Brittany’s Stage 4B Metastatic Squamous Cell Cervical Cancer Story
Brittany W., Squamous Cell Cervical Cancer, Stage 4B
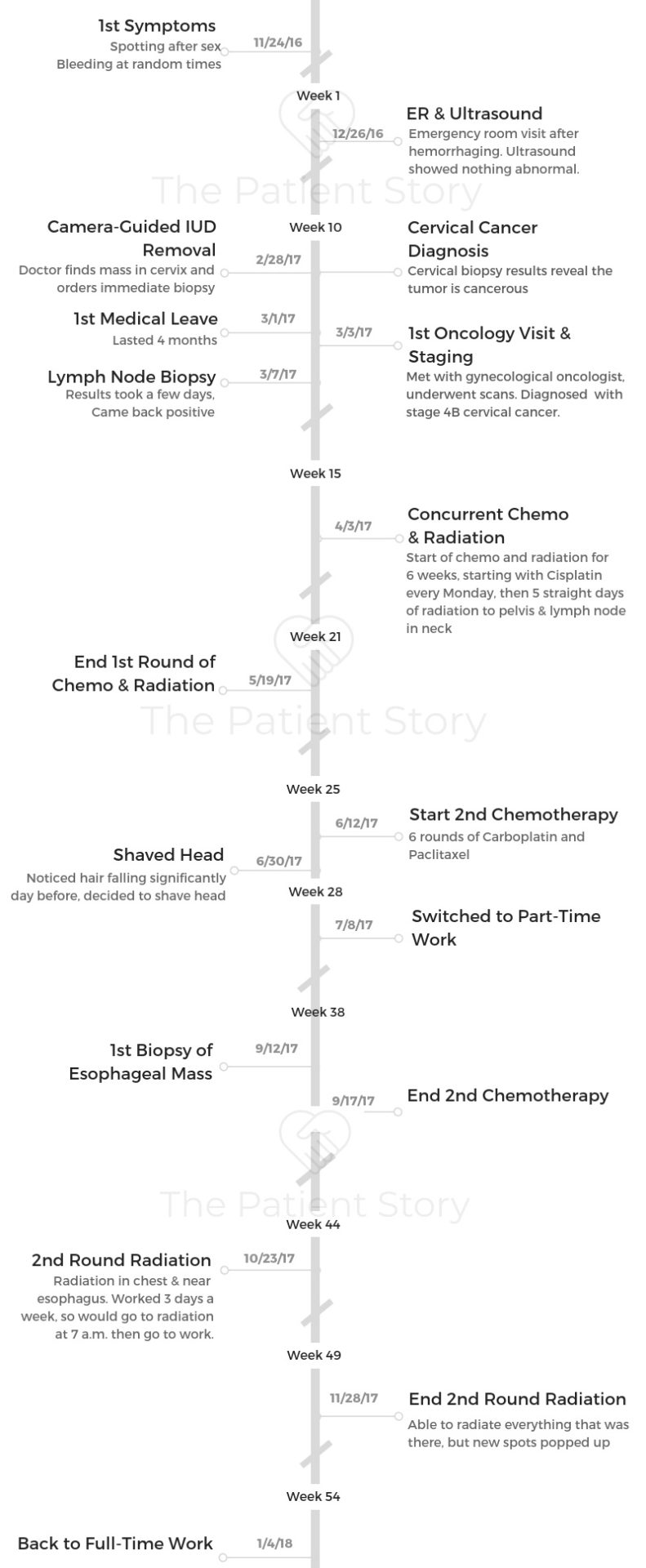
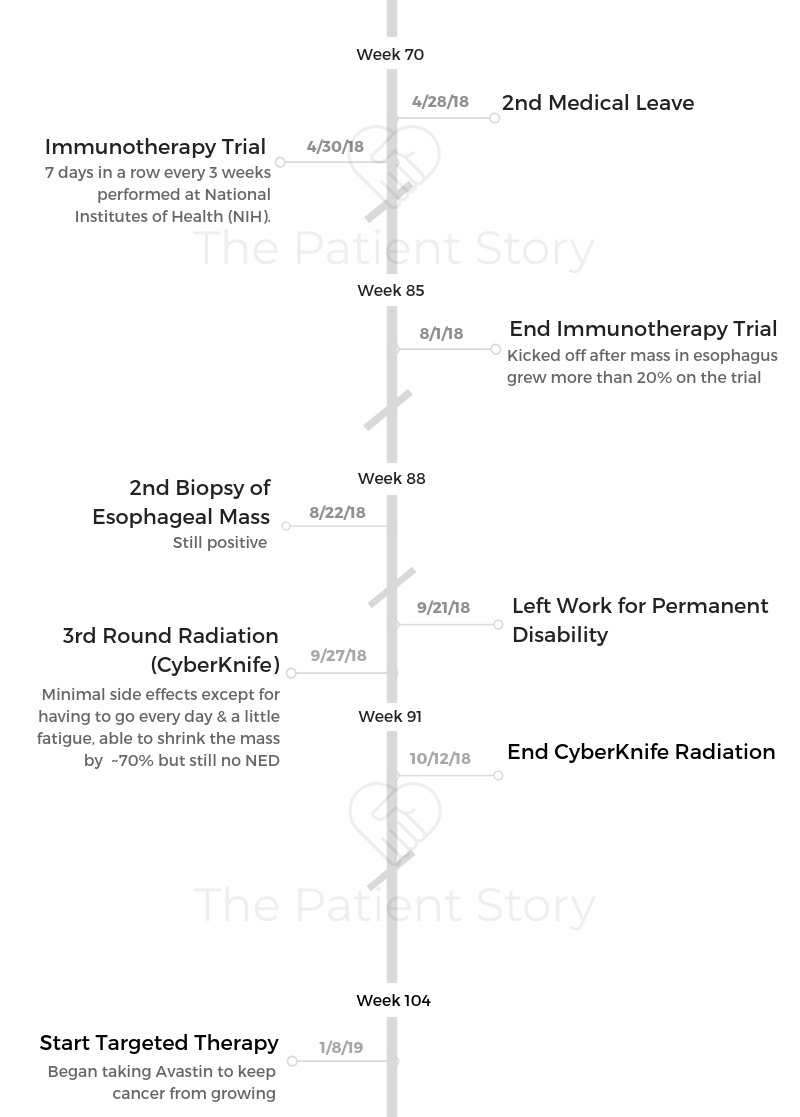
Symptoms: Spotting after sex, eventual significant bleeding at random
Treatment: Chemotherapy (cisplatin) concurrent with radiation, 6 rounds adjuvant chemo, 2nd round radiation, immunotherapy trial, targeted therapy
Brittany’s Stage 4B Squamous Cell Metastatic Cervical Cancer Story
Brittany shares her stage 4B metastatic cervical cancer story, diagnosed at just 30 years old. She detailed her first round of chemotherapy and radiation, second round of chemo and radiation, undergoing immunotherapy, and targeted therapy.
In her in-depth story, Brittany also highlights the issues that were most important to her to navigate: losing her hair, dealing with no real standard of care, how to be a self-advocate, and the impact on her marriage.

You’re doing great. Keep it up. I just look back at all of the doubt that I had every step of the way. I think every day that you live with cancer, you’re a cancer survivor.
Every time you wake up and decide to have a good day and get through what you need to get through, you’re doing amazing.
Brittany W.
- Name: Brittany W.
- Diagnosis:
- Cervical cancer
- Squamous cell carcinoma
- Stage 4B
- Age at Diagnosis: 30
- 1st Symptoms:
- Spotting after sex
- More spontaneous bleeding
- How Diagnosis Happened:
- Hemorrhaging led to emergency room stay
- Ultrasound didn’t detect anything at first
- Brittany pushed to have IUD removed
- During camera-guided removal surgery, doctor spotted massive tumor
- Biopsy revealed cancer
- Tests and Scans Pre-Treatment:
- Ultrasound
- Biopsy of pelvic mass
- PET/CT scan
- Fine needle aspiration (for staging)
- Treatment:
- Concurrent chemotherapy (cisplatin) and radiation
- 2nd round of chemotherapy
- Carboplatin and paclitaxel (Taxol)
- 6 rounds
- 2nd round of radiation
- Focus area: chest and near esophagus
- Immunotherapy
- National Institutes of Health trial
- Ended when one mass grew more than 20% during trial
- Targeted therapy
- Avastin for indefinite period
- Goal: to keep cancerous tumors from growing
- Diagnosis
- Tests & Staging
- Treatment Decisions
- Chemotherapy & Radiation
- 2nd Round of Chemo & Radiation
- Describe the 2nd round of chemotherapy
- Describe each cycle of that chemotherapy
- What were the 2nd chemotherapy side effects?
- Describe the 2nd round of radiation
- What were the 2nd radiation side effects?
- You underwent no surgery
- What was the result after this second round of treatment?
- Describe the moment you realized you still weren’t at "no evidence of disease” (NED)
- Immunotherapy
- CyberKnife Radiation
- Targeted Therapy
- Dealing with no standard of care
- Hair Loss
- Financial Support
- Emotional & Mental Care
- What helped most with the emotional and mental stress?
- How do you approach thinking about life and your future?
- What kind of outside support was most helpful?
- Did you and your spouse have different styles in approaching treatment?
- How did the diagnosis impact your relationship?
- What’s your message to those dealing with the same or any cancer diagnosis?
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
Diagnosis
What were your first symptoms?
It started off with a little bit of spotting or bleeding after sex. I remember it very clearly the first time it happened because it was Thanksgiving morning, and I was with my husband.
I was totally freaked out. I put it on the back burner because it was Thanksgiving. I chalked it up to having an IUD.
I made a lot of different rationalizations in my head.
A few weeks later, I ended up going to get a pap smear, and I was bleeding. I wasn’t supposed to have my period. It was my first time seeing that gynecologist. She reprimanded me, “You know you can’t come when you’re on your period.” I told her I wasn’t.
One thing led to another, and I was telling her about this. She said, “Okay, you know it is probably your IUD. I can’t see it right now, so I’m assuming that maybe it’s shifted or something, and that’s what’s causing this.”
Cut to a few weeks later, I was asked to make an appointment for an ultrasound. My insurance was saying, “We can only do it 6 weeks out.” I was waiting for an ultrasound, and then on Christmas Eve with my whole family around, my in-laws and my parents, I started hemorrhaging.
That really scared me, but I didn’t want to say anything because it was Christmas. I had my whole family here, and in a way I guess I was being a little willfully ignorant about the whole thing.
The next day, I ended up in the emergency room because it had happened again overnight. I spent the day after Christmas in the emergency room. I was there for 10 hours.
They did an ultrasound, but they told me they couldn’t see anything. They didn’t know what was wrong with me. They put me on birth control, saying I had something called “irregular bleeding” or something. But I knew something was off. I kept pushing to get the IUD out.

What led to the diagnosis?
Finally, I went to have the IUD surgically removed with a camera. The woman who did that procedure happened to be the specialist in gynecological biopsies.
As soon as they put the camera in my cervix, they saw a huge, massive tumor, and she was able to biopsy it right that second. They actually had another doctor come back to the hospital to confirm that it was a cancer diagnosis.
I woke up from thinking I was having a quick IUD removal to seeing my husband and asking him what happened, if they had got it out.
He told me no. Right at that moment, I just knew something was really wrong.
That night they told me I was anemic because I had been hemorrhaging so much. “You have to be in the hospital. You need a blood transfusion. This is definitely a cancerous tumor, and you need to start seeking treatment right away.”
After that, I went and met with the gynecological oncologist, and they did all of the scans. At that point, they diagnosed me with stage 4 cervical cancer.
You had to deal with misdiagnosis
To make matters even worse, when I had gotten the pap smear, it had come back for HPV. My doctor had referred me to get a colposcopy.
They cut some tissue and test it from your cervix, but they wouldn’t do the colposcopy because they said I was bleeding. They said, “We have to get the IUD out before we can do the colposcopy, because that’s what’s causing your bleeding.” But really it wasn’t at all.
They had been putting off actually doing the test that could’ve diagnosed the cancer. It was a really challenging time.
I have several women I know from the cervical cancer community who have had very similar experiences.
Describe the first biopsy
The biopsy wasn’t done until the end of February, actually. They had put me on this birth control and said, “You just have some irregular bleeding.” I was like, “Okay, whatever.”
I had gone to get the IUD out at another appointment. I’m not sure how familiar you are with IUDs, but generally a gynecologist can just pull it out and be done with it.
For whatever reason, they kept scheduling this appointment to get it out, and then they couldn’t see it. They couldn’t figure out why they couldn’t see it. Turns out it was because there was obviously a massive tumor in the way.
But they just kept saying that the IUD had shifted. It took me until the end of February of that year to actually get the proper appointment and get the diagnosis, even after I had gone to the emergency room.
Describe the 2 months before your diagnosis
There was more bleeding, more hemorrhaging. I remember being at World Market and having to run out because I was just hemorrhaging.
I was starting to develop really intense lower back and hip pain on my left side. I had been working out constantly, and I just thought that’s what it was from.
Again, I don’t know if I was at the time fully convinced of that, but wanting to think that. I was feeling progressively, progressively worse, to the point when I finally did get my diagnosis, I was almost relieved. Not relieved, but I just felt like this all made sense now.


How did you process the preliminary diagnosis?
My husband actually broke the news to me about the cancer. He had been informed by the doctor, who did the biopsy before I even woke up, that they found something and they were pretty sure it was cancer.
My husband was the one that told me. The doctor had asked him not to say anything to me until she was able to confirm or come back in the room.
When I asked him if it had worked and what was wrong, he said he just couldn’t lie to me or say anything. So he just spilled it.
‘They found something, and they think it’s cancer.’
I was just completely overcome with all different types of emotion. Like I said, relief. But of course, just utter, utter sadness and fear.
It’s kind of weird. I don’t know if this is something you would share with everybody, but I’ve always felt like in my life, I’ve always been waiting for the other shoe to drop or something.
When my doctor told me that, sitting in that hospital room, something clicked, and everything made sense in a way, even though it was absolutely terrifying and the scariest moment of my life.
»MORE: Reacting to a Cancer Diagnosis
How did you break the news of the diagnosis to your loved ones?
I was with my husband. I remember not being able to call and tell my mom. I asked my husband to do that. They admitted me to the hospital that night because I was so badly in need of a blood transfusion.
I broke the news to my family and friends. It was hard. For my parents, my husband is the one who originally told them of the diagnosis. I called my best friend, who’s really more like a sister to me, honestly. I’ve known her since I was 8. I told her.
At that time, I said I assumed it would be an early stage of cancer. I just thought, “Okay, I have this, and we’re going to get through this.” I remember I was more concerned about their feelings and telling them these things than I was about myself at that time.
When I had to tell my parents about the staging, that was hands down the hardest thing, having to tell them that I was stage 4B. That night I think I had a crazy, large glass of just gin to get through it.
I just remember saying, ‘It’s really not good, you guys. I’m going to do the best I can, but it’s really not good.’
My husband thankfully has been an amazing caretaker in all of this and has done all of the research and everything. He was able to research more of the details.
I found having to tell other people to be literally the hardest thing about this. I find it so hard to have to share with my loved ones.
»MORE: Breaking the news of a diagnosis to loved ones
Tests & Staging
What were the tests, scans, and biopsies that you had to undergo?
- Ultrasound
- Pelvic mass biopsy
- PET/CT scan
- Fine needle aspiration
When I went to the emergency room, I underwent an ultrasound. I don’t know why that didn’t pick up anything, but apparently it didn’t. After that, I had the original biopsy of the mass in my pelvis.
Then I had a full PET/CT scan, which showed that it had spread to lymph nodes and my abdominal area. Then also it spread to a lymph node in my neck. I had to have what is called a fine needle aspiration, which is basically a biopsy that they do.
They stick a needle in a lymph node if it’s surfaced, if it’s close enough to your skin. That did come back and confirm that the lymph node in my neck was positive for cancer. That’s how we ended up getting not only a stage 4, but a stage 4B diagnosis. That’s the absolute worst one you can get.
That literally all happened within 3 days, so I was going, going, going, constantly doing things to get the diagnosis.
There were doctor appointments every day. Then that Friday, when I knew I had all weekend and I got the final diagnosis, that’s why I collapsed a little. All the tests were done; all of that was done. It was just those words. Then you go home and somehow try to continue your life.
The only question I could get out was, “Can I still do yoga?” I do a lot of yoga now, but at that time, I don’t know why I asked that. I thought it would make me seem healthier or something. I just remember how dumb I felt after I said that.

Describe the pelvic mass biopsy
It didn’t hurt at all. I was put completely under general anesthesia. It was supposed to be a quick in-and-out procedure. Basically they put you under. and you go home that same day.
No issues. It wasn’t painful. Because they had found me to be so anemic, that’s where all the complications had come in.
The biopsy was a couple of hours because they basically weren’t going in to biopsy it. They had to scramble and get everything together while I was on the table.
Describe the PET/CT scan
I had never done one before. I’m someone who suffers from anxiety, so I remember being really, really scared about going into the machine. I’d always heard that people with anxiety or people that are afraid of close quarters don’t do well.
I was more scared about flipping out and having a panic attack than I was about anything that would come up in the results.
Honestly, it wasn’t as scary as I made it out to be. They did pretty heavily sedate me at that point, but that’s okay.
If there’s a message there, it’s okay to ask for Xanax if you’re scared of the imaging machines, or just if you’re scared about getting them.
I had to be in the machine at that time for about 15 or 20 minutes. I’d never had a scan like that before, where you’re fully immersed in a machine that’s completely surrounding you for that long. I never had one like that.
Describe the fine needle aspiration
The fine needle aspiration biopsy also wasn’t painful, but just very scary. That one, you’re under local anesthesia, and you can tell someone’s basically digging around inside your neck.
It’s just very uncomfortable, but also very quick. The fine needle aspiration was maybe 10 minutes total.
How long did it take to get staging?
Staging only took a few days. We worked really, really quickly. That night when I was in the hospital, I had emailed my work and said, “Look, I’m not going to be in for probably a week. I have some crazy health stuff going on.”
Within a couple of days, we had gotten the staging. I went into the hospital on a Tuesday, and it was that Friday actually when I got my official diagnosis.
Do you remember the moment you got the staging?
After scans and everything, when I was told it was actually stage 4, I lost my thought of, “I can get through this. I can do anything.” I really just fell apart for a few days at that point.
They had prescribed to me some sort of narcotic pain pill for all of the pain I was having in my back. They told me on a Friday, and I totally felt medicated for that entire weekend.
My parents were down, and I just look at myself in photos from that time or even a little bit before that. I just see how gaunt and drawn I looked. I didn’t have any blood, so I distinctly remember just sitting in the little exam room with my back up against the wall with my husband.
The doctor told me it was stage 4. “We’re going to give you the best that we’ve got, but we really don’t know how much good it will do.”
At that point was when I was really like, “Holy shit. I don’t know if I can do this.”
Treatment Decisions
Did you get a second opinion?
I did decide to get a second opinion, because I knew you have to be your own advocate.
I’m lucky enough, living in the Washington, D.C., area and having the insurance that I have because my husband’s active-duty military. I was easily able to get the referral for a second opinion and go to Johns Hopkins.
I saw a really great gynecological oncologist there who was a woman, which for some reason made me feel better. Up until recently, every single one of my doctors had been male. I was able to meet with her, and she said, “I know your doctor at that hospital you’re going to. I think this is the absolute best course of action.”
Let’s be honest, at stage 4B, there’s not a ton of options there. If you can, you undergo radiation and chemotherapy, and those are really your only options. Just hope that they knock out as much of it as possible.
But I still thought it was important to see another doctor and ask the questions because I wouldn’t have been able to forgive myself if I had left something on the table.
»MORE: How to be a self-advocate as a patient
How did you decide where to get treatment?
I didn’t really have any options there because my husband’s active-duty military, so we have to go to military medical facilities. I ended up with this team of doctors because that was my only option, unless I had gone to Johns Hopkins for the second opinion and they said, “Absolutely not. We would do things completely differently.”
Then I could have left to go somewhere else. I ended up getting treatment at Walter Reed, where I’m still getting treatment, just because of how our insurance system works.
Is the hospital you’re at now a smaller hospital or larger medical center?
I would characterize it as pretty small because you have to be either active-duty or retired military to go there. I don’t know how many people that they treat, to be honest. I would say it’s probably a smaller hospital. It’s not MD Anderson or the Mayo Clinic by any stretch of the imagination.
What have been the pros and the cons to the hospital size?
We’ll start with the cons. Even though my team is amazing and they work with the best of the best, I feel like I have to really advocate for myself because they are a smaller hospital. Especially being a military hospital, dealing with the gynecologic cancer.
I’ve had to do my own research [to] see what clinical trials are offered around at different places. It just helped to be on top of that for myself. I think at some of the larger hospitals, there are more resources there, as far as that goes.
The pros are definitely that I feel really comfortable there because I know my doctors really know who I am individually. I have what’s called a nurse navigator. I know a lot of places do this, but any time I feel any weird ache or pain, feel like I need a prescription, or feel like I need a test or something, I can just text her. She always gets back to me within an hour.
I just love being able to have that. It’s a big asset to me. When I was at a bigger center, if I had any questions, I’d have to submit a question through a form. “Then we’ll email you back.” There are a lot more levels of bureaucracy there.
Describe getting the port put in
I got the port put in a couple days after my diagnosis, before I even had a second opinion. They said they needed to move and no matter what kind of treatment I did, I would probably need some sort of infusion, so I got the port put in.
The procedure was fairly easy. They put you under local anesthesia. You basically don’t feel any pain, but it’s uncomfortable, and there’s some tugging.
They put you in what I think is called a twilight sleep, so while you’re not necessarily completely zonked out, you’re not really aware of what’s going on. It’s a pretty quick procedure, maybe 30 minutes.
How was recovering from port surgery?
What I was not expecting was how painful the recovery was, or maybe I had just been so jilted by that point, I didn’t care. I had made plans to hang out with my friends that night of getting the port placed, and I was in so much pain just from the whole procedure that I couldn’t even think straight.
I remember I ended up leaving, going home, and just taking the pain pills they gave me and going to sleep for the rest of the weekend, because this was also on a Friday.
I was a little surprised by that. People are always like, “I’m getting my port line placed,” and everyone’s like, “Oh, it’s no big deal, blah blah blah. You’re fine.”
I always want to be that one detractor who says, “Not to scare you, but just so you know, it can be a little painful afterwards. Just don’t plan anything. Take the time to recover.” All of that.
That was something, but I obviously recovered in a couple of days. People tell me I’m really lucky because the scar isn’t very pronounced, so that’s good.

Chemotherapy & Radiation
Describe the first round of concurrent chemo and radiation
The original treatment, my first treatment I had was a combination of chemotherapy and radiation. The chemotherapy was intended to boost the effects of the radiation.
I did that for about 6 weeks, where I would get cisplatin every Monday. Then I would do a full 5 straight days of radiation to my pelvis and to the lymph node in my neck.
For about 6 weeks, I did cisplatin every Monday, which was through an infusion, like regular chemotherapy. The intention of that chemotherapy was just to boost the effects of the radiation therapy.
I went every day, every Monday through Friday, for 6 weeks to radiation every day to have radiation to my pelvis and to the lymph node in my neck.
What were the treatment side effects?
I believe it was about 2 hours every Monday. Right after that, I would go into radiation. I didn’t really have any side effects directly from that cisplatin chemotherapy.
It generally doesn’t give you a lot of side effects. They also had me on a great deal of steroids and anti-nausea to combat any of the side effects.
I would say some of the side effects of the steroids, as I think anybody who’s had chemotherapy knows, almost seem worse. I’d rather just be nauseous than deal with some of the steroid side effects. I just never could sleep. I always felt out. I just didn’t feel right.

But from the radiation, it started off on an upward swing. I started to feel better because it was working, and the pain in the neck was going away. Let’s say that’s the first 2.5 weeks of the 6 weeks.
Then it starts to go downhill a little bit, where it’s like you’re no longer getting all of that excitement from the good effects of it, and you’re starting to get more tired and more nauseous. I remember I went to lift a box with clothes in it, and I almost passed out. I was so weak and so tired.
What helped with those radiation side effects?
During that time, I had to have 3 or 4 blood transfusions because I was already fairly anemic from all of the hemorrhaging. A lot of your red blood cells are made in your pelvis, so if you’re radiating your pelvis within an inch of its life, your body can’t make blood cells.
There were several times when I would get lab work done, come home, and have them be like, “You need to come back. Your red blood cells are so low. I don’t even know how you’re functioning.”
That was definitely a lesson to self-advocate because I just assumed that that’s what it felt like to have cancer. I didn’t think, “Oh, there’s something wrong.”
It’s a side effect of something, and so that was a really good lesson for me to learn that you don’t have to feel terrible.
»MORE: Cancer patients share their treatment side effects

Describe the blood transfusions
It’s like a chemo infusion, except there



