Stephanie’s Stage 4 Primary Mediastinal Large B-cell Lymphoma (PMBCL) Story
Stephanie V., Primary Mediastinal (PMBCL), Stage 4
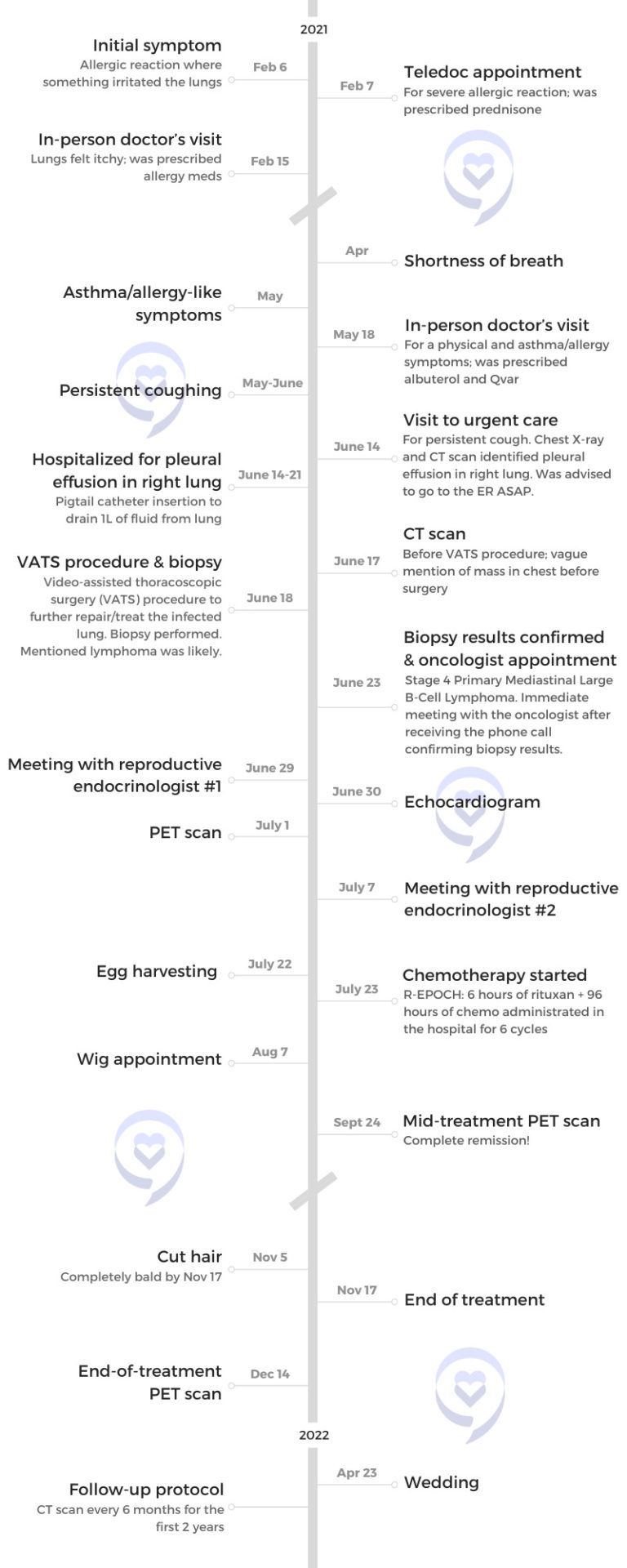
Symptoms: Asthma/allergy-like symptoms, lungs felt itchy, shortness of breath, persistent coughing
Treatments: Pigtail catheter for pleural drainage, video-assisted thoracoscopic surgery (VATS), R-EPOCH chemotherapy (6 cycles)
Stephanie’s Stage 4 Primary Mediastinal Large B-cell Lymphoma (PMBCL) Story
After her father’s Hodgkin lymphoma diagnosis, Stephanie still never thought her persistent cough was anything more than allergies or asthma. But after her cough progressed and she couldn’t do or say anything without coughing, she finally decided to go to urgent care.
As doctors cleared fluid from her lungs, they found a mass in her chest. She was then diagnosed with stage 4 non-Hodgkin’s lymphoma only two years after her dad’s diagnosis.
She voices how she processed her diagnosis, how she advocated for her health, and how her father’s diagnosis impacted her cancer journey.
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
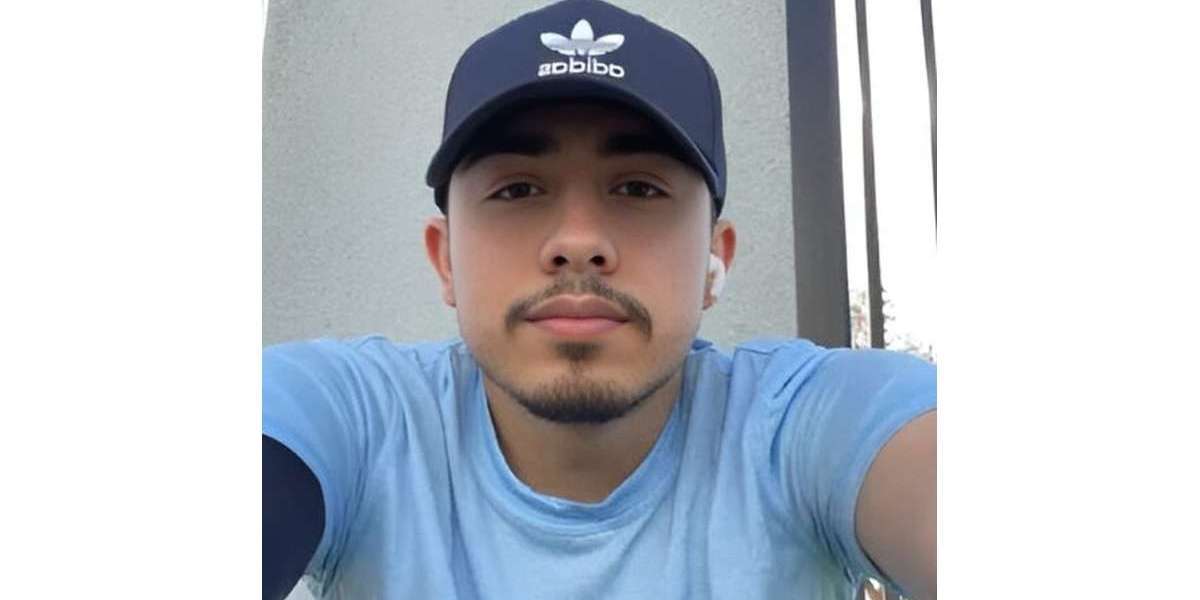
- Name: Stephanie V.
- Diagnosis:
- Primary mediastinal large B-cell lymphoma (PMBCL)
- Staging: 4
- Initial Symptoms:
- Allergic reaction
- Lungs felt itchy
- Shortness of breath
- Asthma/allergy-like symptoms
- Persistent coughing
- Treatment:
- Pigtail catheter for pleural drainage
- Video-assisted thoracoscopic surgery (VATS)
- Chemotherapy: R-EPOCH

Introduction
I work in private wealth management. I manage a team that oversees investing high net worth accounts. I enjoy developing my team members and associates that report to me; that’s always been something I’ve been interested in since I started with the company. I’ve been with them for almost eight years so it’s been quite an endeavor in that sense.
In my spare time, I like remaining active. I’ve danced since I was 2.5 years old. My passion was always ballet, but I also did tap, jazz, [and] contemporary.

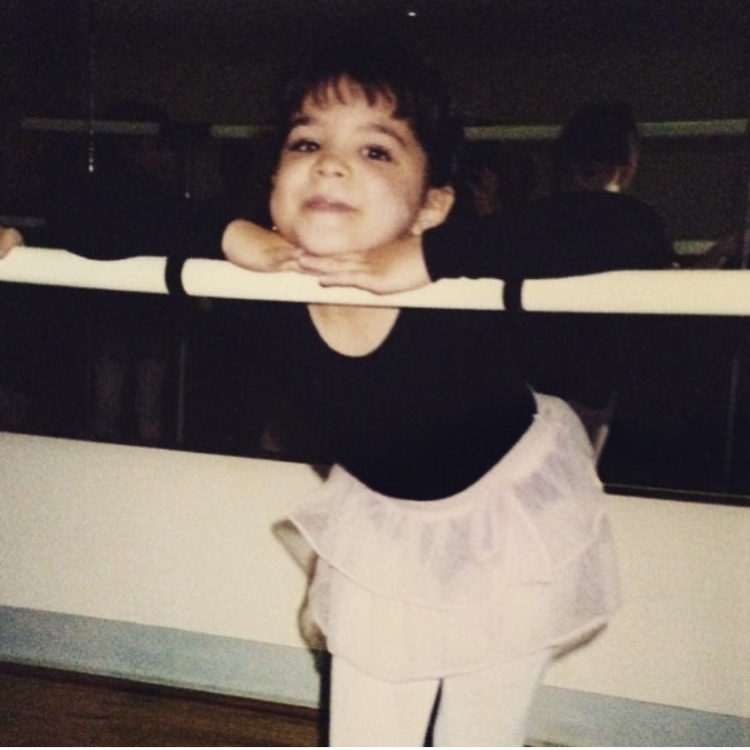
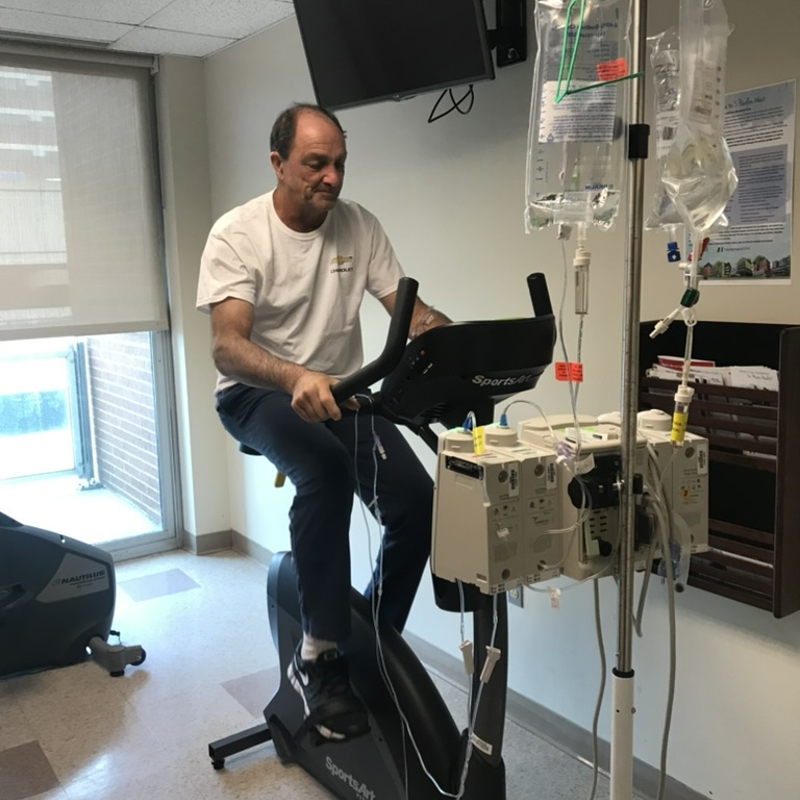
I studied dance in college with a focus on economics. I did dance on the side knowing that it wasn’t going to be my end goal or career, but something that I kept up with. Now I’ve translated that into exercising on a regular basis and trying to keep active. Remaining active has always been something important to me.
In the winter, we go skiing and spend time with family. It’s always been very important to me.
My father’s Hodgkin’s lymphoma diagnosis & journey
We’re very healthy individuals, my dad specifically. He works in construction so [he has] an active job. He’s very tall, very lean, [and] very healthy.
We started to notice [that] he had this cough in late 2017-early 2018. He works in dirt so we thought, Oh, he’s inhaling too much dust. He’s just coughing it out. It did become very persistent and we said, “Maybe he should go to the doctor [to] get this checked out.”
He hadn’t been to a doctor in 20 years; didn’t really need to go because he’s a healthy person.
His tumor was so dense [that it was] difficult to get a good sampling. He had many biopsies because every time, the results came back inconclusive.
The doctors knew that he pretty much had Hodgkin’s lymphoma. He had every symptom in the book: night sweats, weight loss, coughing, and itching. We knew he was sick, but we couldn’t get that confirmed diagnosis.
After about three or four months of going back and forth and finally getting that confirmed diagnosis, he was able to start treatment. I forget what treatment he did, but I consider it an old-school treatment. It wasn’t the ideal treatment that they wanted to do for him, but they did that one I think because of insurance purposes.
He went through his treatment cycles and had a clean scan, but within three or four months, he had the cough, itching, [and] night sweats again. It came back.

The next plan was to do a stem cell transplant where he was his own donor. Now, this is [the] summer of 2019. He was in full isolation. We were wearing masks and gloves to visit him. We could have visitors at that time as it was pre-pandemic. He started to do immunotherapy as [a] maintenance treatment after the stem cell transplant.
He’s been good ever since, thankfully. He has his regular checkups with our lymphoma team at the cancer center. He’s now doing one-year scans but has a checkup every six months. He was pretty much confirmed clean before the pandemic started.



Initial symptoms
I didn’t really have any symptoms other than a persistent cough. I pinpoint this back to a day in February [when] I might have had a food allergy mixed in with some dust contact shortly after. I guess my immune system might have been down and couldn’t fight whatever was coming into my body at that point.
I did a teledoc appointment that weekend. My face was very swollen and I was prescribed some prednisone. A few weeks later, I still didn’t feel very well. I still had itchy lungs.
I went to the doctor in person. They prescribed allergy medication. It was winter in New Jersey. I already have food allergies [and] eczema and so I said, “Okay, add it to the list.”
I noticed shortness of breath in April 2021. I was actually supposed to get married [that month]. My husband, then fiancé, [and I] were in Newport, Rhode Island, for our would-be wedding date and we were walking around. Our hotel was over a little bridge that had an incline.
I noticed that I was getting out of breath and we were just walking around, not even having anything to drink. It was just a nice day and I was very out of breath. I had to stay in the hotel room more than we’d liked.
May 2021 was when my symptom progressed. I started to have a cough and more asthma allergy-like symptoms where I definitely was more short of breath. I went to the doctor and they said, “It’s probably asthma. I’m going to give you two inhalers.” One was albuterol and something called Qvar, which was a little bit more intense. I said, “Okay, this was probably coming.”
Coughing progressed
By June 2021, my coughing had progressed a lot more where I really couldn’t do anything or say anything longer than a sentence without coughing nonstop. It was impacting my work.
I speak a lot. I do training for my team and I couldn’t get through a presentation or even a sentence without coughing so that was becoming a lot more noticeable. Definitely, not a time when you want to have a persistent cough. It was confirmed many times [that I] didn’t have COVID.
After not feeling well to the degree that I was that morning, I finally decided to go to urgent care. I was going to go that week, but I realized that morning I had to go. I did get sick from coughing so much. I think my body was probably doing it out of habit at some point, too, just because I couldn’t go more than two minutes without coughing.
I was convinced it was pneumonia at that point just because [of] the way I was coughing. I just couldn’t breathe.


Pre-diagnosis
Going to urgent care
First, I went to urgent care where I demanded an X-ray. They said, “You might have COVID.” I knew I didn’t. I asked for a chest X-ray.
Before I even put my clothes back on, they said, “You have something that’s called a pleural effusion or an empyema and you need to go to the emergency room right away.”
This was a different medical group than where I ended up getting all my treatments. They said, “Go to this hospital. We’ll call you in.”
I said, “If this [has] anything to do with my lungs, my dad already has a pulmonologist that’s at a different hospital network. We know people there. I’m going to this emergency room instead.”
They called the hospital that I wanted to go to. You need to advocate for where you want to go [and] what you want to do because it is all about you at that point.
Going to the emergency room
I did get to the emergency room. This is the middle of the day on a Monday [so there were] a lot of people in the emergency room, probably about 50 people waiting. I [was] waiting my turn and the second I said my name, they said, “We’ve been waiting for you.”
They pulled me into another room, threw a gown on me, [and] started to do all these tests. I’ve never been to the hospital other than when I was born. I go to the doctor [for] my yearly visits. All these tests, all these patches on me, [I was] getting a little nervous.
Then they said, “Okay, we have your blood.” At urgent care, I did not have a fever. The second I got to the emergency room, I was 101°F or 102°F. I think my body was just saying, “Okay, this is time. We’re going to show every symptom we have now.”
They put me on a gurney and rolled me into my other room. I did start to cry a little bit because I was very overwhelmed. I was with my sister and at first, [we] were very lighthearted. We make a joke out of everything so I was said, “Oh, I guess it pays off going to urgent care first before going to the ER because they can give a heads-up.”
Everyone else is either walking to an exam room or in a wheelchair, but I get a gurney and I said, “Okay, no one’s really telling me what’s going on. They’re just all acting a little fast.” That’s when I got a little bit nervous.





They told me I had about a liter of fluid in my right lung that needed to be taken out. They couldn’t do it that day, but they would be able to do it the next day. Not only was this my first trip to the hospital, [but I’m also] now automatically staying [the] night.
I was admitted on a Monday. They didn’t know it was cancer until Friday. There’s so much fluid in my lung that they first thought pneumonia or pleural effusion and they need to get that out. Once they cleared out the lung, that’s when they did the CT scan and saw the mass in my chest.
They didn’t tell me until Friday. They were just concerned about what was happening in the lung and how to treat it. I don’t know if they didn’t care to look at it. I don’t want to make it sound like the doctors were being careless, reckless, or anything like that, but I think they were just addressing that issue first.
Rolling into the OR, they said, “Oh, by the way, can you sign here? Because we’re also going to biopsy this mass in your chest.” All I remember thinking was, Interesting. My dad had a mass in his chest, but at that point, I still didn’t think it could ever be lymphoma. I said, “Oh, that’s interesting,” and the next thing I know, [I’m] getting a mask on me and going to sleep.
There’s so much fluid in my lung… Once they cleared out the lung, that’s when they did the CT scan and saw the mass in my chest.
Requesting a chest X-ray
That is a lesson learned from my dad’s experience. He is considered young by most standards so I’m considered extra young.
When he had the cough, I think he had gone to the doctor maybe two times, one for a physical because he hadn’t gone in so long.
At that point, I think anyone over 50 should be getting a chest X-ray from what I understand. But that first doctor did not do a chest X-ray so he could have seen something earlier.
When I was coughing so much, my mom said to me, “When you do go, get a chest X-ray because that’s where we’re going to start every time,” not thinking that this was going to turn into stage 4 cancer.
We said, “Okay, it’s what? $12 for a chest X-ray with insurance or something like that. It’s very harmless and we’ll just cross that out.”


Getting back from the OR
I wake up. They cleared out my lung, but there was still a lot of infection in there. While they were in there, they took [a] biopsy of the chest and the lung as well.
I get rolled into the surgical ICU for recovery. This is pandemic time so we only had two visitors at a time. A couple of minutes later, my mom, dad, and fiancé came in. I thought, “Interesting. We have three guests. How did we do this? This is very nice.” If my sister was there, that would have been the goal but, obviously, we can’t push it.
I had my important people there and I was asking my fiancé because he was sitting right next to me. I asked, “ Did they say anything? They mentioned a mass [in] my chest. Did they mention anything about it? I don’t know what that is.” He just shook his head and said,, “I don’t know about that.”
I have a popsicle in my mouth because I had a sore throat from the anesthesia. I’m licking away and I said, “Okay, well, this is it, guys. I’m going to be here for a couple of days, go home, and we’ll all laugh about this later.”
She immediately called the cancer center and said, ‘My husband’s a patient and I believe my daughter’s about to be a patient. What can I do?’
Diagnosis
Getting the official diagnosis
The doctors come in. I thought they were just going to go through the surgery and say what I have to do to fix myself. It was actually a team of surgeons. They can’t say it without having [the] biopsy results, but the doctor was very confident that I had lymphoma in my chest.
I looked at my fiancé and my parents and asked, “Are you sure you didn’t pull my dad’s files? We’re in the same hospital unit and he had [a] mass in his chest. Dad has lymphoma, not me.”
They left. My mom’s face, I knew she already knew the information. What I came to learn was the doctor called her, telling her that I was out of surgery. He said, “I was able to look at the actual mass and at the cells and I believe it’s lymphoma.”
She said, “Please do not tell my daughter until I get to the hospital with her father [and] her fiancé. She cannot hear this news alone.” That’s how they got three visitors in the hospital.
The second she got that phone call, she went into her mode. This is Friday afternoon. She immediately called the cancer center and said, “My husband’s a patient and I believe my daughter’s about to be a patient. What can I do?”

We didn’t have the biopsy results but she wanted to get our names on the board immediately.
She did say she paused because again, I’m in this transition of getting married and my spouse might be the one who wants to make some decisions, too. She had to pause and turn to my fiancé and say, “Are you okay if I start running with this?” He said, “Please. Go right ahead,” because she knew the road to take and we just had to get right in there.

Reaction to the cancer diagnosis
I still think it’s absolutely bizarre. We’ll never understand. I’m not sure when I’m going to say, “I just had stage 4 cancer and my dad had it, too, all within five years.”
I was very calm. I don’t think it actually hit me until someone mentioned family planning. That was hard to understand, especially as I’m trying to get married and I have someone who is looking to me to start a whole life together. I thought,“Well, this might get cut short.” But otherwise, I was calm.
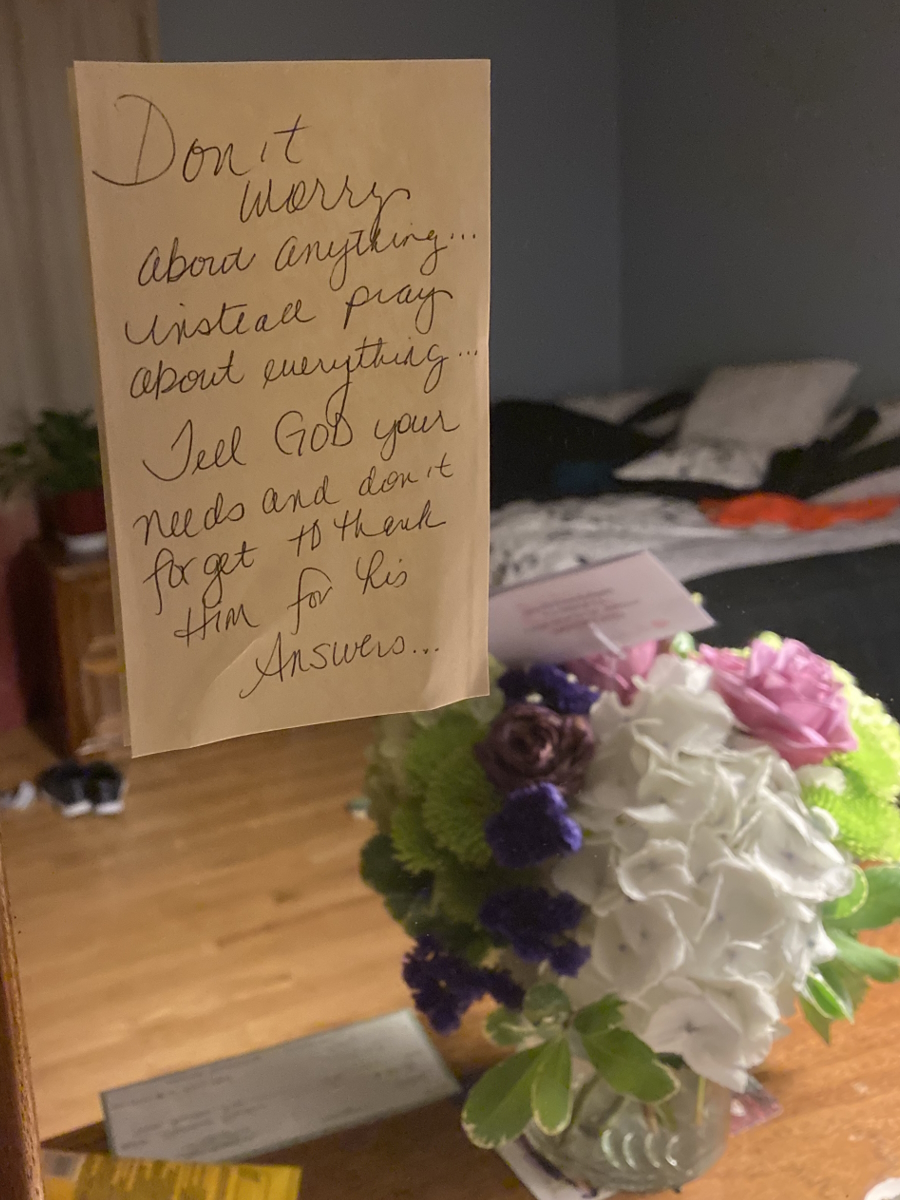
I like to deal with things as they come. I accept it and say, “Okay, what are we going to do about this?” I do that in my work. I’m learning in my life, too. That’s not to say I don’t have anxieties or stresses about it, but I do think I remain calm under these pressures.
You never want to see that look on both my parent’s faces. You never want to be the cause of their worries. I think that that happens naturally when you become a parent, I’m sure. But to this degree, I don’t think you ever want that.
My mom’s got her way of reacting [to] things. But I know with her, I was in good hands. We knew what we were going to do. It was going to get done.
With my dad, [it] was hard to look at him, and over the course of the next couple of months, too, because he knew what I was about to go through more or less. You don’t want that for anybody.
He said, “If I could trade places with you, I would ten times over,” and you just don’t want to hear that. I don’t want him to go through it again, too.
I think it’s more stressful for me to see everyone else worry about everything… You don’t want to be the cause of people’s worries and restless nights.
We’re [a] family who jokes and tries to make light of things when we can. Looking at my fiancé at the time, I said, “You can get out now. It’s going to get ugly.” My mom said, “Yeah, James, we’re going to give you three tries and after three, you’re in. So here’s your first try. You can go.” Of course, we’re joking and, obviously, he wouldn’t leave.
You don’t sign up for those things. No one does. But we didn’t even say “I do” yet and this is the “in sickness and in health.”
I think it’s more stressful for me to see everyone else worry about everything. That was the heaviest weight to carry. Not my health or what I had to go through but seeing other people go through it. Seeing it with my dad, I knew as a loved one how that felt. You don’t want to be the cause of people’s worries and restless nights.
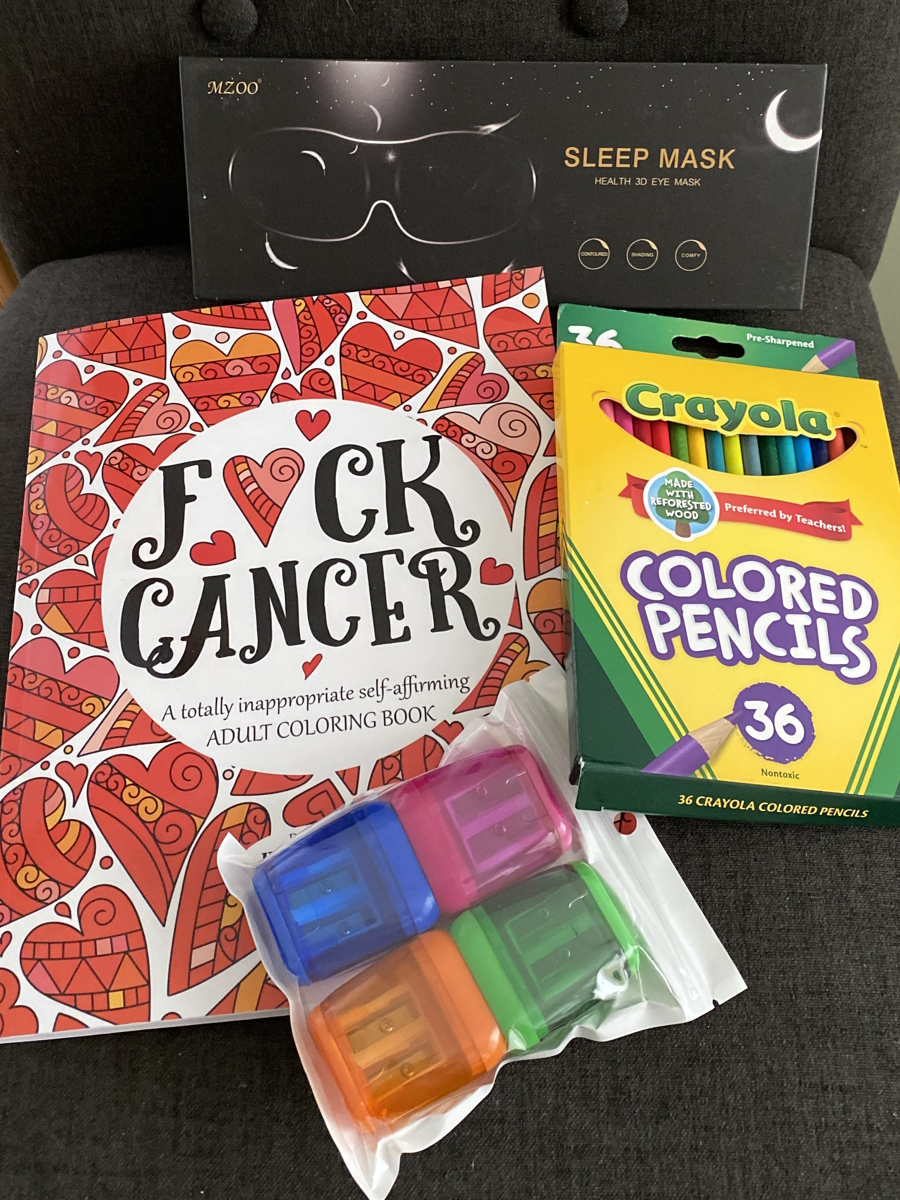
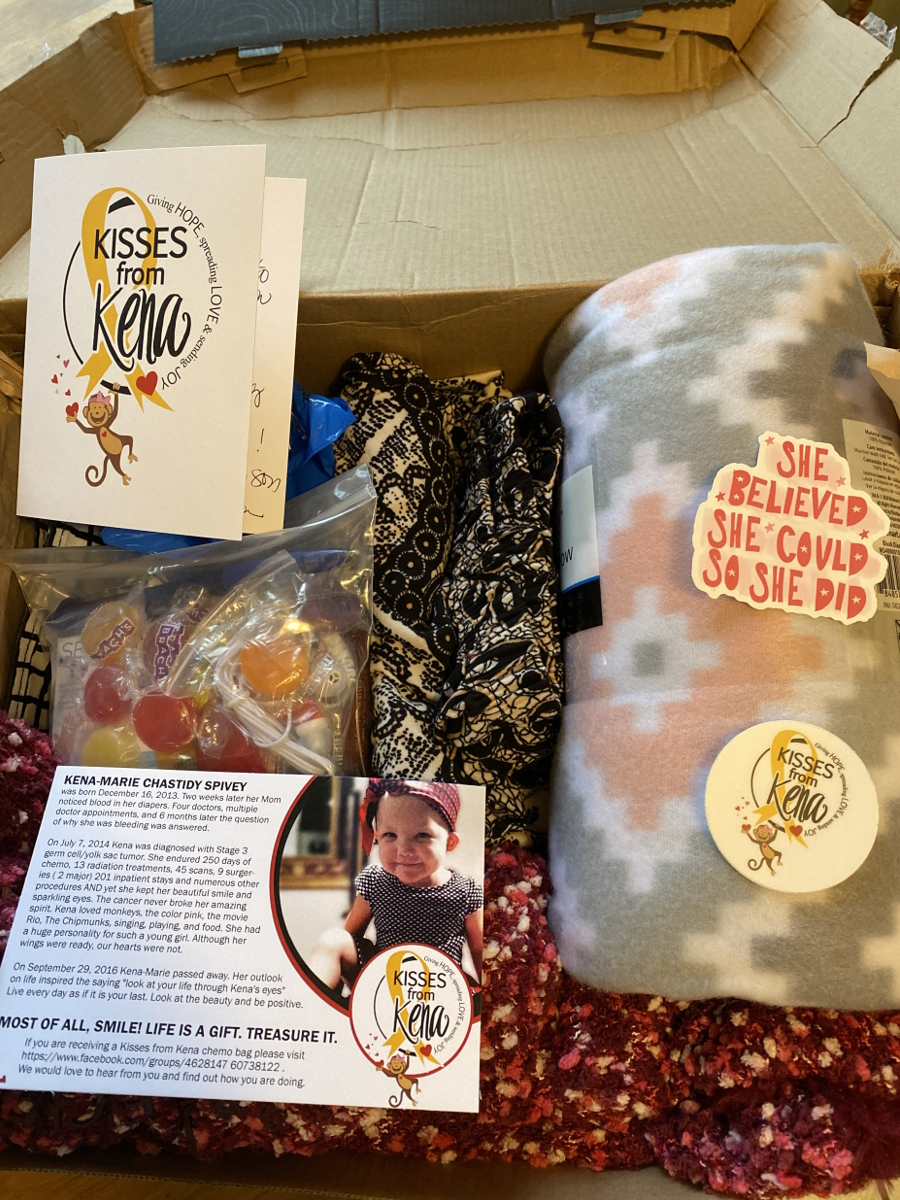
Having a support system when you get your cancer diagnosis
I wouldn’t have expected it any other way. There’s no scenario where they wouldn’t have been there. I think that’s the part that she gets done every time, like having those three people in the room knowing that this is life-changing news. If she could get my sister in there, too, she would. I think that’s just the way she does things.
You can’t just hear about it by yourself with a SpongeBob popsicle stick. You need those people around you. That’s when day one starts.
You’re never alone in this process. But to hear that news, you cannot be alone. For her to do that, that’s the person that she is, knowing that she’s done it before.


Treatment
Starting treatment after cancer diagnosis
It was about a month afterward. I got the confirmed diagnosis a few days after I was released from the hospital. I got [a] phone call from the surgeon.
I called my mom right away and said, “Okay, it is lymphoma.” There was a case where it could have been some lung disorder or disease that would still be treated with chemo, but it wasn’t cancer, so that was also a blessing in disguise. We said, “Well, we know lymphoma so we’ll take it.”
My mom immediately called the cancer center and said, “We officially have the diagnosis.” The surgeon was about to call the cancer center as well.
The cancer center called me back and said, “Our oncologist has an appointment open [in] 45 minutes. Can you go?” My mom’s at work, I’m at my house, and the cancer center was about 25 minutes away. I said, “I don’t know if we can get there. Let me call you back.”
I called my mom. I said, “She’s available in 45 minutes, but you’re at work, Mom.” My mom said, “No, we’re going. I’m dropping everything.” She had an amazing boss at the time who was so understanding and knew everything about my dad’s history. Anytime anything happened, she would just say, “I have to go,” and he said, “Okay.” That’s it, no questions asked.
She picked me up. We sped down to the cancer center and got our appointment with the oncologist. She’s a rock star.
These are people who’ve known my mom now for a little over two years. They know my dad. They’re the younger couple so people tend to recognize them and know them in the unit.
The look on their faces… The head oncologist and her team of nurse practitioners had this look. My doctor said, “I’m so sorry.” She genuinely was upset that we were in there.
She went through the whole thing and that’s when they said the staging. My dad never got a staging. They just treated him. My parents had asked a couple of times, but they never really clarified. We think maybe 2 or 3 and I could totally be wrong about that.
But for me, right away, it was, “Okay, well, you’re stage 4.” I said, “What?” I didn’t have any symptoms other than this cough, but my lung was completely infected and that was all the cause for it.


Immunotherapy & chemotherapy treatment
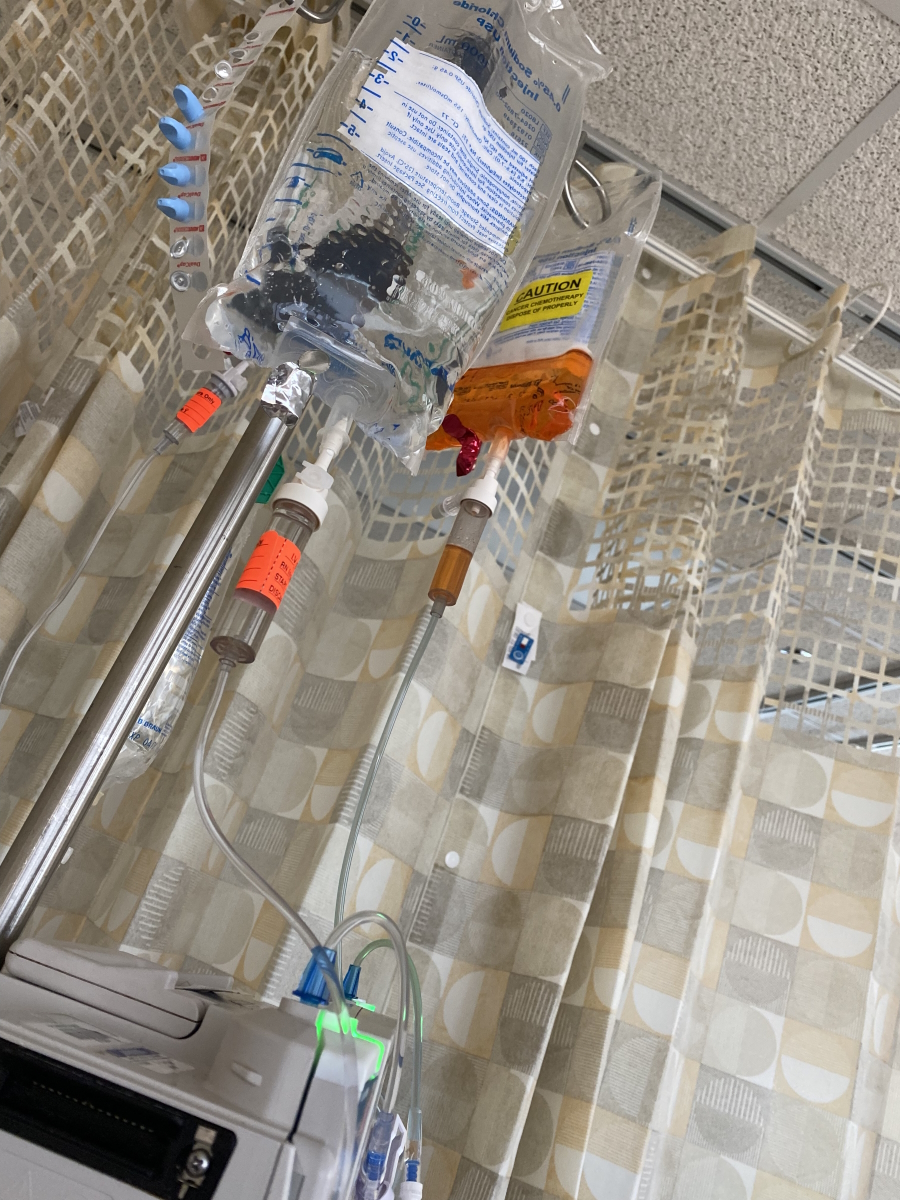
I did the egg retrieval on a Thursday. That Friday, I did my first round of immunotherapy and rolled right into chemo.
I first started the chemo treatments end of July. I did R-EPOCH.