Tina’s Stage 3A ER+ Invasive & Lobular Breast Cancer Story
Tina C., DCIS & LCIS, Stage 3A, ER+
Symptom: Sunken in nipple of right breast
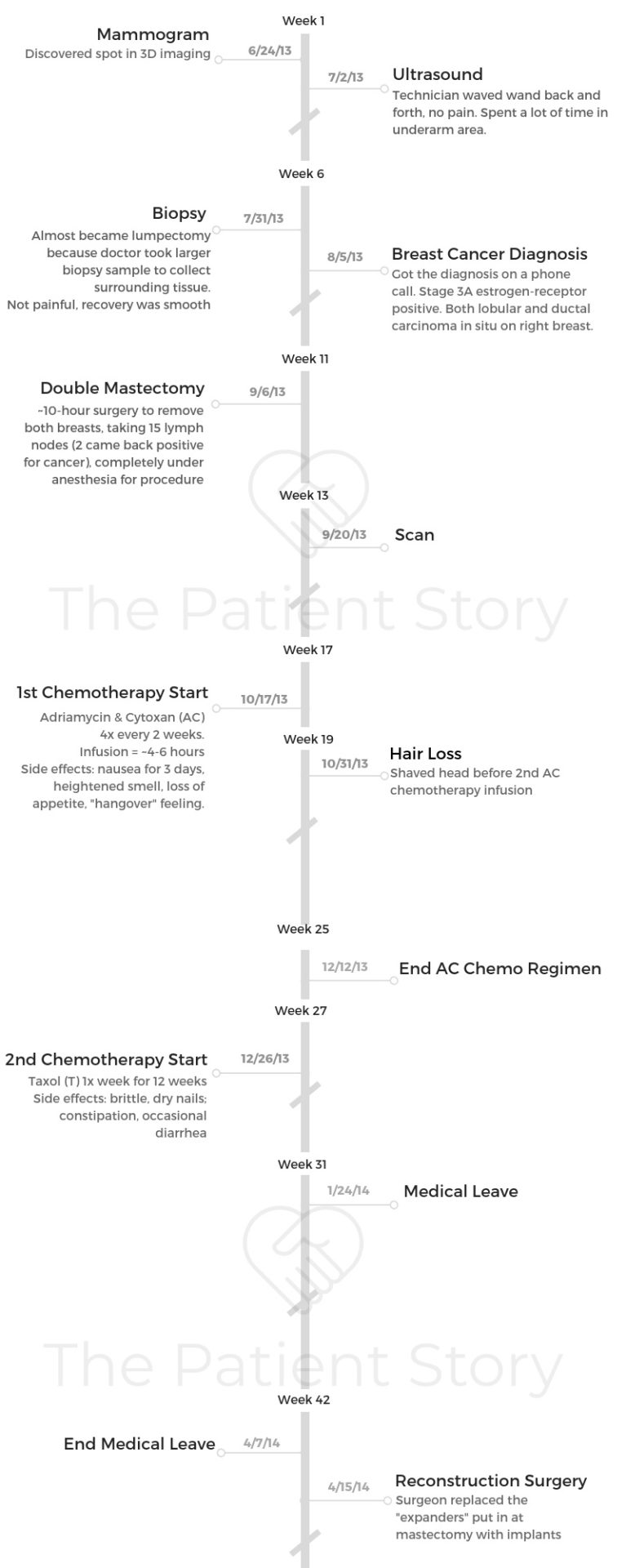
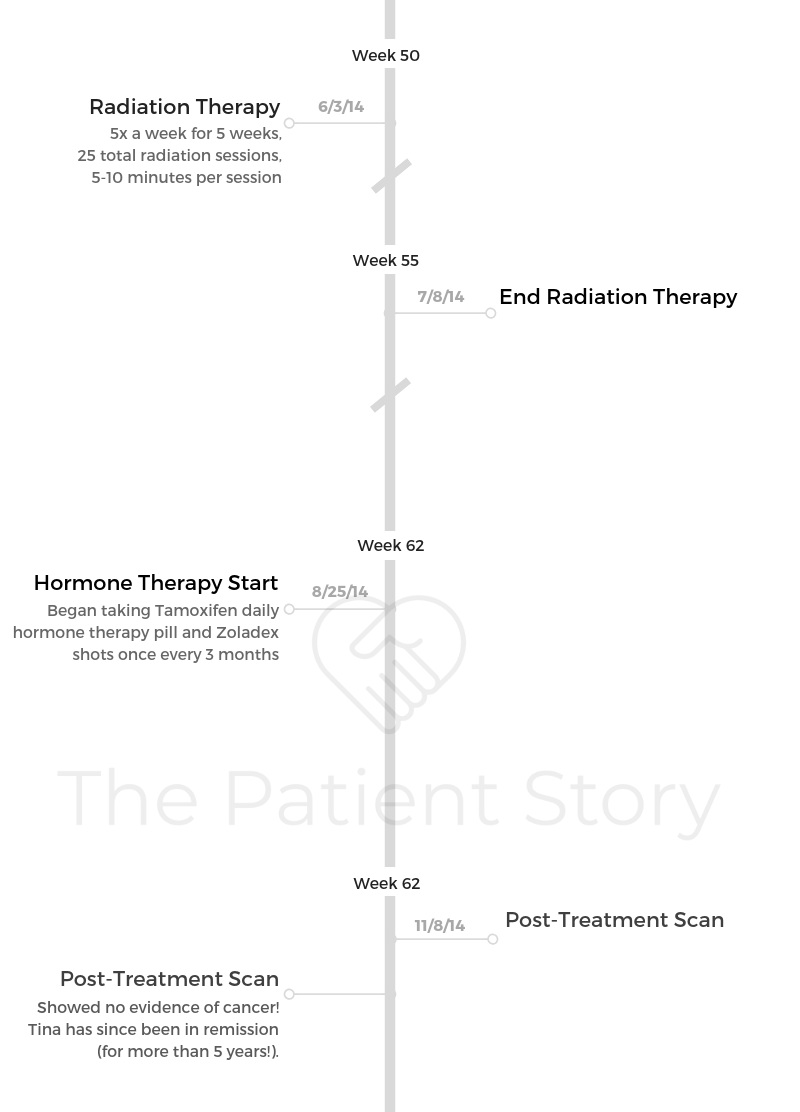
Treatments: Double mastectomy, chemotherapy (AC-T), radiation, hormone therapy (tamoxifen, Zoladex)
Tina’s Stage 3A ER+ Invasive & Lobular Breast Cancer Story
Tina shares her in-depth story on getting diagnosed with stage 3A breast cancer after noticing a sunken nipple. She details undergoing a double mastectomy, chemotherapy, radiation, and hormone therapy.
Tina also highlights how she managed through the trauma of losing her hair, dealing with work and finances through treatment, and the importance of self-advocacy as a patient.
- Name: Tina C.
- Diagnosis:
- Breast cancer
- Ductal carcinoma in situ and lobular carcinoma in situ
- Estrogen receptor positive (ER+)
- Staging:
- 3A
- 1st Symptoms:
- Sunken in nipple on right breast
- Treatment:
- Double mastectomy
- Chemotherapy
- Adriamycin & Cytoxan (AC)
- 4 times every 2 weeks
- Taxol
- 1 time a week for 12 weeks
- Adriamycin & Cytoxan (AC)
- Radiation
- Hormone therapy
- Tamoxifen: 1 pill daily
- Zoladex: 1 shot every 3 months
- Diagnosis
- What were your first symptoms?
- Describe that first primary care visit
- Differences during this mammogram
- It moved quickly to a diagnosis
- Describe the mammogram
- Describe the biopsy
- What do you remember most of the biopsy?
- How was the wait for test and biopsy results ("scanxiety")?
- How did you deal with the wait for answers?
- Describe the moment you got “the call”
- How did you break the news to loved ones?
- Do you remember how your oncologist described to you what 3A estrogen positive means?
- You had both lobular and ductal carcinoma in situ
- Treatment Decisions
- Did you get a second opinion?
- How did you find your oncologist, surgeon, and radiation oncologist?
- How did you decide who to go to for treatment?
- Describe the treatment center you went to
- What did you like about it?
- Did you make the decision to undergo a mastectomy?
- Did you have a choice to pursue chemotherapy?
- Surgery (Double Mastectomy)
- Chemotherapy
- Reconstruction Surgery
- Radiation Therapy
- Hormone Therapy
- Hair Loss
- Work & Finances
- Support & Care
- How did you manage the mental and emotional stress during treatment?
- It’s hard to slow down for many. Any tips?
- Were there big surprises during treatment?
- Finding your community
- Were there moments you had to self-advocate?
- How important was it to have caregivers around?
- Any advice on how to ask for support?
- Survivorship
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
It’s definitely a roller coaster. There’s going to be ups, and there’s going to be downs. In some ways, you’ll appreciate the journey. Looking at it on the other side is just totally different. It’s amazing, and you just appreciate more, but it’s not easy.
You have to talk to somebody if you find yourself just staying in a down place. You need to.
Tina C.

Diagnosis
What were your first symptoms?
I remember at my wedding thinking something just seemed a little different with my breast. That was in April of 2013.
The nipple on the right side had sunken in a little. I thought, “Oh, that’s odd or strange,” but I really thought, “Oh, getting old sucks,” even though I was 37.
In my mind, it didn’t really click, even though my mom has had breast cancer 2 times. It was always a lump, so I just ruled it out for a little while.
Another couple of months passed. Something happened with someone at work, totally unrelated to breast cancer, but it just made me take inventory of my own health.
I was like, “You know what? This hasn’t changed with my breast. I don’t know what’s going on, so I’m just going to go have a talk with my OB-GYN.”
Describe that first primary care visit
I went in about June and had a conversation with her. She said, “It’s probably nothing, but let’s just get it checked out.”
I had a mammogram when I was 30, and I had one when I was 33, so I had a pretty good baseline at that point in time.
She scheduled my mammogram pretty soon thereafter. I went in and got the mammogram. It seemed normal, so everything seemed to go the way it had in the past, except I got a call back about another week or so after the mammogram that something was abnormal and that I needed to come in. That was definitely unique to what had happened in my previous mammograms.
Differences during this mammogram
For the second mammogram, my husband went in with me. From there, they did an ultrasound. They had never done an ultrasound before.
They were spending a lot of time in my armpit area, which I knew enough about my mom’s diagnosis to know that that’s where your lymph nodes are. Something’s obviously unusual.
They wouldn’t tell me anything while I was lying there, so I had to wait until the doctor could come and officially read it. He came in and said, “Well, I know you know something’s not right.”
They needed to do a biopsy. I could choose to either do a needle biopsy or meet up with a surgeon and have a surgical biopsy.
Because of my mom’s history, I did choose to meet with a surgeon and go that route. From there, I did do the biopsy. I think that was in probably late July.
From that biopsy, I woke up to my breast surgeon telling me, “I think you need to get your mom’s records.” That was the first thing I woke up and heard.
That was on a Thursday. I took Friday as a mental day. Then on Monday, I got the official diagnosis that it was cancer.
It moved quickly to a diagnosis
It escalated pretty quickly. It was good that everyone took me very seriously, even though I was 37.
I think that me having my mom’s diagnosis gave me some credibility. Nobody second guessed what I wanted to do. Everyone was very obliging of what I needed to do.
Describe the mammogram
The mammogram was just a normal mammogram, where it squeezes one breast at a time. I’m not very large-chested, so I never had any pain or any issue.
Nobody really reads you the results right then and there. Certain clinics have different procedures, but the one I was at, they definitely waited. Your actual doctor talked to you about it, or sometimes you get the thing in the mail later that everything was okay.
The ultrasound was a wand going back and forth, back and forth. They were looking at the breast with the wand, but they were spending a lot of time in my underarm area. Then another person would come in.
I think the hardest part was nobody would talk to me, so it was really frustrating. I’m a human being sitting here. Can’t you at least just tell me what is going on?
I understand that there’s procedures. Different people read different things, and only certain people can also tell you what’s happening. I was not naïve enough on this case to know that there was probably a problem.
It felt very frustrating to lie there. I remember lying there with the ultrasound wand and just having a tear go down my face because I knew something was happening, but nobody would talk to me.
»MORE: How to be a self-advocate as a patient
Describe the biopsy
It actually ended up being almost a lumpectomy because when she got in there, she could definitely tell things weren’t right. She took more than what a tiny needle biopsy would’ve done. It is almost like she performed a lumpectomy and tried to take the surrounding tissue as well.
It wasn’t very painful, and my recovery wasn’t very hard. It was the tip of the iceberg, so emotionally it was very hard and very difficult, but physically it wasn’t that big of a deal.
I’ve had so many surgeries. I think it was just local [anesthesia], and I went home later. It was an in and out. Obviously, the mastectomy is totally, totally different.
I had some bandages and dressing to change. I remember more the emotion than I remember the physical part of it.
What do you remember most of the biopsy?
Just to hear, “Get your mom’s records,” was truly, truly eye-opening. I always felt in my heart that me getting breast cancer was definitely possible, but my mom was 46 when she was diagnosed. I never in my wildest dreams thought I would be in my 30s. I don’t know why. I just thought that seemed crazy.
I thought if it would happen to me, it would happen later in my life. My mom did get her records in order and get everything sent over. I spent the weekend calling everyone that I loved and telling them, “Hey, this is likely going to happen.”
It was very emotional, but it did allow me to process it with a bunch of people a little bit before I even heard the official diagnosis.

How was the wait for test and biopsy results (“scanxiety“)?
Each was probably a couple weeks. It seemed the wait got shorter the more engrossed it was. From the first mammogram to the second mammogram, it was probably a couple weeks.
Each thing just seemed to take some amount of time. It was probably 6 to 7 weeks from that point to get the full diagnosis. I had my biopsy on a Thursday. I got my official diagnosis the following Monday that it was cancer. By the end, things were moving rather rapidly.
»MORE: Dealing with scanxiety and waiting for results
How did you deal with the wait for answers?
I tried to just live my normal life. I had been promoted in February of that year, so I had still a relatively new job. I really just tried to immerse myself in work and my life. Not trying to worry about it so much, but then everything had to change once it became a cancer diagnosis.
Leading up to that point, I felt like I just tried to — I don’t want to say ignore it, but just tried to remain calm and just be myself as much as I could.
Describe the moment you got “the call”
I’m sure my story’s not too unique to anyone else’s. Even with having the doctor tell me on Thursday that, “Hey, get your mom’s records,” there’s still just this glimmer of hope that everything is for some reason going to be okay and not a cancer diagnosis.
I went back to work on Monday. I think I got the call 3:30, 4:00 in the afternoon from the doctor. I walked away from my desk. I remember them saying, “You have cancer.”
It’s just the hardest thing. The whole world stops. Everything that you felt and hoped and wanted to do — just everything just suddenly changes.
I often say it’s just a line that’s drawn. You can never go back to that pre-period. It’s just different from that point forward, so life as I knew it definitely changed. For the next year, everything definitely changed.
It is that raw emotion. It just really comes back and takes you back to that very day that you found out.
»MORE: Processing a cancer diagnosis
How did you break the news to loved ones?
My husband actually worked at the same place as I did, so I emailed him and was like, “Hey, we’ve got to go.” I’m sure he knew at that point.
Plus, everything leading up to it. In the car I was able to just be sad and let it all out. I waited to tell everyone at work maybe a week, just to give myself some time to process it.
We actually set up a meeting. I had a good discussion with my boss. At that time I was leading a team of about 10 people, so we invited the whole division basically. My boss framed it up like, “Hey, we are a family, and sometimes families go through tough times.”
It was good to have their support from the very beginning, understand what was happening, and to hear it more from me and not hear it just through the grapevine.
I’m definitely more of an honest person who’s just going to tell you what’s happening. Let’s find the best way to treat it and to move on.

I think it was probably the hardest for my mom. She was living in Michigan, and I was living in Chicago suburbs at the time. For her to be 7.5 hours away, she definitely felt a lot of guilt.
She felt like she caused it or it was because of her genetics or something. She had a really hard time dealing with it at the beginning.
I remember one of my aunts who lives in the same hometown emailed me and said, “Your mom is really not taking this well. She’s blaming herself. She’s just not doing good.”
I called her, “Hey, I heard that you’re not taking this well [and] that you’re blaming yourself.” She’s like, “Yeah.” She got really quiet.
“Well, I can’t worry about you doing this. I don’t blame you.” I told her I didn’t blame God. I just told her, “Hey, we just have to deal with this. We just have to move forward and deal with this.”
I released her of those feelings. She could come to terms with it. [She] just supported me in the best way that she could from that point forward.
She couldn’t obviously make it to everything, but she came and stayed with me for a week during my mastectomy and my first chemo. Definitely, she was the hardest one to break it to, outside of my husband.
»MORE: Breaking the news of a diagnosis to loved ones
Do you remember how your oncologist described to you what 3A estrogen positive means?
I tried to negotiate with him.
Tina: How about 2C? There’s not a lot of difference between 2C and 3A.
Oncologist: No, it’s really 3A.
Tina: Yeah, but 2C just sounds so much better.
I remember having that conversation with him, but the size of the lobular mass that I had [was bigger]. I also had ductal cancer. It is crazy that I had 2 kinds of breast cancer.
I don’t even have the same cancer that my mom had, which is even crazier. That was very interesting to learn. My mom had triple negative; that’s a very tough type to have, and it’s usually very ferocious.
Mine is some blessing. I had multiple conversations, I remember, talking to my breast surgeon.
Tina: Well, is this a better kind to have then?
Breast Surgeon: The fact that there is a treatment that after chemo can help you, then yes. That is the better thing.
We had our conversations about it, and the fact that mine is hormone receptive — there are drugs that can help me post-treatment — was a good thing to have and to understand, even though that drug for many people comes with a lot of side effects.
You had both lobular and ductal carcinoma in situ
Yes. Lobular is like spider-web crazy, and that’s actually what pulled the nipple in. Ductal was more like a lump in the ductal gland. That’s the kind my mom had.
Ductal typically forms a lump, but the lobular is just this mass of a spider web, and it’s just messy random things growing together. Both were on that same right breast.
Treatment Decisions
Did you get a second opinion?
I think they were still staging it at that point in time. With the fact that I had a surgeon, it wasn’t just some needle biopsy, and that she got in there and clearly could see something — I guess I felt that this with my mom’s prior history, too, that we just need to move forward.
I was pretty clear with my surgeon from the beginning, like, ‘Hey, if this is going south, I want a double mastectomy. That’s just what I want.’ She was always very accommodating of what I felt I needed.
How did you find your oncologist, surgeon, and radiation oncologist?
I lucked out. I just felt most all my surgeons fell into place. It seems my OB-GYN had worked very closely with the breast surgeon that I had, and I really her. She worked very closely with a plastic surgeon. He was really great to work with for reconstruction.
She also was familiar with an oncologist, so that’s how I got in touch with him. They were all in the same network or same hospital, because they all shared the same operating rooms and different things.
The only one that I bucked the trend on was my radiation person. After a consultation, my husband was, “No. I’m not allowing it.” I just had this feeling, and then he verbalized what I felt. He was just like, “No, we’re going to get somebody else.”
How did you decide who to go to for treatment?
I’ve talked to other survivors, and it’s amazing. I always say, “Listen to your gut.” You want a smart person, and you want someone very capable. You do want good bedside manner. I’m not saying that’s most important, but you do want some good bedside manner.
[The first surgeon] took 2 personal calls during my consultation, left me with an iPad, and said, “It’s this, but it’s not.” I was like, “Well, what part is that? What part is not?”
I was also like, “If you can take 2 personal calls to an appointment that means the world to me, then I don’t think it means the world to you.” I think you just have to find a doctor that you feel is as invested in this, in your cancer journey, as you are.
If you don’t have that feeling, you should get a second opinion. You should talk to somebody else. There’s always options.
They might not be as convenient, but you should always look into options if you don’t have the feeling that they’re on your team.
Describe the treatment center you went to
It was fairly newer and fairly mid-size probably. It was part of Advocate Hospital, which was a bigger network in Chicago, but it was one of the outlets for it.
What did you like about it?
I would definitely say for me it was convenient. I don’t feel people should just make a choice based off of conveniency, but it was convenient to get to for still trying to work and still trying to have some normalcy to life.
I knew other people who would go downtown Chicago from the suburbs, but you’re talking maybe a 2-hour drive there, 2-hour drive back with traffic, depending on the time of day. It was on my way home from work. I could schedule things easier with my lifestyle.
I actually felt the caliber of doctors was amazing, the people that I had. I don’t know if I just lucked out with the team that I got, but once I had that team, I really felt they were a dream team. They just all gave me such great advice. They even advocated for me.
I ended up taking a medical leave at one point in time because my oncologist asked me tough questions, and I needed it.
Oncologist: Who’s your advocate at work?
Tina: My manager. She cares about me.
Oncologist: No, no, no, no. I’m not talking about caring. Who is your advocate at work?
Tina: I don’t have one.
Oncologist: Well, then I really need you to consider taking a medical leave.
He just put it in very black-and-white terms that I needed to hear. He was very resolute, like, “You need to consider this.” He wouldn’t tell me necessarily what to do, but he would always put it in a way that was black and white.
Sometimes when you’re so confused in the whole process, you do need someone that tells you [how] it is. I’ve always felt like that’s how he would treat his friends. That’s how he would treat an aunt.
He would do the same thing to any one of us, so I just appreciated his candor and his honesty all the time.
Did you make the decision to undergo a mastectomy?
I definitely was an advocate for it, in that my one side ended up having lobular and ductal. Lobular was pulling the nipple in and was a hot mess inside there. I think lumpectomy would never even have been an option for that side.
I just didn’t want to have to worry. I wanted things to be symmetrical. In my mind, my mom had a lumpectomy, it came back, and then she got a double mastectomy. That just meant some more peace of mind for me.
But I understand their statistics. Everything’s always changing. Maybe it’s not necessary, but for me I did have peace of mind doing it. No one ever really questioned it, and it wasn’t a difficulty at all.
Did you have a choice to pursue chemotherapy?
My oncologist showed me a piece of paper, and I used to think that I liked statistics, but then he made me realize I’m not sure if I do.
He told me if I did no chemo and no radiation, my chances of dying from cancer in the next five years were 50%. That’s pretty humbling news, so in my mind, that’s not an option.
Surgery (Double Mastectomy)
Describe the prep before the (double) mastectomy
I remember going in early in the morning, talking with the anesthesiologist, and them wheeling you back. It was a really long surgery. Between taking both breasts, checking the lymph nodes, and then putting expanders in, it was about a 10-hour surgery, maybe 11, which is a very long time for anyone to be under.
I even had my in-laws come and stay with my husband because I was worried about him just being there by himself for so long, too. They came and were part of it, which was amazing to have that support. If it’s a double (mastectomy), just plan that things can take a very long time.
Describe the double mastectomy
I understand some people start off with chemo to see if markers are shrinking and different things, but in my case, they wanted to do the surgery first. They did the double mastectomy right after Labor Day. Within a month of my diagnosis, I had the surgery done.
They took 15 lymph nodes on the one side, and then the other side they took off as well. Of the lymph nodes, 2 came back with cancer in a macro way and then 2 micro, but definitely 4 were impacted by cancer.
The good news is there were 11 that were not, and that was pretty much the extent of the cancer, from the scans and everything else. The surgery was very challenging.
It’s just a testament to being in a weird position for so long. There can be other side effects, actually. My toe hurt for a couple of days, which is crazy. I’m not saying that’s going to happen to anybody else. but just the way that they position you and being under for so long, you know it’s a long time.
I remember coming back to the room, and at first I felt really great, but I still was probably under the pain medication, everything that they had given me. Then a wave of just feeling nauseous and horrible. Then a nurse came in and said, “You look so pale; we’ve got to give you something.” I had to take some more medicine.

That first night was pretty rocky, and I spent 2 nights in the hospital. On that third day, I went home. By then I was ready to go home, but that first day and a half, it’s really tough.
I have never been in a hospital since I was an adult, so it’s just difficult to have someone come in your room and check on you every couple of hours.
Those machines, when your legs are moving and making noises, it’s just a whole different world. Some people are maybe more used to it from having surgeries as an adult, but for me it was definitely a learning curve.
»MORE: Read more patient experiences with surgery
What were the side effects after surgery?
You’d go home with drains that had to stay in for 2.5 to 3 weeks. Then you had to go in and see your surgeon. They put expanders in at the same time to get the skin ready for the upcoming implants.
The whole mobility thing was really, really challenging. Mentally I felt fine. I wasn’t really tired afterwards. I could walk [and] do things, but just learning how to eat cereal or just put on a shirt was very, very challenging.
I wanted to wear button-down shirts because it’s just really difficult to get anything over your head and raise your arms.
I remember eating cereal with my left arm because I felt [like] a caveman, but I felt a caveman either way, whether I eat with my right hand or my left. It was just crazy to relearn some things that are so simple.
I did these “Itsy Bitsy Little Spider” exercises all the time to run your fingers and stretch your mobility. I definitely took it seriously and tried to work on all the exercises they had you do.
When you’re in the midst of it, you just feel, “Am I ever going to be normal again?” It’s definitely a very slow and gradual journey. From that point forward, it takes a long time to feel right again.
How long did it take to recover?
The first week at home, my mom was with me, so she did all the cooking [and] all the laundry. It was very helpful to have someone there, because I couldn’t lift. I was very limited in what I could do.
I don’t even think you can even lift a half gallon of milk. You’re probably not even supposed to. You’re very limited in what you can lift and how much weight your arms can raise.
I couldn’t take a shower because of the drains, so that was really difficult. Had I thought things through, I would’ve maybe cut my hair shorter, knowing I was going to go into chemo and do that next. Just because the showering part or having to take a bath is so much more complicated, and obviously brushing your hair is really difficult.
It’s pretty humbling to be 37 years old and having your mom give you a bath and comb your hair and do all those things. You’re an independent woman, so it’s really difficult and humbling. But I made it through, and all I wanted to do was shower. It was my end goal.
I do remember when the bandages came off, and at that point in time, my mom had stayed with me for a week. My best friend had come and stayed with me for 4 or 5 days, so I was finally alone. The weight of it all was just enormous.
Seeing myself with just this body I didn’t recognize, the emotional toll of it — that was really hard. Probably more than even the physical part of it.
Describe the drains
They fill with fluid, but you had to measure the contents [to see] how much was draining. I had a little checklist, and we had to get it down. When they finally got to a certain amount low enough, then the drains were able to be removed.
Basically, it was tubing inside of you that connected to this little bulb. For me to leave the house and go do anything, I had to pin the [tubing] together. I didn’t want them showing, so I had to hide them in some way.
What were the expanders put in during the mastectomy?
They put in these expanders, and then they would fill them every week or every 2 weeks. I’d go in and see my doctor, he put a little more cc’s [of fluid] in [the expanders] each time to gradually stretch the skin so that next April I had the exchange surgery. Then those expanders came out and actual implants went in.
Chemotherapy
Describe the surgery to put in the port (used to deliver the chemo)
I didn’t have any issues with it. You could shower. I think you could go swimming, even though swimming was obviously not advisable. You could do whatever and live your normal life.
To me, it was more so I just felt like an alien. If you just have this weird thing sticking in your upper chest, your clavicle area, it just looked weird. I just felt like I looked like a mutant or not a human.
But it really was convenient because, obviously, they don’t have to find veins every time, and you don’t have all that. I was fortunate I never had any infections or any issues with it. It actually was quite a convenience once I look back and look at it now.
What was your chemotherapy regimen?
Chemotherapy regimen:
- Adriamycin & Cytoxan (AC)
- 4 times every 2 weeks
- Taxol







