Lynn’s Small Lymphocytic Lymphoma (SLL) Story
Lynn’s Small Lymphocytic Lymphoma (SLL) Story
When Lynn received his small lymphocytic lymphoma (SLL) diagnosis in 2013, he felt like he had lost his future.
Lynn saw a specialist at MD Anderson for treatment options. He is a strong proponent of seeing a specialist, especially after being a caregiver for his son when he was diagnosed with cancer in 1977.
A decade after diagnosis, Lynn reflects on his first symptoms, treatment and side effects and living life with a glass half-full mindset.
- Name: Lynn B.
- 1st Symptoms:
- Prolonged fever
- Night sweats
- Diagnosis:
- Small lymphocytic lymphoma (SLL)
- Non-Hodgkin’s lymphoma
- Tests for Diagnosis:
- X-ray
- Chest CT scan
- Bone marrow biopsy
- Treatment:
- Rituxan (rituximab) and Revlimid (lenalidomide) combination for 3 months
- Rituxan (rituximab) and Imbruvica (ibrutinib) combination – ongoing
- SLL 1st Symptoms and Diagnosis
- Introduction
- Symptoms and Tests
- The Diagnosis
- Receiving the diagnosis
- Processing the diagnosis
- Did you feel like you were losing things you had been looking forward to?
- Can you describe what you meant by feeling "marked"?
- Processing what it means to live with chronic cancer
- Can you explain the power of your doctor saying you could manage the cancer?
- Treatment and Side Effects
- Being a Caregiver and Lessons Learned
- More SLL & CLL Stories
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
SLL 1st Symptoms and Diagnosis
Introduction
Tell me about yourself
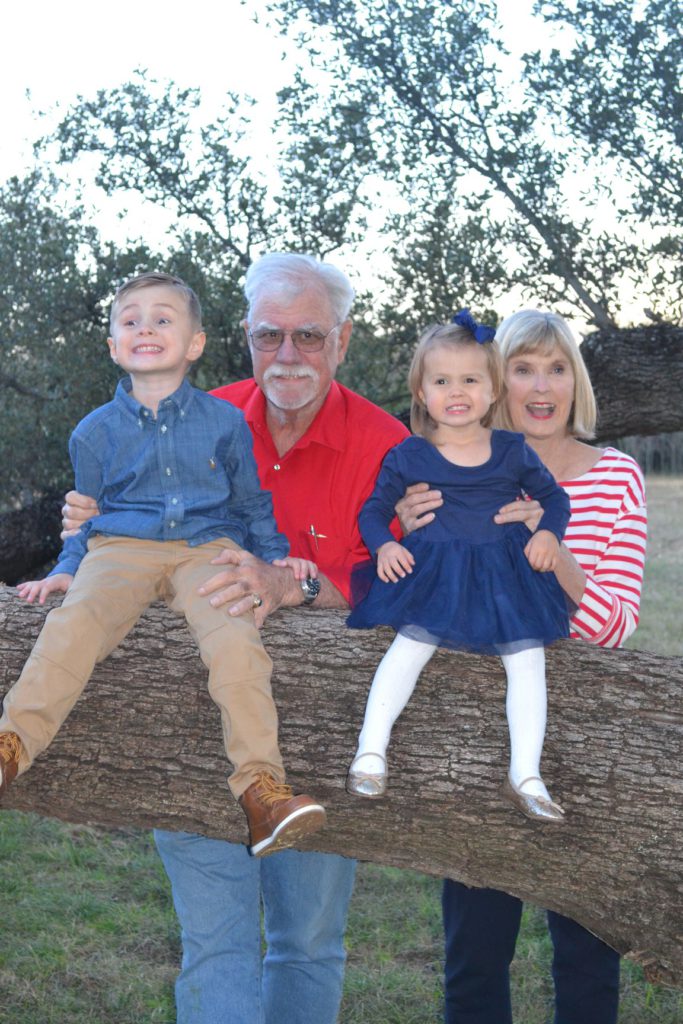
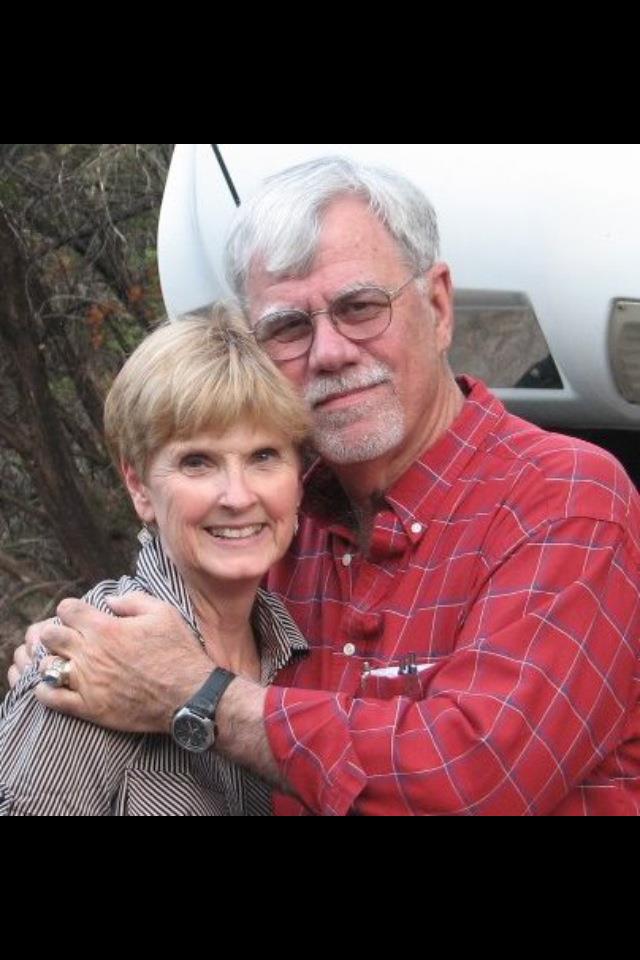
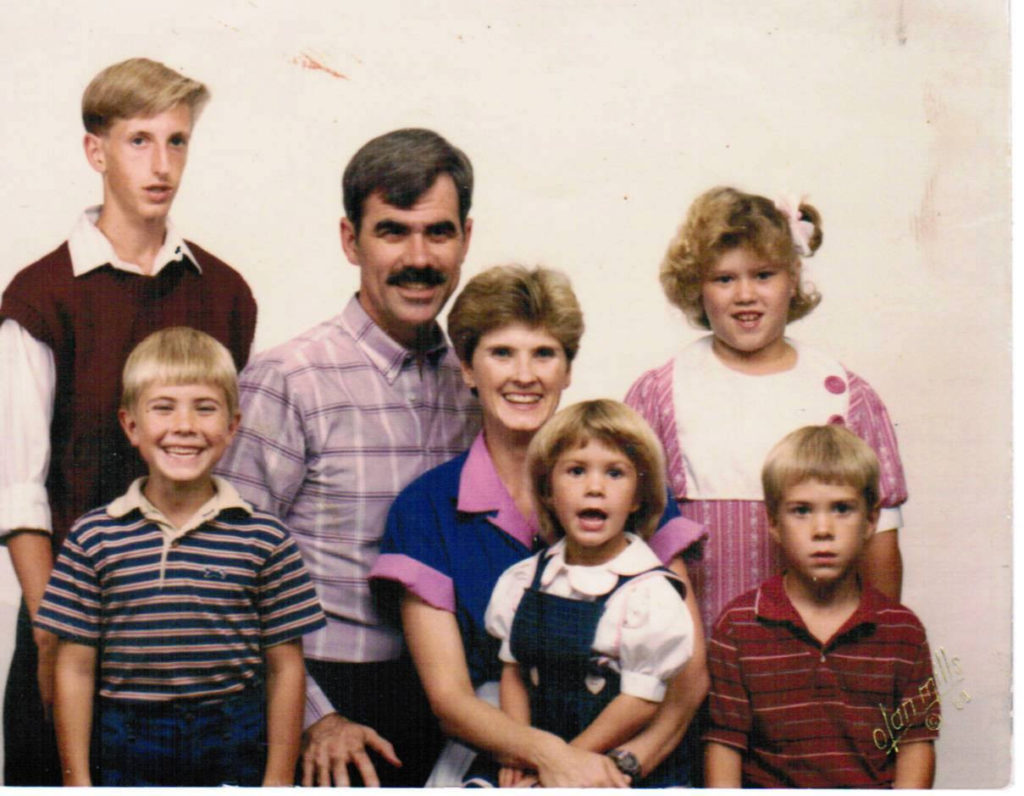
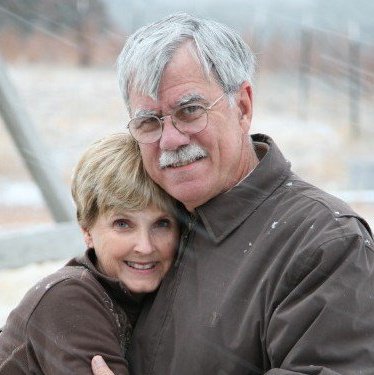
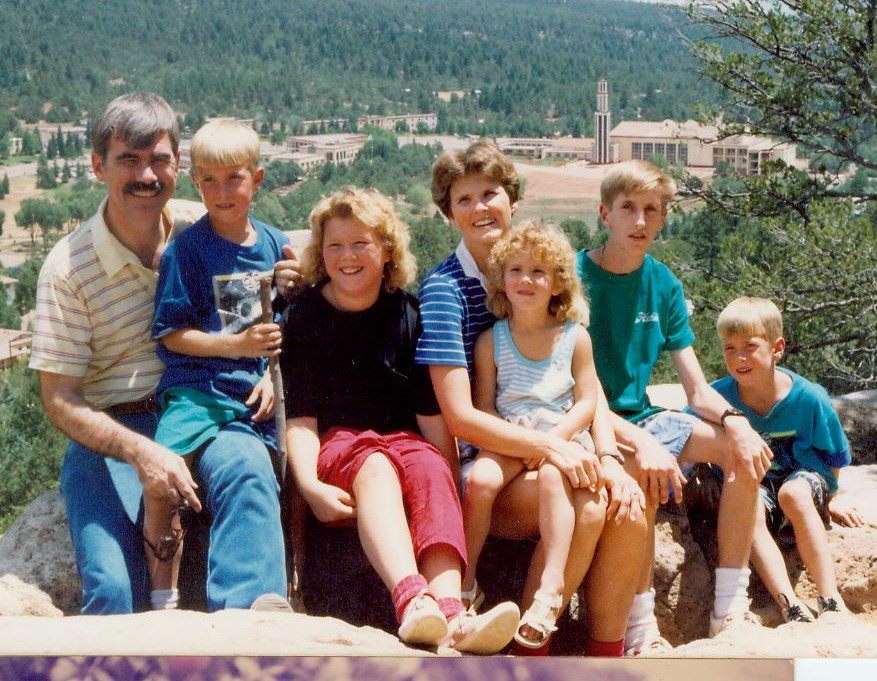
I’ve been married to my wife since 1970, so that makes 52 years. She’s a long-suffering lady, and we alternate being caregivers. I couldn’t have done it without her. We had five children and when you have children, you’re a hostage for the rest of your life. Every day she’s got to check on them!
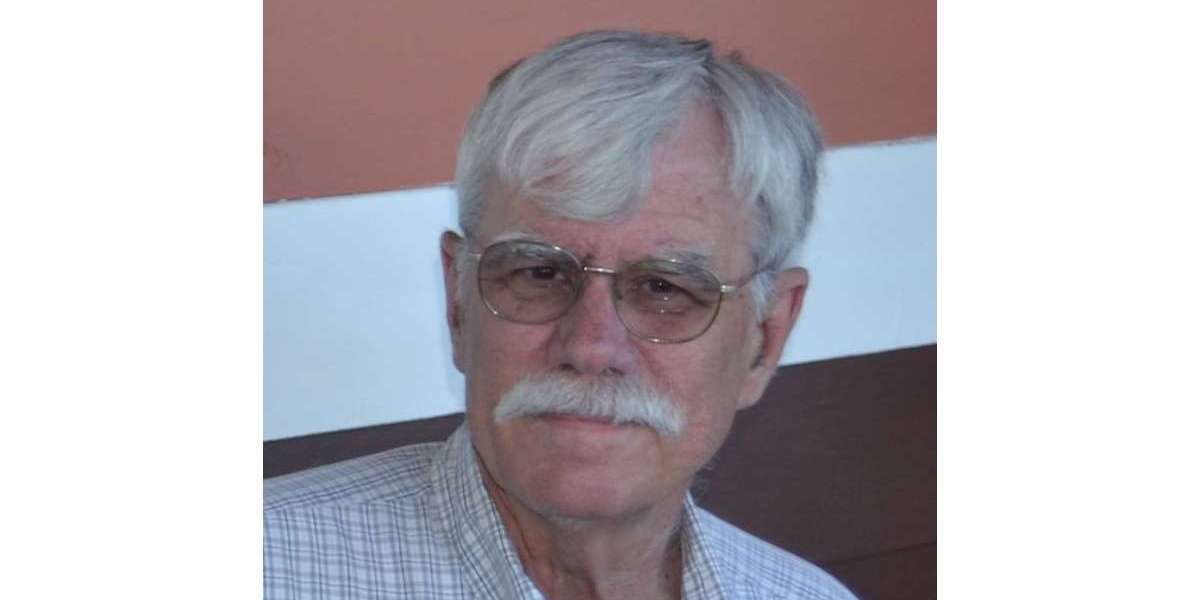
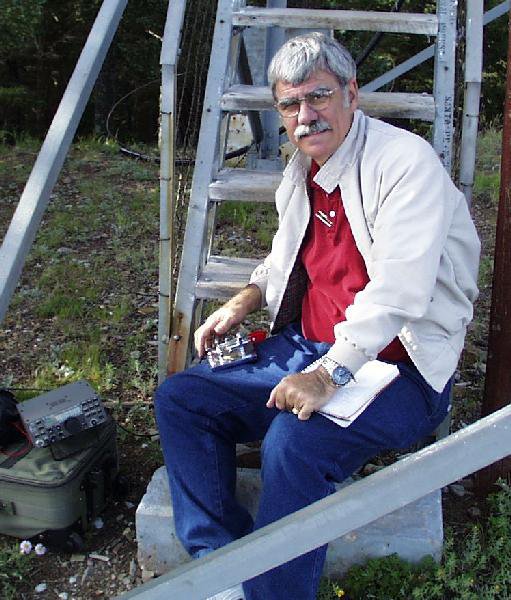
I worked for an electric utility for 40 years. My training was in electrical engineering at a school in South Texas, and that was growth out of my hobby, which was ham radio. This has been an interest of mine for all these years.
In some senses, I was bi-vocational because when I went to work for the electric company, I also was a youth minister, served in several churches, and then later on was a volunteer music minister directing choirs and leading music in a church.
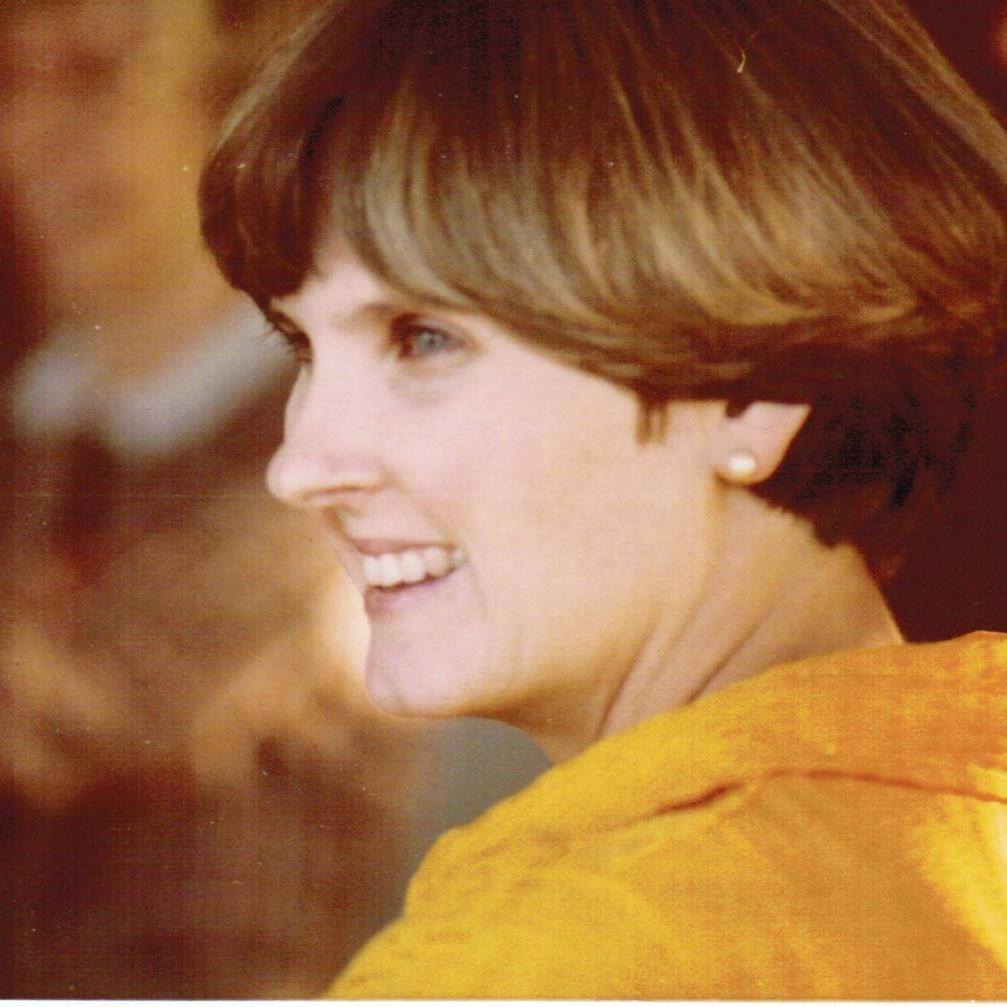
Music is one of my real loves, having grown up singing in choirs, playing a trombone in the band, and picking up the guitar. It should be no surprise that my wife, I love to hear her sing, and her voice has lasted much longer than mine has.
It all started with sitting by her as she waited to be picked up at high school. Of course, I had been trailing her for months, getting up the nerve. I was about to graduate, so I had to make my move. She left her [sheet] music there as we were sitting and visiting. When her dad drove up, she left the music, so I didn’t say a word. Of course, I knew where she lived. After her dad took her home, I followed about 20 minutes behind and handed her the music.
Ham radio
[One] morning I had insomnia about 2:00 a.m. I knew some guys were talking, and I went out into my ham shack and talked to them. First time I’d actually talked to them, but I told them I had been listening to them for 10 years.
I said, “When I was diagnosed with blood cancer, it meant a lot to me to be able to get some normalcy by listening to you guys in the middle of the night when I was lying awake worrying about my disease.”
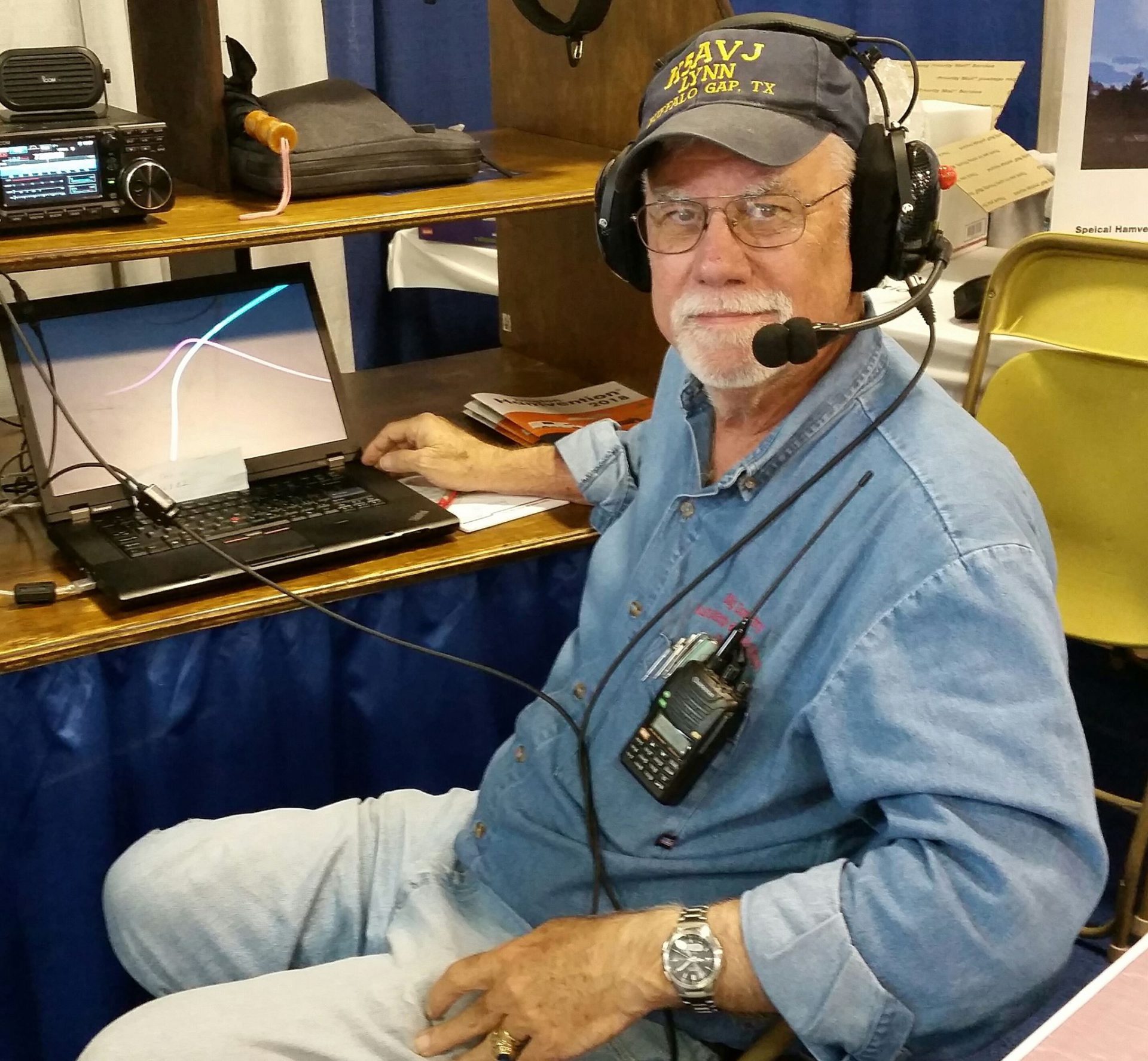

That meant a lot to me to bring some normalcy into my life. You just longed for that. Your life has changed for forever when you’re diagnosed with cancer. That was my chance to say thank you to those guys that morning.
They said, “Hey, everybody out there, this is Lynn’s first time. Say hi to him.” I was hearing voices and people giving their call signs from different locations. I certainly did feel welcome. I had witnessed their companionship, the type of camaraderie. Anyway, the friendship that they have, their camaraderie.
My wife has put up with it, like they do with hobbies, whether your hobby is radio or fishing or whatever. She’s put up with it. I appreciate that. It’s not all time consuming, but it varies.

Cancer’s impact on who you are
When you’re diagnosed with cancer or you go through a hard time in your life, it can put you in a very dark place. My normal personality is a very optimistic-type person, but I got into a real dark place. It was hard to come out of.
I’ve shared with you that in ’74, our son was diagnosed with cancer, and I lost 20 pounds just within just a short time. People react differently to depression, but I did the same thing when I was diagnosed with cancer.
One of the side effects of this cancer is weight loss, but I think it was as much for me as having that diagnosis hanging over me and not knowing what it meant. That it might mean I have 2 to 3 months left to live or maybe a year or 2 or 3, hoping to be a granddaddy, things like that. It’s a tough time to deal with.
Symptoms and Tests
What were your 1st symptoms in 2013?
I began to run a fever with no known cause, which was not a new thing, but it prolonged. It lasted day after day after day. It went on for a week, and so I said, “Okay, I don’t know what it is, but I want to go see my primary care physician.”
I was having some night sweats along with that, too. I was meticulously keeping the record of the daily temperature. I actually saw the nurse practitioner, but he had a lot of experience and he said, “Let’s just get a chest X-ray and see where we go from there.”
Then the call came from the doctor’s office after they got the chest X-ray. They said, “He also now wants you to go get a CAT scan.” The alarm bells went off then. I said, “What did they see on the X-ray? Something’s going on here.”
Anyway, I went and got the PET scan. Then I had the appointment the next week with him to see what he saw. He said, “It appears that you may have a type of lymphoma. We don’t know, but you need to go see an oncologist.” That’s how things evolved at that point.
Night sweats
I had some night sweats with that. I didn’t know what to think about that. Is this just part of the fever or what? I would find that it would get much worse in the coming months. I found that it would be to the degree where your night clothes were drenched and the sheet underneath you was drenched.
I would sometimes have to get up and change clothes, underclothes and then the spot in the bed would be too wet to lie back down on. Through all that, I didn’t want to wake my wife up. We are in a pretty dry climate out here in West Texas, so things would dry out pretty quickly.

Getting an X-ray, CT scan and bone marrow biopsy
X-rays don’t raise an alarm. You’re just kind of like, “Oh, yeah, I’ve had a lot of X-rays.” But when they said, “We want a chest CAT scan.” Well, I’ve never had a chest CAT scan. Something is going on. I try to compartmentalize that, try to put it off to the side, but it’s there. It’s just nagging and you know something’s not right.
All of a sudden, what life I had left, which I thought was maybe 15 years, shrunk down to maybe just months.
The next week, I went in to get the report from the primary care physician. He said, “I think you’ve got lymphoma.” I went home and told my wife, and she didn’t believe me because I’m always joking and pulling pranks on her and things like that. She didn’t believe me when I went and told her. I had to insist that it was true.
She really stepped up to bat, because I withdrew into my cave. She began to research and print things out off the Internet, and I didn’t want to read them. Of course, I had the upcoming appointment with the oncologist and then the bone marrow biopsy.
When I got there, she said, “We can do a biopsy of your lymph nodes, but they’re all internal, so it’s going to be a little more difficult to get to them. We need to do a bone marrow biopsy and we can assess from that what type of cancer this is.”
The Diagnosis
Receiving the diagnosis
Then when the report came back on that, she said, “This is small lymphocytic lymphoma (SLL), which is akin to chronic lymphocytic leukemia, except this is primarily in the lymph nodes and not detectable at this stage in your blood. What I would recommend is that you be treated with R-CHOP.”
We remember the acronyms from when our son had cancer. We remember the acronyms and that they had meanings, and we recognized some of the drugs that she mentioned that I would be treated with.
I went home with the feeling that my days were numbered. Of course, I’ve always known my days were numbered, but I said, “They’re very short.” I went home with the thought, “I got to go through this.”
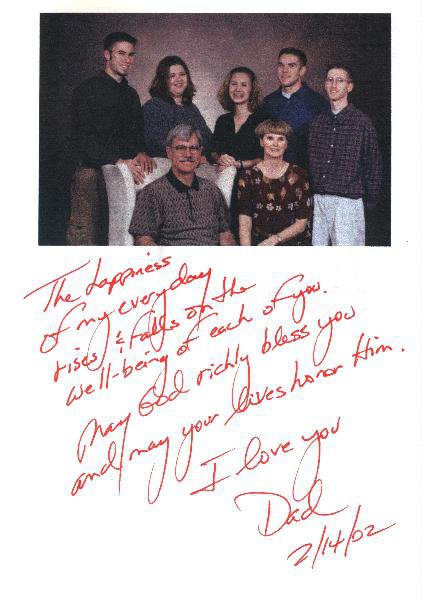
Within a day or so, my wife contacted the children, the grown adults, and told them what was going on. She came back and said, “The kids and I want you to go to MD Anderson.”
Processing the diagnosis
I crawled back into my cave and just accepted the fact that I was going to have to go through chemotherapy. My days were numbered. It was a dark place and just almost a resignation that this was the end.
My wife came, and still I had not read any literature. I had not looked on the Internet. I was scared of what I would see. My wife came, and she had printed some things out that I didn’t want to see. She said, “The kids want you to go to MD Anderson.”
With our history with our son having had cancer back in the ’70s, we were familiar with MD Anderson. We knew it was the right place to go. I knew it was the right place to go, but I just felt so lousy. It didn’t feel good, and I didn’t want to make the 400-mile trip.
She stepped up as the caregiver and called MD Anderson and made an appointment. She didn’t even get a referral. She just made an appointment and said, “I got you all lined up. We’re going to go down there, and we’re going to go there in a week-and-a-half.”

It’s one thing when somebody else gets a diagnosis, but when you personally get the diagnosis, in my life the future just disappeared. Even at that age of 66, the dreams I had of being a granddad and what was to come and things to enjoy since I was newly retired — those all vanished.
All of a sudden, what life I had left, which I thought was maybe 15 years, shrunk down to maybe just months. I didn’t know. I certainly knew I didn’t feel good, and something was wrong. The doctors were right. I did not feel well.
»MORE: Patients share how they processed a cancer diagnosis
Did you feel like you were losing things you had been looking forward to?
Yeah. We had retired where I was working in West Texas, out in the country on 6 acres. There was an extensive area to mow, but there were things we were involved in.
We were involved with our church, and we were joining with an acoustic group of musicians singing at the rest home. I was enjoying getting to take my guitar, and there were dulcimers, violins, other banjos and other kinds of instruments.
He said that we can’t cure this disease, but we can manage it. All of a sudden, the glass for me was half full again.
All of a sudden you’re sick, and you need to stay away from people. When I saw people, I was not one who held it back or didn’t share my diagnosis. I shared that with other people. All of a sudden, it’s like you’re marked, and I felt marked.
I felt like, “I’m here, and I just want to tell you that I’ve got this diagnosis of small lymphocytic lymphoma.” Of course, nobody knew what that was. It is a rare disease, just like its counterpart CLL. They’re rare diseases.

Can you describe what you meant by feeling “marked”?
We’ve all been through that in our life where somebody we knew was diagnosed with a terminal disease. You have different reactions. When you hear that, you don’t know how to respond to that person or to their family. Sometimes you’re asking their family members, “How are they doing?” because you’re uncomfortable asking that person how they’re doing.
We’ve seen through life experiences that some people withdraw from you. Some people that have been friends don’t know how to cope with it, so they pull back. I was pulling back, too. It was a difficult time.
Processing what it means to live with chronic cancer
I finally saw the specialist at MD Anderson, and the phrase that he said to me brought hope back in my life. He said that we can’t cure this disease, but we can manage it. All of a sudden, the glass for me was half full again. It was not half empty. I found that to bring hope to my life.
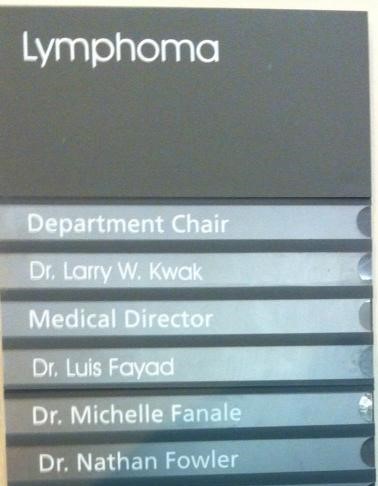
On that trip we made to MD Anderson, I decided to start looking for things that were humorous again and find things to laugh about. As I stood there in the medical clinic at MD Anderson and I looked at the list of doctors, I began to laugh. One of the doctor’s names was Dr. Fanale. He was not my doctor, but that was one of the doctors.
The doctor at the top of the list, the one in charge, was Dr. Kwak. I had to take a picture of that and post it on my Facebook page to let folks know that I was finding things to laugh about again.
We stopped and ate at a restaurant. Of course, camo or camouflage-type dress is common in Texas, and I looked over there and saw these folks with camouflage. It made me think of the TV show about the guys in Louisiana that sell the duck calls. I thought about them. Things like that were bringing humor back to my life.
Can you explain the power of your doctor saying you could manage the cancer?
I think I was thinking he was going to say, “We can just buy you some time.” But he turned it in a positive way to say that we can manage it.
I did not have any comprehension of the research that was going on that was going to begin to explode in the treatment of CLL and SLL, which certainly has exploded in the last 10 years. It would bring so much hope for people that are diagnosed with those diseases.



To that point, the treatment was going to be chemotherapy. But as we sat down and talked — the doctor and I did, and my wife and son were with me — he said, “Let me just talk to you about some of the treatment options. We’ve got the traditional chemotherapy that we can treat you with, or we can treat you with some novel therapies, targeted therapies.”
We began to see that there were some other options. We were up into the time frame of November, and he was ready to start treatment because I had 70% involvement in my bone marrow, and my blood counts were beginning to drop. The B symptoms, as they say, would be getting worse: losing weight, the fevers and the night sweats.
Treatment and Side Effects
Deciding to Start Treatment
Testing for treatment options
He gave the option to start treatment in December, and I said, “You said that this is a disease that we don’t have to treat right away? We can defer. How about if we start in January? I would like to enjoy Christmas.” That’s the way that took place. We went back to MD Anderson. At this point, we were going to MD Anderson every month.
Now I digress a little bit, but you go from where you’re comfortable, the doctors you’re comfortable with. Here you go to the big city, and you go to the parking garages, and you go to the freeways. All that, to me, was like a maze. As we age, we’re not as capable of negotiating those kind of traffic jams and problems you have.

It’s like a great sigh of relief came when you get the car parked and stop and take a picture of the parking lot number so that you remember where your car is when you get ready to come back to your car.
We were having CAT scans, and I had PET scans, bone marrow biopsies and blood work. I’m sure at some point in there I had an X-ray, and then at some point in there I’m sure I had an EKG. They wanted to be sure that the kind of drugs they were giving me would not interfere with that.
Discussing treatment options
There we were, going to start in January, and we discussed the options. It was chemotherapy or a novel therapy. The doctor said, “We’ve got 2 drugs that have had some benefit for this type of cancer. One of them is Revlimid. The other name for that is lenalidomide. It’s a common treatment for multiple myeloma. The other drug is Rituxan.”
Of course, those didn’t mean much to me. Some folks have a long watch and wait. During that time, they can research and see what the different drugs are and how they interact and so forth.

A pill a day keeps the cancer away.
I was so naive that the Rituxan went in on an IV, so I thought that meant I was actually getting chemo. I didn’t understand that it was a monoclonal antibody, and it was not chemo. I got Rituxan and Revlimid. I was getting the Rituxan IV every week, so we stayed there locally.
We were going back every week to get another infusion, and this stretched out for about a month. Then after that, we were coming monthly for the IV and to get a refill on my pills, which were the Revlimid.

Changing treatment
At the 3-month mark from the time we started, the doctor said it’s time to do a CAT scan and see if this is working. The results came back, and we sat down with him. That was in April of 2014, and he said, “Okay, what we’re seeing is no difference.”
I said, “Well, that’s good, isn’t it? I mean, they haven’t grown.” Here I am, the guy with a glass half full of water.
He said, “No, no, that means we need to try something else.” He said, “There’s a new drug that was just approved by the FDA, but it’s approved for second-line therapy.” I had failed Revlimid and Rituxan, so I was ready for second-line therapy.
We began with again repeating the Rituxan every week (and then stretching it to every month) and taking the ibrutinib every day. That’s how that all started in April of 2014.
»MORE: Read more about ibrutinib and other patient experiences
Over 8 years later, are you still on ibrutinib?
That’s right. I’m still taking my daily pill. As I say, a pill a day keeps the cancer away. In some ways, to me, it’s not too much different than the person who’s a diabetic and has to get insulin every day or some other type of chronic disease.
I choose to look at it in a positive way. I know that this may not work forever. I know it’s got some side effects, and we don’t know for sure what the long-term side effects are.
God bless those folks that were in clinical trials, because those pioneers that took this — some of them it worked for them, and for some of them it didn’t. For some of them it’s still working, and they’re at 10 years on this drug. They continue to bring me hope that this will continue to work for me.
In the meantime, I’m on the very first of the BTK inhibitors (ibrutinib), but since then, there have been several other ones that have been developed. There are second generation and third generation ones that have fewer side effects and are easier for people to take. It brings hope for other people.
Besides that, there are other types of treatment that are targeted or novel that are not chemo. They know now that chemo’s probably not the best treatment. Before ibrutinib, the standard of treatment was FCR. That still is the standard and probably is in some other countries. Fortunately, in the U.S., we’re able to move on to other options.