they were very informative, telling me what they’re doing and why. It was just great; I loved it down there.
As for my infusion center at a different, “smaller” place (Marin Cancer Center), I actually liked having the little smaller place for my actual infusions.
That was a much smaller community, and I think for my chemo, I loved that. Because it was a small infusion center, I knew all the nurses taking care of me, they knew me, [and] we knew about each other. It felt like family.
You would get to know the people around you in the room. I’m there on Fridays; I know all the Friday people. That had a real family and community feel to it. That was closer to home.
Did you understand the different players on the medical team?
Yes, I used the online portal a lot to communicate with the nurses or with the doctor. My doctor was very good and would communicate directly with me. She’s called me several times. She would always call me before she put something in the portal and talked to me about it.
I felt like I had great communication with her. I felt every time I went in for an appointment at UCSF or at Marin General, I always had to fill out mental health questionnaire, so I knew that there were resources available.
If I had said, “I’m struggling; I’m spiraling,” I knew that the doctors would be in there in a snap to get me set up with something. I always felt like there were resources available to me.
I didn’t really need any of them, but I felt like I would have easy access to them if I needed it. I would have felt very comfortable to call and say, “I’ve got to talk to somebody right now.”

Describe each test and biopsy
After the first CT scan, it was just of the abdomen, but they could see a little bit of fluid in my lungs. I went and had another CT scan done of the chest, where they did find a little growth on my sternum and a couple of enlarged nodes in my lungs.
After that, I had to have a biopsy in my lower abdomen. I think they were trying to get tissue right off the tumors on the ovaries.
It was a very simple procedure. They just numb you up. They go in with a needle and take a sample of the tissue and sent it off for testing to find out what exactly kind of cancer I had and to make sure it wasn’t colon cancer or another type of cancer showing up in the ovaries.
It was very similar to getting an ultrasound for a baby, actually, because when you go in, they put all the goop on your tummy and do an ultrasound to actually find good pockets of tissue.
When they go in, they know exactly where they’re going. I did not feel a thing. I can’t even remember feeling anything when they numbed the area, when they did the numbing injection.
It was very painless at that time. Since I was so bloated, they did drain a bunch of fluid at the time, and it made me feel so much better. There was really no recovery. I went and sat in a waiting, recovery room for about an hour and then got dressed, went home, and was fine. The whole thing was pretty easy.
I’d get my blood test the day before I had chemo. I’d go in and get my blood drawn just to make sure all the levels were okay and that I had recovered well enough and also to track the CA125.
It’s one of those tumor markers, which is a really good indicator for ovarian cancer. It was one of the things they did to diagnose me with ovarian cancer. A normal CA125 is between zero and 35.
Mine was at around 6,500, so it was a big indicator. Then every time I’ve had chemo, it’s been going down and down and down. It was high. I think you can use it to mark other cancers, but it’s a very good marker for ovarian cancer.
What were the results of the biopsy?
Originally, I was diagnosed with stage 3, but once they found the stuff up in the chest area, they bumped me up to stage 4.
It had crossed over into the lungs, but it really hadn’t metastasized. They still wouldn’t classify it as metastasizing out of the lower abdomen so much.
It wasn’t in any of my vital organs.
The lymph nodes in the lungs were very tiny, just barely enlarged, so it was the growth on the sternum that was the big concern for them.
How long did it take to get results?
For the biopsy, about a week. But I’m going to go back to when I was first diagnosed.
First, it took a long time to get the first CT scan and then a long time to get back into the doctor. When I got my first appointment with my oncologist, it was about three weeks out.
You know you have cancer, and you have to wait three weeks to see the oncologist. Then they’re scheduling another CT scan in two weeks, then a biopsy, and you have to wait.
The doctors didn’t have the sense of urgency that I did. Looking back, now that I’m on the other side of it, they were actually — in terms of medical scheduling — getting me in quite quickly. Things were moving the normal rate and the normal pace, but when I was actually in it, I felt like it was forever. I was very impatient.
Describe the wait between appointments, tests, and results
It felt like, ‘I have cancer! Let’s get going on this!’ But there was quite a bit of a wait, and that’s so normal. The doctors weren’t worried about it, but I was.
I’ve come to find out from everyone else I’ve talked to that just the waiting to get the treatment started is the worst part. I think that was just horrible waiting.
Waiting to get going because I knew there was stuff all over in me, and I just wanted to start working on getting it out of there.
»MORE: Dealing with scanxiety and waiting for results
Did you undergo genetic testing?
We did genetic testing. Ovarian cancer is highly linked to breast cancer, so I met with a genetic counselor. We talked about my family history, family tree going back, family kids who are younger, females that are younger.
There were several different types of genes they tested for. BRCA1 and BRCA2 and some other more unusual genes. They were thinking I’m quite young to have ovarian cancer, and I’ve had six babies.
Usually that will serve as a protection against ovarian cancer, so they were hoping there was something in my genetics, but everything came back normal.
I just talked to a counselor. We went back and filled out a family history tree, talked about health issues within the family, especially cancers and different types of cancers. Then I just had to fill a test tube up with spit, and I was on my way.
Those results took over a month to come back. They weren’t so urgent at the time because I had already started some treatments.
We haven’t talked about my big hysterectomy surgery yet, but after I had that, they did do genetic testing just on the ovarian tumors just to see if it was a rare kind of tumor.
Maybe I didn’t have it in my genetics, but maybe the tumors had something wrong with it or weird with it. It all just tested as a normal ovarian tumor.
Treatment and Side Effects
What chemotherapy treatment regimen did you undergo?
I had four rounds of chemotherapy, followed by a complete hysterectomy, and then three more rounds of chemotherapy.
Describe each cycle of chemotherapy
I had chemotherapy every three weeks. The infusions took about six hours.
The first cycle — I believe it was the Taxol — I had a bit of an allergic reaction to it, and they told me I might. It was really scary. They told me what would happen, but when it actually happened, it was really scary.
They started the infusion, and I was doing fine. They left, and all of a sudden I went from “I’m fine” to “I can’t breathe.” A cute lady in the room looked at me and said, “Do you need help?” I just nodded. She ran and got the nurses.
They were able to take care of that with some antihistamines quickly. They would do my Taxol infusions a little slower, so it would usually take well over six hours to get my infusions. There was a real chemical taste in my mouth and throat. I could tell I was being poisoned with something.
With the Benadryl, I usually just slept. I didn’t like people coming with me to get my infusions because I didn’t want to feel like I needed to entertain anyone.
I just needed to lay down and take my nap while they kept changing the bags, and so that’s worked well for me.
How many bags of chemotherapy for each cycle?
I think there were about four to five. There were two chemo bags, but then I would have saline solution, Benadryl, and some other antihistamines typically.
The first ones they injected quite quickly. I think two hours for one bag of the chemo and another three hours for the Taxol.
How were you feeling physically after each infusion?
The Benadryl would wear off within the six hours, and I would feel fine to drive back. I would always have someone on call just in case.
I would say, “I should be done around four this afternoon, so just in case I don’t feel well, can you come pick me up?” But I was always able to drive myself home.
Did you experience any chemotherapy side effects?
Day 1 was I would just be tired, but I would feel great. I would go home and rest, but I would feel great. In the middle of the night or the next day, I would just get so nauseated, be so sick.
Those first few treatments, especially prior to my surgery, I felt like my insides were being electrocuted. It felt like I was being shocked on the inside, especially on my abdomen, where my cancer was.
But I could feel it in my arms, legs, hands, feet, and it felt like a shocking pain that was vibrating. It didn’t let up for a while. That would only be for a few days.
They had told me about the numbness in the fingernails, the mouth sores, everything, but I remember calling them up and saying, “I need some pain pills because nobody told me I was going to be electrocuted! This hurts.” That starts to subside.
»MORE: Cancer patients share their treatment side effects
What medications and methods did you find most effective with the side effects?
I really feel like I could take the anti-nausea medication, and I learned after the first one, I’d just take it that night when I went to bed [and] take it when I wake up. [I] just keep on that regimen. It really kept the nausea down.
I only threw up a few times during the whole process. After the first time, I was in a lot of pain. I always just took the meds beforehand and just kept taking them until I felt noticeably better, because it was so much easier to stay on top of it than to get behind.
The pain pills would help me relax enough to sleep, so I would just sleep through it. Once that feeling of being shocked inside would go away, then the bone pain would set in. I could have shooting pains in my bones; I could just have dull, aching pains.
My mouth would get really raw. You have all the neuropathy in your fingers and your toes. I had restless leg syndrome really badly. I couldn’t hold still without some medicine.
The doctors prescribed a lot of anti-nausea medications, three different kinds, different variations I could take. It was just trial and error [to figure out] what worked best for me. They would just give me pain medicines.
I don’t like taking pain meds. I was like, “I don’t want to come out of this cancer addicted to pain meds,” and they said no.
You’re in pain, and you need to take them. When you feel better, you won’t want them. We don’t see a lot of chemo patients come out addicted to meds.
As soon as I felt like I didn’t need to take them anymore, I really don’t think about them or want them at all.

Did the cycles of chemotherapy get better or worse?
My first chemo treatment, I actually felt better after four or five days. I got up and I did a few more. The more chemo, I had the worse it was and the longer I was down.
By my last round of chemo, I was flat in bed for over two weeks before I could get up and start moving around again. The doctors would say, “Really?” Yes, really.
I was really frustrated because they said I wouldn’t feel good for a few days, and I would be able to do more. I took that as I would be yucky for a few days, and then I’d be able to get up and function. That was not the case.
I still didn’t have energy to do anything. I could get up and do a few more things like drive my kids to school, mostly just drive around, get in and out of the car. Other than that, I was pretty weak and on the couch all the time.
I went in and [jokingly] said, “You lied to me, you guys. You said I was going to be moving, and I’m on the couch all the time!” They said, “You’re doing great! That’s normal.”
I said, “You need to tell your next patients that they’ll feel yucky and probably start to feel better, but won’t be able to do much instead of implying that I would still be able to be a mom and take care of my kids.”
Did you get a port or a PICC line?
The one thing from getting my second opinion at Stanford is she said, “Be sure you get a port. Make them give you a port.” I didn’t. They just said my veins were great, and I just did everything using an IV.
Now as time has gone on, I’m getting my blood drawn so often, and I was getting IVs for surgery, IVs for scans, IVs for chemo that I feel my veins are really shot.
I wish I had listened to that advice and asked for a port or PICC line.
At the time, it was like, “Well, my veins are great. They’re just doing these IVs.” But now it’s a lot more difficult. A lot of my veins have scarred, and I do wish I had kind of pushed or at least asked about getting a port and a PICC line.
»MORE: Read more PICC line experiences
Describe the plan for surgery (hysterectomy)
The cancer was all over my lower abdomen. It was in my fallopian tubes, my uterus, and the omentum. I’d never heard of the omentum before, but now I know what it is, and I don’t have one (anymore).
Originally my surgery plan was they were going to cut me open, remove all of my reproductive organs, my omentum, some lymph nodes. The tumors had been pushing on my bowels, so they were going to perform bowel reconstructive surgery.
Having the chemotherapy, I had to have another CT scan before surgery. That one actually came back showing what looked like a spot on the breast.
I was supposed to have three cycles of chemo before surgery and three after. I had four cycles before surgery because I then had to go get a mammogram to rule out breast cancer.
That came back clean, but it postponed the surgery a couple weeks because, again, you’re waiting for those appointments and those results. We just kept me on the chemo regimen. Then they said I would have two chemo cycles after surgery, but they lied and gave me three.
After the mammogram, from the result of the CT scan, the chemo had killed so much of the cancer and shrunk so much that they thought they could go in laparoscopically instead of cutting me open. My oncologist said, “We’re going to start laparoscopically. If we can’t do it, we will cut you open.”
Describe the actual surgery
There was still a good chance for bowel reconstruction surgery, but thankfully they were able to do everything laparoscopically. They removed all the cancer in my lower abdomen.
The fallopian tube that was really swollen, enflamed, pushing on the bowels — the chemo had killed all of that, so it just lifted right off the bowel. I didn’t have to have bowel reconstruction.
What seemed like bad news, delaying the surgery and having an extra cycle of chemo first, led to me having a much easier time. They were saying, ‘You’re going to be in the hospital for a week.’ I was there overnight.
I just was in a recovery room. I never made it into a real room. They just released me. I just had four little incisions on my