Sara’s Stage 3A High-Grade Serous & Clear Cell Carcinoma Ovarian Cancer Story
Sara I., High-Grade Serous & Clear Cell Carcinoma, Stage 3A
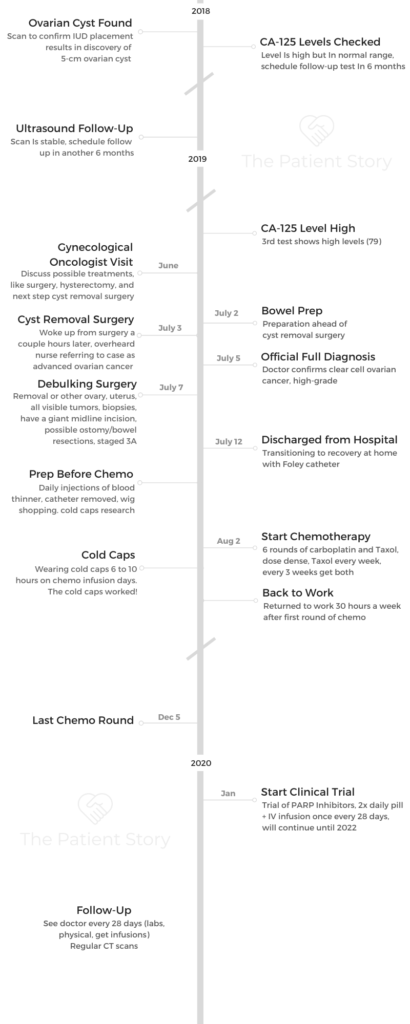
Symptoms: Random sharp pains, unrelated scan showed ovarian cyst
Treatments: Debulking surgery, chemotherapy (carboplatin & paclitaxel), PARP inhibitors (clinical trial)
Sara’s Stage 3A High-Grade Serous & Clear Cell Carcinoma Ovarian Cancer Story
Sara shares her stage 3A clear cell, high-grade serous ovarian cancer story, from getting diagnosed at just 34 years old to going through debulking surgery, chemotherapy, and a clinical trial involving PARP inhibitors.
She also dives deep into how she navigates life with cancer. Sara describes how she’s managed quality-of-life issues, including using cold caps to prevent hair loss, self-advocacy as a patient, finding her cancer community, dealing with scanxiety, processing the loss of fertility, and transitioning to survivorship.
You can read her in-depth story below and watch our conversation on video. Thank you for sharing your story with us, Sara!
- Name: Sara I.
- Diagnosis (DX)
- Ovarian cancer
- High-grade serous
- Clear cell
- Stage 3A
- Age at DX: 34 years old
- 1st Symptoms
- Random sharp pains
- Unrelated scan shows cyst
- Treatment
- Debulking surgery
- Chemotherapy
- Carboplatin
- Taxol
- Clinical trial
- PARP inhibitors
- Twice daily oral pill + IV infusion once every 28 days
- Two-year trial
- Sara's Story on Video
- First Symptoms
- Getting Diagnosed
- Treatment Decisions
- Debulking Surgery & Recovery
- How did you make the decision to pursue a debulking surgery?
- Self-advocating for more anesthesia pre-surgery
- Describe waking up from the surgery
- Transitioning to recovering at home
- Dealing with the mental recovery
- How long did surgery recovery take?
- When could you resume “normal” pre-surgery activity?
- How did you manage the Foley catheter
- Processing the situation at home
- Chemotherapy & Side Effects
- Describe the chemotherapy regimen
- Dealing with having to delay chemo because of neutropenia
- When did the side effects get the worst?
- Describe the Neupogen shots
- List all the chemo side effects
- How did you manage side effects?
- Did side effects get better or worse?
- Describe your work schedule during chemotherapy
- Working and working out were ways to feel “in control”
- Managing Hair Loss
- Clinical Trial
- How did you start a clinical trial the following month?
- Describe the preparation ahead of the clinical trial
- Learning how not to put things off
- Describe the clinical trial
- What drove you to participate in the clinical trial?
- Knowing about the drugs in the clinical trials
- Describe the clinical trial drug side effects
- Managing the side effects
- Why did your doctors say they wanted to pursue the clinical trial?
- The nature of ovarian cancer and recurrences
- Quality of Life
- The importance of self-advocacy
- You advocated to get paperwork for your own records
- The power of being an informed, engaged patient
- The need for more awareness about ovarian cancer
- Finding your cancer community
- The importance of having caregivers
- Guidance on how to support cancer patients
- Drawing boundaries for yourself as a patient
- Maintaining a sense of self and positivity
- Your tips on how to minimize “scanxiety”
- How have you processed the loss of fertility from cancer?
- How has the transition been to survivorship?
- Ovarian Cancer, High Grade Serous Stories
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
Sara’s Story on Video
How I Got Diagnosed
Treatment (Surgery, Chemo, PARP Inhibitor Clinical Trial)
Navigating Life with Cancer
First Symptoms
Tell us about yourself outside of the cancer story
I love activities — physical activities, outdoor activities. I have been a nurse for more than 15 years. I’ve always taken care of people, but my family is very, very important. I love to travel. I feel like everybody says those things, but I do.
I’m in the gym at least five days a week. Snowboarding — I skipped a couple of years and impressed myself with actually not face planting completely this past year. I’m completely down for skydiving, traveling, hiking, climbing mountains.
Whatever is going to be a new adventure for that day, I’m in for it.

What were the first signs something wasn’t right?
About a couple years ago, I had random sharp pains. We tried to figure out what they were. We couldn’t figure it out.
My mom had breast cancer, so I always veered away from hormonal birth controls just for that reason. Also, because I just didn’t feel right on them.
Eventually, I ended up getting an IUD placed. They do a one-month follow-up ultrasound, so they did that follow-up ultrasound and saw a cyst on there.
My doctor was like, “Okay. There’s a cyst. It’s a decent size. Let’s monitor it and see,” because I wasn’t really having symptoms.
Describe the follow-up
We followed it up six months later, and things were fine. My CA 125 level was still normal, but on the higher side.
Then at my one-year mark, she had done another ultrasound and had some concerns that it had changed. In hindsight now, if I had known more of what the ovarian cancer symptoms were, I may have been like, “Yes, I have had some bloating, or I have had some like unusual things as far as that goes.” But I was completely unaware of any of the symptoms.
Meeting with a gynecological oncologist
I went in with the fact that I didn’t really have any symptoms of anything. I did end up having to meet with the gynecologic oncologist for surgery.
He was more concerned. I think I still was very oblivious. I thought there’s no way that this was cancer. He’s telling me all of the possible treatments, like the surgery, the hysterectomy, all this, and that.
I’m like, “We’re having a cyst removed. I’m going back to work in three days. It’s going to be laparoscopic.”
Getting Diagnosed
When did you realize things were pretty serious?
I feel like I went in pretty optimistic. About four minutes after I got to pre-op, when they did a urine pregnancy test, it came back positive.
Then I was like, “That’s not good.” They had to do some blood work. They were trying to convince me that I was pregnant, and I knew very well that there was zero chance of being pregnant.
I knew that that was not a good sign. You don’t have a positive pregnancy test. A tumor can cause a positive pregnancy test. That’s when I started having the, “Oh, no. This is not a good situation.”
Describe the cyst removal
I was going to have the cyst removed. My doctor and I talked at length on what the plan was, and I had to go into it positive.
I knew that I had to go into it with my head on straight, so I had told my doctor, “We’re going to go in. We’re going to remove the right ovary. We’re going to do the cyst. Then we’ll make a plan from there.”
I was not willing to sign consent to have a hysterectomy. I wanted kids still. I hadn’t had kids. I was very much trying to control what I could control, and he was very much trying to lay out the facts of things.
The doctor finally said, “Okay, we’ll do surgery,” because he was still concerned about this positive pregnancy test.
What do you remember of the surgery?
I didn’t go into the operating room (OR) until July 3rd, and it was late at night. We didn’t go until three o’clock at night because they had to wait for the surgeon to come out, talk to me, and everything.
We went in, and I was in there until about nine or ten o’clock at night that night. I ended up coming out of the OR and was immediately admitted just because it was a long surgery. I stayed in the OR for so long.
We also didn’t really know what’s going on at that point.
I woke up, and I just had some small, tiny laparoscopic incisions. I was like, “Is this still a cyst, or we don’t know?”
You heard your diagnosis by accident
When I was in the wake-up recovery room waiting to go to my room, I heard the PACU nurse call report up to the floor and said, “I have a 34-year-old female with metastatic ovarian cancer.”
Now, I’m completely out of it, have no idea what’s going on, and I’m the only person in there. It’s nine, ten o’clock at night in the recovery room. There’s nobody there. It’s me and the nurse. I’m sure he didn’t want to be there.
That’s when I was like, “Oh, this is why we are staying the night. This is why we are not going home.”
He just closed up surgery after taking out that cyst and said we would have to talk about it. I ended up getting admitted to the hospital. Then my family was still all there. We went to the room. I broke down a little bit and was like, “It’s cancer. It’s cancer. It’s cancer.”
No one in my family really knew about the cancer because I told my doctor he wasn’t allowed to tell my family until he told me. I was the medical one, and they didn’t understand, so they didn’t know anything.
They weren’t even prepared for me coming out to OR to start telling them that I had cancer. They weren’t expecting that either because I hadn’t talked to anybody. I had just heard about the cancer myself.
Then my doctor came in the next morning, and he said, “We have to make a decision. We have to wait and see if it is cancer. If it comes back as this kind of ovarian cancer, we can just do chemo and stay the course. If it comes back as this, then we have to go back for more surgery.”
We just had a waiting game at that point.
Processing the official cancer diagnosis
On July 4th is when I found out it was cancer. Up until that point, they had done a lot of work with my bladder. I couldn’t pee. I had to get a Foley catheter put in; my electrolytes were all off. I was a disaster on July 4th.
How did you handle those first days in the hospital?
I was very much not myself. I wanted out of there, and I wanted to escape. I’d let myself do what I wanted to do. I was like, “I’m going to go for a walk. I’m going to do whatever.”
My big thing was I needed to get out of my room. I needed to get out of that hospital room.

We had a big courtyard in the hospital that I was able to go to for a long time, and I honestly spent probably the entire July 4th out there with my Foley catheter hanging out, not caring, because I did not want to spend any time in that hospital room.
I had lots of visitors come in throughout. That helped a lot. I had tons of visitors come in and out. I was still on a full liquid diet for many more days.
Getting the full cancer diagnosis
On July 5th, my doctor came in and was like, “We’re going to keep you. We don’t know what’s going on, so we’re going to have you stop eating. I’ll come in, and I’ll talk to you about things.”
He came in finally at 5:00 p.m. and told me that I had clear-cell ovarian cancer, high-grade. That’s when I just straight broke.
I’m one of the rocks in the family. I’m the medical one. I know what’s going on for the most part. I’m the one who’s going to support the family, but I broke.
I completely lost my mind. I ripped off my shirt that I had on. It was down to a bra and shorts and just basically screaming and crying.
It’s funny now because at the time, I never wanted to put myself back in that spot because it was when I just broke. My whole family watched me. My whole family didn’t know what to do. No one knew what to do with me. I was completely irrational. I didn’t want anyone touching me.
My cousin had been there just visiting, and he was getting ice packs for the nurse because I was sweating. It was so hot.
Finally, I almost was like, “Okay. I just needed out of that room.” I went and found my nurse assistant, and I was like, “You need to dump this Foley out. I need to go for a walk. I need to get out of here.” I just randomly wandered the hospital at that point. I just needed to get out of there.
Treatment Decisions
How did you break the news of the cancer diagnosis?
I had a very close group of friends. My family was all there. A lot of my friends knew I was going in for this cyst removal procedure. They were aware of that.
I didn’t really tell many people about it just because I didn’t know. I didn’t want to be like, “Okay. I’m having an ovarian cyst removed, and I need attention.”
I’m very much someone who is very independent, so I didn’t want to go there with people. Once I found out that it was cancer, I started to tell some people. Obviously, the news trickled down through my family.

After I had my major debulking surgery, one of my best friends started a GoFundMe for me because I live alone with a single income. I was going to be out of work.
She typed up a story, and it got out really fast through that way. I ended up having a blog at one point just to take it away from my Facebook.
It goes back to the whole issue of control and the fact that I didn’t want cancer to be everything at that point. I was still trying to be in denial as well.
Tip: bloging helps prevent repeating information all the time
The doctors would say stuff to me, and I would have to explain it to my family. Then it’s like, “Okay. Now, I’m just going through it over and over again multiple times.” I ended up being like, “Okay. This is where I can put updates, and everyone can look there.”
My mom would try to do some things, and then I’m like, “Just send anyone there.” Everybody goes there. They can read there. They can follow there.
I had so much love and support. It was great, but it was also so overwhelming, where everybody wanted to know how I was. I was like, ‘I actually don’t know how I am.’
My best friend, Courtney, was very helpful with going through this group of friends, just trying to keep them in the loop. My brother was great. My mom was great.
There are so many people who just were great to take pods of people and keep them informed, helping the information trickle down. Eventually, I don’t even know if I eventually just blurted out on Facebook and said it, or if it just got to enough people and that’s how they found out about my cancer.
It was a weird time frame, especially since we didn’t think I was having surgery, and then everyone’s like, “Oh, you had surgery? Oh, my God. You have cancer. When did this all happen?” I was like, “Well, I didn’t think it was cancer either.” I didn’t want to bring that attention ahead of time.
Did you consider getting a second opinion?
I did not consider getting a second opinion. I went to Karmanos Cancer Institute in Detroit. It’s basically connected to the hospital that I work at.
I work in the pediatrics [department] and across the courtyard that I spent my entire time I was in the hospital. It was actually funny that I was walking around with a Foley catheter in front of my colleagues.
I would walk there. It just was the first place that I knew. I had gone there for my mammograms and all that stuff because I started getting mammograms so young because of my mom.
My OB-GYN recommended them, and then someone else recommended them in the beginning when we were just trying to look for someone.
He encouraged me to get a second opinion. He said, ‘If you want to get a second opinion, go get a second opinion.’ My only other second opinion would have been through a main hospital.
I honestly think having a cancer center made a huge difference on a lot of things. I see a gynecologist and oncologist. He runs my chemo. He runs my treatments. He runs all my stuff.
In the beginning, was I super overwhelmed? Yes, but at that point, I have cancer. It’s like when I first was going in for surgery, I’m like, “Oh, I may never see you again.” I kept playing dumb.
I just started researching what the treatments were. There wasn’t much of a difference. Since then, I’ve established a relationship with my doctor. From follow-up visits, I’ve established quite a relationship with the staff there and everyone else there.
Importance of good relationship with doctor
My own physician gave me his cell phone number the day I was diagnosed in the hospital. He said, “If you need anything, you can text me anytime.” We have a really good communicating relationship.
If it were to come down to later down the line, if I were to have recurrences or something like that, maybe I would go somewhere else.
He’s fairly young as well. I feel that he’s going to stick with me for quite a while, so that’s nice.
I do think second opinions are great for some people. You have to trust your physician and your team. You have to have that communication. Everybody’s different. Everybody has different personalities.
In the beginning, I was like, “Maybe he’s not good for my personality,” but then we’ve grown on each other where I just have trust in my team.
You’ve got to be able to trust them — not even that they’re going to do the best thing for you, but that they have your best interests in hand. Sometimes, they’re going to tell you no, and that’s because it’s in your best interest.
Debulking Surgery & Recovery
How did you make the decision to pursue a debulking surgery?
I knew that I wanted to get out of the hospital. Again, I’m a firm believer that you need to have communication with your team.
You need to advocate for yourself. I was like, ‘What’s going to get me out of the hospital faster? What’s going to have a faster recovery?’
I had talked to my doctor about that, and we talked about doing a nerve block versus an epidural at surgery time because I was like, “An epidural keeps me in the hospital longer. A nerve block could be less.”
The surgery involved making a giant incision right below the rib cage, all the way down to the pubis bone, and opening up and taking out what needed to be taken out.
Sometimes I would forget that I had this major surgery, because it is major. Everything’s taken out and put back together. They looked at things. Once you’ve had surgery, you see the actual incision. You don’t see what they’ve done on the inside.

Self-advocating for more anesthesia pre-surgery
I was very firmly telling them before surgery that I didn’t want to remember going into the operating room. I remembered going into the operating room my first surgery. I remembered it was just cold and sterile, and I was alone and scared.
I begged the anesthesiologist to give me some more medicine to keep me in la-la land before surgery. Again, a little bit of my control just wanting to not be there at that moment. I feel like a lot of it was just trying to escape those moments.
Describe waking up from the surgery
My surgery was seven hours long. The next day, I got back out of the operating room. It was probably ten or eleven o’clock at night when I got back to my own hospital room.
I ended up waking up in the recovery room with no nerve block, not any pain medication on board. They thought I was too sedated, so they didn’t do it.
I was in excruciating pain from not having that. I still do not regret the fact that I didn’t get an epidural. Once the nerve block worked, it was really, really good.
As a pediatric surgery nurse, I knew that number one was I had to get up. The next morning, I woke up and was like, “We have to walk. I need to get in my normal clothes. I want out of this gown.”
I ended up coming off pain medications pretty fast. I ended up walking as much as I could. I was just moving around. As soon as I could, I got moving.

Transitioning to recovering at home
My nurses were great. I ended up having to go home with a Foley catheter. That’s when I feel that a lot of things hit home.
The pain was bad from the surgery, but I never felt that it was so bad. I was pretty physically fit beforehand. I felt strong. I knew that my arms were strong to help me get in and out of bed. My legs were strong to get me in and out of bed. I just tried to not use my abdominal muscles.
Just from being a nurse and knowing positioning and stuff like that, it was really easy for me to get moving. The fatigue was something that started hitting at that time, where I’m like, “I’m going to walk down the hallway. I want to take a nap now.”
Dealing with the mental recovery
I remember I had talked with my doctor as soon as I was diagnosed and said, ‘I’m not going to be okay. I want to talk to somebody.’
They sent a psychologist in there. She may have come in the day before surgery. She came and found me the day after my surgery, later on that day. I was just crying. She asked, “What is wrong with you?” I’m like, “I’m tired.” She’s like, “Why don’t you sleep?”
I had been trying to entertain everybody around. It’s hard to take care of yourself. You forget that you’re a patient. You’re like, “Okay, there are people here. I need to stay awake.” My family was like, “Just sleep. Just sleep. Just take a nap.”
It was very hard for me to step back and be the patient and be like, “Oh, your body needs this. Your body needs rest.”
Then the next day, I was sitting there just sleeping all the time. I felt much better. I felt that there was so much of me that knew what to do, but then so much of me that needed to be told what to do.
That’s where my two worlds were clashing, where I was like, “I want to be better. I want to be home.” Then the other part of me was like, “You’re not there.” It was this kind of meet-in-the-middle situation after surgery.

How long did surgery recovery take?
As far as recovery from surgery, it took two months, if not longer. I felt really good at my three-and-a-half-week post-op visit with my doctor.
But then I started chemo about three weeks after surgery. It was almost like, “Now, this is just happening.” Probably 14 days after surgery, I was much, much better.
I was stubborn. My sister-in-law had a bridal shower. I got out of the hospital Friday. The bridal shower was Saturday, and I went.
My brother had taken such good care of me. I was so excited for their shower. I needed to be there.
Do I regret it? Not at all, but it was so much. It was very exhausting, but I did it, and I’m so happy that I did do it, even though I was miserable the entire time.
About 14 days after, I was able to get in and out by doing things, moving around. The Foley catheter was gone. Things were much, much better.
When could you resume “normal” pre-surgery activity?
As far as working out, my doctor said I could start three, four weeks after surgery. You can wait longer.
I had a five-pound weight restriction from surgery until six weeks. I was only allowed to lift five pounds until six weeks. I also had four weeks of no driving.
As with most people, they know that narcotics cause constipation. I weaned myself off the narcotics as fast as I could. I went to just Motrin, Tulane, Tylenol. I didn’t want to take any medicine.
Every single time I told my doctor, “Can we stop taking this one? Can we stop taking that one?” He’s like, “Just let it happen for a while.”
At around four weeks, I started light jogging. Once he gave me the go-ahead, I started to lift weights again. It was probably at least three months until I could do a sit-up. I would do sit-ups, and if I could do them, the next day I was in excruciating pain.
Everyone would be like, “You did have a major surgery.” I had to be reminded all the time, because I was so mad that everything else was starting to work and that was not working. I played the whole game that I tell my patients, “If it hurts, don’t do it. If it’s sore, it’s okay.”
I went with like, “Okay, I just can’t do abs.” Once a week, I would try to do it again, and then I would be like, “No, not time yet.” I played around with that. I probably would say at about three months I was fully surgically healed. At about six weeks, I was feeling much more like my normal self.
How did you manage the Foley catheter
The first surgery happened, and they had to do some stuff where they had to check the bladder. Part of the cyst was against the bladder. My urethra was basically pretty swollen.
The next day, I was in and out of the bathroom peeing enough. Then I just didn’t feel that I was peeing enough. They asked me, “How are you?” I was like, “I don’t know if I am emptying my bladder all the way.”
They did a bladder scan, and they were like, “You have an ova leader in your bladder right now.” I was like, “Oh, I don’t really have to pee that bad.” I went to the bathroom, and I peed literally like 800 milliliters, and they bladder-scanned me for leader cells.
They have no idea how much I had in there because I’d just gone to the bathroom. They were like, “You’re not emptying your bladder. We have to put a Foley catheter in.”