Pete DeNardis’s Waldenström Macroglobulinemia Story
Pete D., Waldenstrom Macroglobulinemia
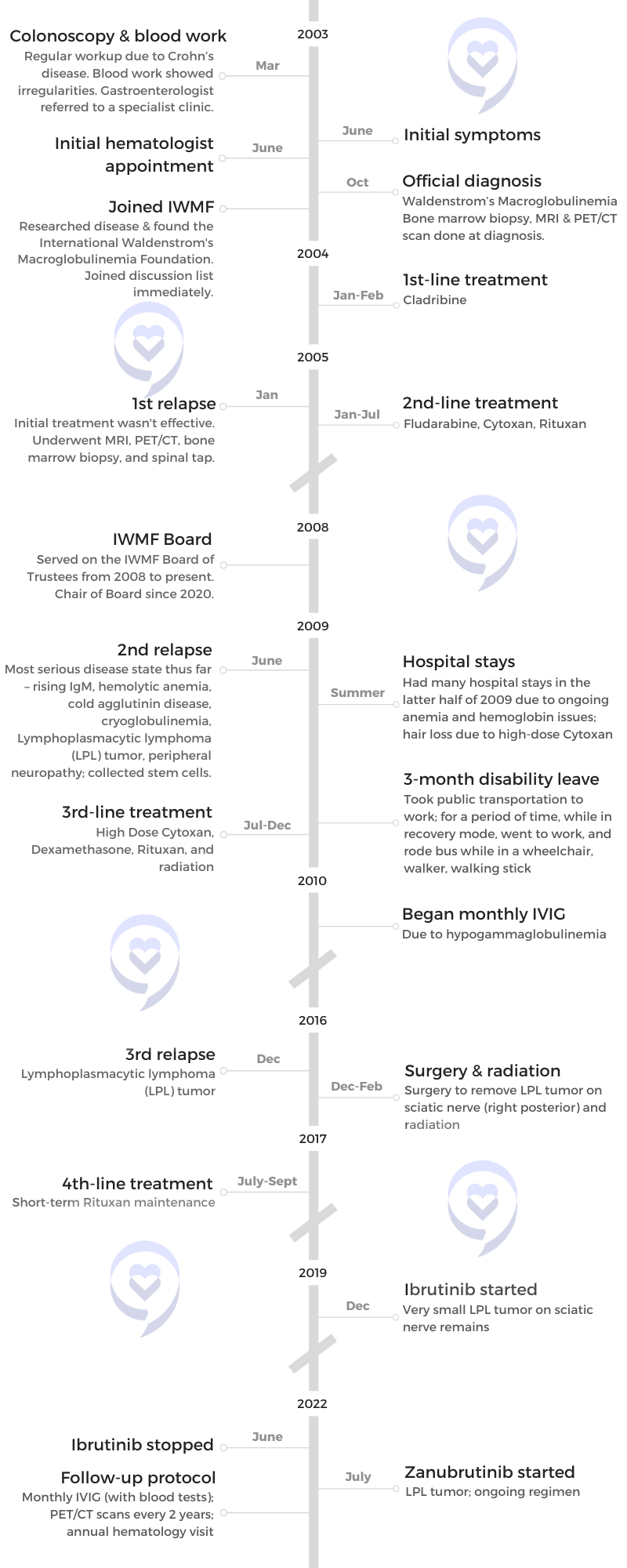
Symptom: Irregular blood test results during a regular workup for Crohn’s
Treatments: Chemotherapy, surgery, radiation, monthly IVIG
Pete DeNardis’s Waldenström Macroglobulinemia Story
Pete DeNardis was diagnosed with Waldenström macroglobulinemia (WM) at 43. It is a type of non-Hodgkin lymphoma and is a rare cancer that begins in the white blood cells.
He shares the importance of educating yourself about your disease, communicating with your disease community, getting a good support system, improving your quality of life, and being your own advocate.
- Name: Pete DeNardis
- Diagnosis:
- Waldenström macroglobulinemia
- Initial Symptom:
- Irregular blood test results during a regular workup for Crohn’s
- 1st-line Treatment:
- Cladribine
- 2nd-line Treatment:
- Fludarabine
- Cytoxan
- Rituxan
- 3rd-line Treatment:
- High-dose Cytoxan
- Dexamethasone
- Rituxan
- Radiation
- 4th-line Treatment:
- Rituxan (short-term maintenance)
- Ongoing Treatment:
- Ibrutinib (December 2019 to June 2022)
- Zanubrutinib (started July 2022)
- Monthly IVIG
If you see one Waldenström patient, you’ve seen one Waldenström patient because we’re all different. We have the same disease, but our bodies behave differently.

This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
Pre-diagnosis
Tell us about yourself
I live in the United States, in Pittsburgh, but I was born in Italy, came over when I was six months old, and got my citizenship when I was six years old. I had your basic American upbringing [and] had a little bit of Italian spoken in the household. I was bilingual initially and still retain some of that.
I’ve been working as an accountant for a long time. I gravitated towards working in financial systems because I also like playing with computers so I’m sort of a financial systems analyst, a hybrid of sorts.
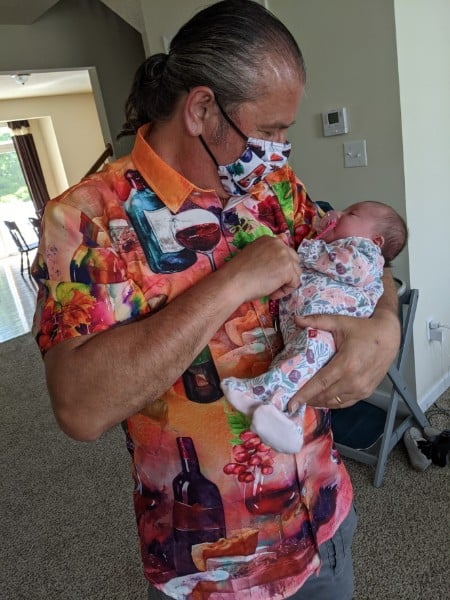
I have a family and three kids. Two of them are married and two grandchildren came in the past year and a half.


Initial symptoms
At that time, I had just started a new job. I decided to change careers. A lot of people do that after they get cancer; I did it before and I decided I wanted to teach full-time. I was teaching part-time for a while and I got an opportunity to teach at Penn State’s Beaver Campus.
I was setting up classes and working during the summer. I was in this little office, like a closet. I started to feel tired. I thought, I’m just working too hard, trying to try to learn how to do all of this, and also prepare materials for classes.
Then I started having severe nosebleeds, but I thought, I just have a cold or something. They were pretty serious nosebleeds. It was very difficult to stop them, but for whatever reason, I was on that work train and wouldn’t stop.
[My gastroenterologist] called and said, ‘Did you ever call that number that I gave you?’ I said, ‘No, I got busy, I forgot.’ But he said, ‘It’s really important that you call that number right away.’
It was so bad that I would end up with blood going down my shirt from the nosebleed. I would wipe it up or try to hide it at least and then get the heck out of there. But it happened fairly frequently so then I thought, something’s going on, but I’m too busy. Every once in a while, it would stop so I didn’t think anything of it. It’s a pretty good flow coming out of your nose, which is not normal even for someone who normally gets nosebleeds.
I also had a colonoscopy because I have Crohn’s disease so I do that every couple of years. Part of that is the blood test workup. At around the same time, my gastroenterologist called and said, ‘I saw some funny numbers.’ He might have said elevated protein, but it didn’t mean anything to me at the time because I didn’t pay attention to that stuff and I ignored it.
Three months later, he called and said, “Did you ever call that number that I gave you?” I said, “No, I got busy, I forgot.” But he said, “It’s really important that you call that number right away.” He didn’t say anything else.


Initial hematology appointment
I called the number and the receptionist said such and such hematology clinic. Right there I thought, “Oh, something’s up here. I don’t know, but this doesn’t sound good.” We made an appointment. My wife and I went and we did blood work.
We got to meet with a hematologist and he said, “Based on your blood work, it appears you have some type of lymphoma. I’m not sure what it is. We can do the bone marrow biopsy right now if you want, or you can schedule it.” I said schedule, but my wife, being my very important caregiver, said, “No, we’re doing it right away. I don’t want you putting it off.” We did that right there.
Bone marrow biopsy
It was an interesting experience, to say the least. They did numb the area, but I was not sedated — a bit uncomfortable, put it that way.
‘It appears to be a rare form of cancer that’s not curable. You should really think about getting your affairs in order.’
Diagnosis
It takes a couple of weeks to get the results. We went back to see him and he basically said, “I’m not certain, but it appears to be a rare form of cancer that’s not curable. You should really think about getting your affairs in order.”
Getting a second opinion
We were in shock, but we sat back and said, “Okay, I’ve already had one chronic illness. Let’s add another one to it. Let’s move on. There’s got to be something we can do.” We said, “Okay, I appreciate your opinion, but can I get a second opinion? Because I can’t believe that I can’t do anything about it and I’m going to die in six years.” He did say, “Well, that’s your prerogative and that’s your opinion. I’ll be glad to give you the name of someone else who’ll probably be more than willing to treat you right away.”
I thought, well, that’s an odd attitude to take, so I’m glad that I’m getting [a] second opinion. The doctor that he sent me to was actually a pretty good doctor. Right away, I had a good relationship with him and that’s when I started treatment, right away at that point.

‘I appreciate your opinion, but can I get a second opinion? Because I can’t believe that I can’t do anything about it and I’m going to die in six years.’

Deciding to get a second opinion
It’s important, especially when you have a rare form of cancer, to seek out those centers of excellence if you can. If you can’t afford that or can’t travel to it, go to a larger research university-based hospital. Fortunately, I live close to one in Pittsburgh. We have the University of Pittsburgh. We have a lot of research going on there. I was able to go to both hospital systems that I can go to. They both have noted researchers there so that makes a big difference.
If you go to a community hospital — I’m not denigrating the hematologists or the cancer doctors there — but they may not even see a person with my disease in their whole career. It’s important to get in touch with a doctor that has experience with your disease or can consult with other doctors in their practice that do have patients with your disease.
It’s important, especially when you have a rare form of cancer, to seek out those centers of excellence.
That first doctor had that attitude and maybe he was right, but that attitude of I know what I’m talking about so don’t question me. Even his staff, when I would call and say, “Hey, why is he requiring this test?” Or “Why does he want me to do this?” They would say, “Well, why would you question that?’ And wouldn’t even answer the question. I knew right then that definitely I’m not going to this place again.
The second doctor was much more open. He sat down with you. He drew charts. He explained. He said, “Okay, you have Waldenström macroglobulinemia and we’re going to treat it. This is how we’re going to treat it. This is standard treatment at this point in time and just because you see a lot of statistics out there, that’s an average. That’s just the median. Some people live shorter, some people live a lot longer. And given that you’re diagnosed at an earlier age, there’s a good chance you’re going to live for a lot longer than those six years that they’ve been quoting to you. Plus, I have the ability to consult with a lot of other researchers and hematologists in our practice and in our hospital system. We’ll discuss your case and we’ll treat you accordingly.”

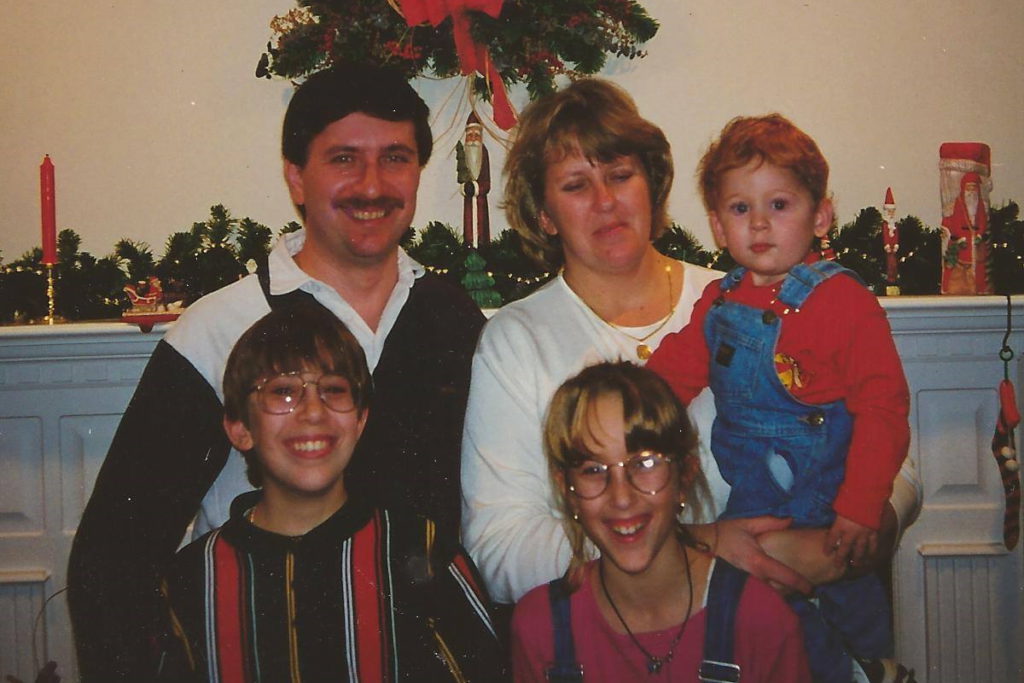
What really hit home was wow, I won’t get to see them graduate. I won’t get to see them get married. I won’t get to see any of the special moments in their lives.

Processing the diagnosis
[My wife and I], we do everything together so right off the bat, my first concern was for her. What’s she going to do if I’m not around?
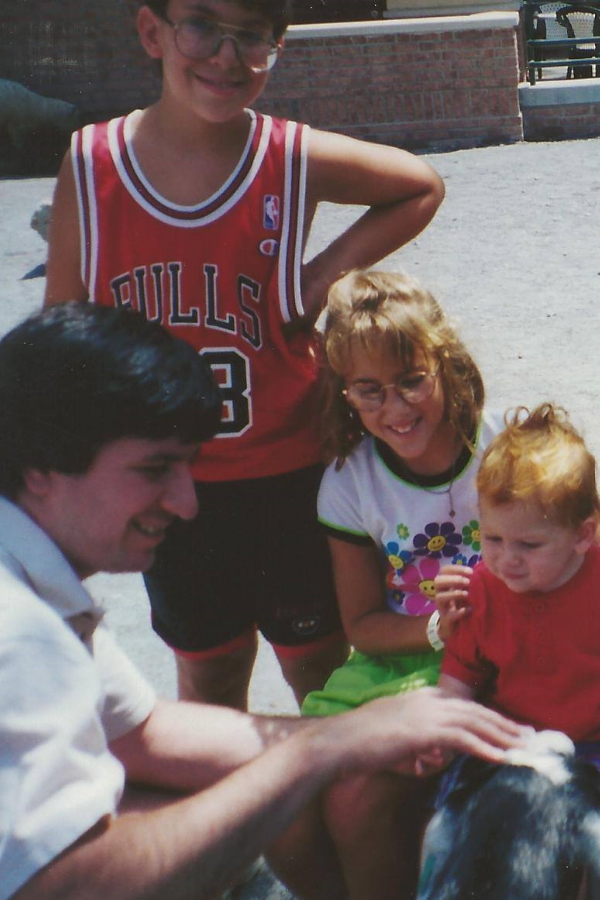
Then the thoughts automatically go to my children. I’m not going to be around. They’re in grade school and high school. They were seven, 14, and 16 at the time. What really hit home was I won’t get to see them graduate. I won’t get to see them get married. I won’t get to see any of the special moments in their lives. They won’t have me around. That was [what] hit me the hardest, not being there for my family.
You can’t bottle that up. You bottle that up, that gets even worse. There was a lot of crying, hand-holding, and just worrying about all of that. I think that’s normal and that’s healthy to let it out rather than bottle it up. I’m not saying you have to cry every hour of the day but that’s important to let that out.
We laid it out to them straight and said, ‘Look, dad has cancer,’ and try to tell them in as simple a way as possible.
Breaking the news to the children
Once we found out exactly what I had, did a little research on the disease, and then found that it wasn’t an immediate death sentence — because I was diagnosed at 43, which is unusually early for this disease — we decided that because I had to go into treatment right away and I could be pretty weak from the treatment — could have some odd side effects — we felt it was important to let the kids know if I’m not going to be around to take them to soccer practice or any of their school events, they should know why.
We laid it out to them straight and said, “Look, dad has cancer” and try to tell them in as simple a way as possible, that it’s serious but it’s treatable and we just have to go with the flow and I’ll be around for a long time. I’m not going anywhere.
I always told my wife that she can’t get rid of me that easily. We’re honest and upfront, but we’re willing to answer any questions they had. The older ones were fairly intelligent to figure out how to find information, but we did try to answer their questions and were upfront with them. That worked for us.



We’re honest and upfront, but we’re willing to answer any questions they had.

Importance of doctor-patient relationship
What I liked about the second doctor I went to was, right away, I felt a connection with him that I didn’t have with the first doctor. Sometimes it’s a personality thing. It’s their demeanor; you click. It’s odd that that’s an important aspect of it, the human element of that, not just the scientific.
I’ve talked to other Waldenström patients and some, they’ll say, “You go to that doctor? Oh, I can’t stand that doctor.” Because they don’t connect, their personalities don’t work, they want something different — and that’s normal. That’s part of it also.
The important thing is to become educated. When that doctor said, ‘Okay, here’s the treatment plan we’re going to do. It’s fairly standard. We’re going to try this first.’ It was Cladribine and I did a little research on it.
Even then, I went searching on the Internet and found the International Waldenström’s Macroglobulinemia Foundation, hooked up with their online discussion list, and automatically started asking fellow patients. “What do you think of this? Will it work?” Basically, the response I got was there may be better options but as a first-time treatment, at that point in time, it was the least toxic so give it a shot [and] see if it works. It may or may not. And so we went with that.
Initial treatment
I [started treatment] right off the bat in 2003 with Cladribine.
First relapse
Expectation setting
With Cladribine, the thinking was I should get two to five years of response. They don’t like to use the word remission if you’re in a recurring kind of cancer. That was the expectation and unfortunately, I didn’t even get that.
[I was getting] monthly blood tests at that time. We saw the numbers — their marker, which is immunoglobulin — the IgM marker dipped down a little bit but started rising right back up again. We knew it wasn’t working.


Dealing with scanxiety
Back then, you didn’t get your blood results immediately. You had to wait a few days and so that was nerve-wracking because you don’t know what to expect from the results. [There] was always that fear that, Oh, here we go. We’re going to have to go back to treatment again. You dread it but also look forward to it because maybe it’ll be a good result.
It’s better now because you find out almost right away what your blood work results are. I’m in a different position now. I know my body better so I know when things are going well and when they aren’t.
Second-line treatment
The next round was Fludarabine-Cytoxan-Rituxan. At that time in 2005, it was being used but there were rumblings in the research community that you might not want to do that.
FCR was found to be effective. I knew it would be more toxic in terms of side effects so they put me on antivirals and all the other stuff to minimize the side effects.
Every treatment has some side effects so it basically comes down to ‘pick your poison.’
Getting information on new treatment
At that time, Rituxan was fairly new. I questioned the doctor and our patient community [about] what they knew about it, how well it worked, and whether it was dangerous long term. In hindsight, that was a dumb question to ask but who knew back then?
Always go through that process of looking at what’s out there. I’m able to access some medical journals because I work at a university so I follow what’s happening in my disease and related diseases. I’m always looking at the research results of newer novel agents in related diseases — like CLL, WM, multiple myeloma, or other diseases — just to keep track of what’s up and coming and see what are the side effects.
With any novel agent — like for Waldenstrom’s, the newer ones are the BTK inhibitors and so I read up on the side effects of BTK inhibitors. Now granted, when it first comes out, you don’t have a long period of time to figure out the long-term effect.
A couple of the noted experts would always tell me, at least right now, there is no safe treatment. They said, in fact, the best treatment is no treatment at all if you don’t need treatment. But every treatment has some side effects so it basically comes down to “pick your poison.” The idea is what gives me the best potential for a longer period of quietness and minimal side effects.

I like to chart my own blood values so I would be able to see month to month how it was trending. It was exciting to see it actually going in the right direction.

It’s a balancing act, the kind of side effects you could experience. [With] BTK inhibitors, you could get elevated heart rhythm, high blood pressure, [and] elevated glucose levels. You have to deal with all of that. The flip side is your disease goes into a very quiet state for a potentially long period of time, but also, you have to take it every day for the rest of your life.
It’s also very expensive, which is another thing now that we have to consider. Very frustrating, at least in the United States, the fact that financial toxicity is becoming such a big issue.
Responding to the treatment
Right from the start, I like to chart my own blood values so I would be able to see month to month how it was trending. It was exciting to see it actually going in the right direction. I can’t say I didn’t think about it, but I could start focusing more on other things.
I actually enrolled in grad school and thought I’d work on a Ph.D. I did coursework in that and I thought, This is good. Every so often, I’ll get treatment. It’s not that bad and then [I] didn’t need another treatment and I’ll be okay. I went into a sense of security… maybe a false sense of security. But knowing that I was doing better [and] I felt better made a big difference compared to where I was before I started getting treated. That was the way I was looking at it.
Very frustrating, at least in the United States, the fact that financial toxicity is becoming such a big issue.
Second relapse
Symptoms
I did notice that I was starting to get a little bit more tired, a little bit more fatigued. I was watching the chart and would show it to the doctor. He would kind of smirk a little bit but then he would look at it. He would say, “Yeah, you’re right, it is going up but it’s not too bad yet and you don’t seem to have severe symptoms so go enjoy yourself. Have a good time.”
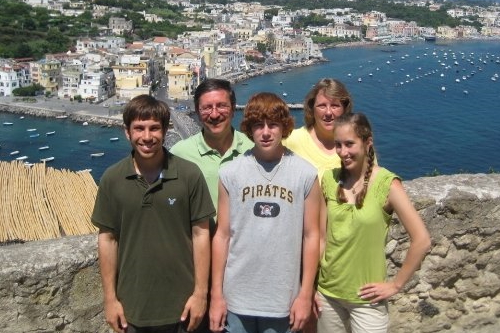
As much as I do, he knew the quality of life was important. He said, “Go, and then when you come back, we’ll talk about your options.” We did a month-long vacation to be with relatives and do all the tourist stuff in Italy and had a great time.
Towards the end, I was sleeping longer and started to get a cough that wouldn’t go away. I got some medicine there from a local doctor. It was some kind of injection of an antibiotic that they told me when I came back here was pretty strong stuff. I still was very tired and fatigued. I knew something was wrong. The trip back was not fun.

Complications
That relapse was pretty serious for me. I had a lot of things going wrong. It’s [already] unusual that I have a rare disease at a young age compared to other people but on top of that, I had other complications that go with that disease.
I had hemolytic anemia. Basically, my red blood cells would just be chewed away and I couldn’t replace them unless I got a transfusion so I became transfusion dependent. I don’t know how many blood transfusions I had. Maybe 16 of them over a period of three or four months.
I had cold agglutinin disease and cryoglobulinemia, which means, to add insult to injury, they had to warm the blood up in order for me to get the transfusion so that it wouldn’t clot. It was an interesting experience because they hadn’t used the blood warming machine in years so the nurses were kind of saying, “How does this work? Do you know?”