Bruce’s Gleason Score 8/9, Stage 4A Prostate Cancer Story
Bruce M., Prostate Cancer, Stage 4A, Gleason 8/9
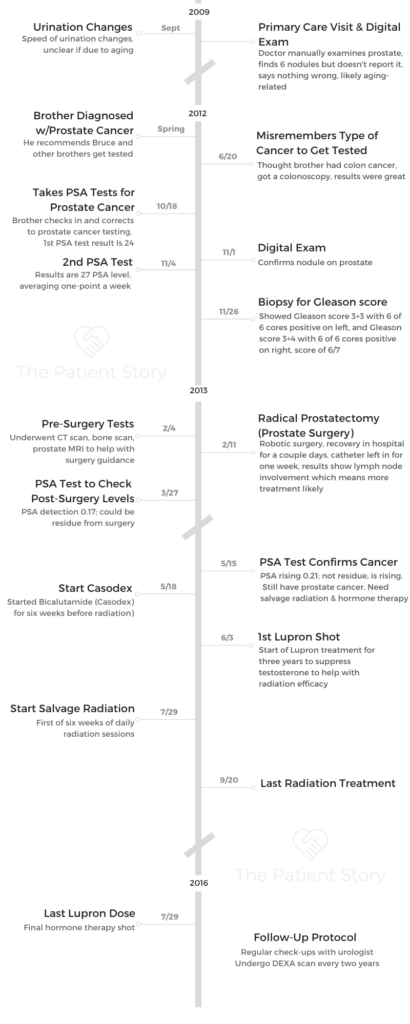
Symptom: Urination changes
Treatments: Radical prostatectomy (surgery), salvage radiation, hormone therapy (Casodex & Lupron)
Bruce’s Gleason Score 8/9, Stage 4A Prostate Cancer Story
Bruce shares his stage 4A prostate cancer story, Gleason score 8/9, which began with a diagnosis at just 51 years old. He details going through a radical prostatectomy (surgery), salvage radiation, and hormone therapy.
Explore Bruce’s in-depth story below, where he highlights many important quality of life topics, including the impact of hormone therapy on sexual function, the importance of self-advocacy and awareness, why it’s important for men to share their stories and ask questions, and the transition to survivorship.
- Name: Bruce M.
- Diagnosis (DX):
- Prostate Cancer
- Gleason Score 8/9
- Stage 4A
- DX age: 51
- 1st Symptoms:
- Velocity change of urination
- Discovered cancer after brother was diagnosed with aggressive form of prostate cancer
- Treatment
- Radical prostatectomy: surgery to remove entire prostate and surrounding tissue
- Salvage radiation
- 6-weeks
- Every Monday-Friday
- Hormone therapy
- Casodex
- Lupron shot (three years)
The phrase that I hear people say is that it’s living with cancer. That’s really appropriate. I’m living with that knowledge that it could come back. It might get me in the end, I have no intention of it doing so, but it’s something I just realize is part of my life now.
I’ve accepted it as okay, that’s just what it is, I’m just going to move on and keep living my life. I think it’s really just not letting it rule your life, just knowing it’s a part of your life, and you want to rule it as opposed to it ruling you.
Bruce M.
- Meet Bruce
- Video: Bruce on Getting Diagnosed
- First Symptoms and Test
- What were the first symptoms
- What happened at the first doctor visit
- Your brother’s prostate cancer diagnosis pushed you to get tested
- Was your brother going through prostate cancer treatment at the time
- When did you realize you may have prostate cancer
- What is the PSA test
- How long did it take to get the PSA level results
- Getting Diagnosed with Prostate Cancer
- Describe the urologist meeting
- Results of the second PSA test
- Describe the digital exam
- Describe the biopsy
- Recovering from the biopsy
- Issues of infection post-biopsy
- When did you get the results from the biopsy
- What was your layman’s understanding of the Gleason score
- How did you process learning about prostate cancer
- How was your conversation with your urologist about prognosis and treatment
- How did you and your wife process the diagnosis
- Treatment Decisions
- Video: Bruce Talks About Treatment
- Prostate Surgery (Prostatectomy)
- What was important to know heading into surgery
- Changing diet and exercise pre-surgery
- How was the prep before surgery
- How were you mentally prepared for the surgery
- Describe the CT scan
- Describe the bone scan
- Results of the scans
- Describe the prostate MRI (with rectal probe)
- The value of the prostate MRI
- Undergoing a pre-op physical
- How were you feeling going into the operating room
- What do you remember of waking up from surgery
- The surgery was quick in part due to your weight loss
- You had undergone a robotic surgery
- Recovering from Prostate Surgery (Radical Prostatectomy)
- Planning for More Treatment
- Salvage Radiation
- Hormone Therapy: Casodex & Lupron
- Video: Bruce on Quality of Life and Reflections
- Reflections After Treatment
- Keeping up with good diet and exercise
- Concerns about sexual function after surgery (prostatectomy)
- Keeping a sense of humor
- Survivorship
- What’s your message to other men on the importance of sharing, expressing, asking
- What does self-help mean (self-advocacy)
- The power of sharing your story
- Taking care of yourself after treatment
- Your "different" normal
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.

Meet Bruce
Tell us about yourself outside of cancer
Passionate about scuba diving though I don’t get to do it often now. I’ve been diving since I was a little kid. My older sister scuba dove and got us into that. Used to live in California and did that as a youngster.
I became a scuba instructor in 1983. The first (PADI) instructor class held in Egypt is where I got my instructor certification.
I was there for a couple of years with my then-girlfriend now-wife, Lisa, whom I met in college in California (see picture).
I love diving into the water. It’s very comfortable!
Video: Bruce on Getting Diagnosed
First Symptoms and Test
What were the first symptoms
I noticed that I couldn’t really control the velocity of my urination. Whether that was due to the prostate cancer or not, I’m not positive specifically, but at the time it was a bit concerning. But I was also getting older.
What happened at the first doctor visit
The doctor looked at it and did a digital exam. The conclusion given back to me was it probably was just me getting older. There was a blood test I could do but it wasn’t really reliable, it was controversial,
Besides, I was ‘too young’ to think about those things, anyway. I was 48 at the time, so they didn’t think it could be an issue of prostate cancer.
I had never even heard of prostate cancer and it was never mentioned in the discussion with the doctors. So at that point, I didn’t think much of it anymore, just chalked it up to me getting older.
Your brother’s prostate cancer diagnosis pushed you to get tested
It wasn’t until later in 2012 when my older brother contacted his male siblings and said he’d been diagnosed with a very aggressive prostate cancer. He recommended we get tested.
I planned to do that but I couldn’t recall what kind of cancer he mentioned. That’s the problem with the lack of advocacy. It just wasn’t in the normal, daily lexicon.
We just don’t know about it as younger men. Older men are much more versed in it because it’s known as an older disease, in general.
So when it came time to make the appointment, the medical staff asked what kind of cancer my brother had. I was thinking it was colon cancer. So I went and got my colonoscopy, which came out with flying colors.
I hadn’t heard of prostate cancer, so it wasn’t in my mind. That could have been a fatal mistake, and nearly was so.
It wasn’t until later in the fall that my brother followed up and asked if I had gotten my test. I said yes, that I had gotten my colon test and it was perfect. He said no, it’s a prostate test you need to take, the PSA, not colonoscopy.
So I called my doctor again and made an appointment to get tested for the PSA.
Was your brother going through prostate cancer treatment at the time
My brother was scheduled for surgery. It had escaped his prostate into other organs, so he had a much more dramatic surgery than I did.
When did you realize you may have prostate cancer
When I got the results from my physician on the first PSA test, she called me up and said she’d schedule an appointment with me with the urologist right away.
That’s not usual. They usually send you an email and you look it up online. That was when I first started really thinking that this would be really serious for me, as opposed to just my brother.
What is the PSA test
It’s a simple blood test. They draw a little bit of blood. There’s no fasting, there’s no extraordinary requirements.
One thing you can’t do is any sexual activity, so a lot of men will gripe about it. I believe it’s three days ahead of the PSA test you can’t have sexual activity or it will skew the results.
Men will brag and say that’s really annoying, in reality I don’t think any men are having sex that much at my age that they can’t withstand three days of waiting for the blood test.
It’s very simple, very easy. The PSA test, itself, when I was first talking to my original doctor, there was a lot of controversy on its efficacy. There were some studies done on the harms of the PSA test versus the actual deaths involved. So there’s recommendations to get away from doing the PSA test some years back. That was around the time I was getting it.
People equated the harms equally of getting and not gettin the PSA test, equating getting an infection from a biopsy or false-positive PSA to death.
To me, they’re not equal! One’s a lot worse than the other.
For the simple blood test, it’s an easy thing to do. The thing you have to think about for men looking at this for the first time, is you have to have some fortitude when you get the results.
The PSA level might be higher or elevated but it’s the doubling time, how rapidly it’s growing, that’s the issue.
So listen to your doctor, but you don’t want treatment without taking the PSA test later or following up with some other evidence, like a biopsy or digital exam. It might be when you take the second PSA test doubling time might be 100 or 25 or 30 years. By then you’ll die of something else other than prostate cancer!
It wasn’t my case, but in most cases, it can be a long time. At that time you do active surveillance, wait and see if it changes at all.
But don’t panic after your first PSA test, even if it’s elevated. It might be elevated but would take a long time for it to get somewhere problematic.

How long did it take to get the PSA level results
I got the results the next day. It was fairly quick. Normally with the doctor it took a couple of days, but this time was within a day.
Getting Diagnosed with Prostate Cancer
Describe the urologist meeting
My first question was wait, if this is cancer, why am I seeing a urologist? Prostate cancer is unique in that way in that it’s the urologist who takes the lead, generally, at first.
The urologist did a digital exam and said he felt some nodules but not to panic yet, that they would check another PSA test in three weeks to see if it changed at all, and if so, how much.
Results of the second PSA test
The PSA level had risen at least three points which in PSA terms, is a lot during three weeks. So it was appearing aggressive. At that point, the doctor recommended a biopsy.
Describe the digital exam
That’s where they probe with their finger, their digit up your backside. They are feeling the prostate to see if there are any lumps or forms they can feel that aren’t normal. That’s what they’re looking for.
It’s really just something you have to do, and I don’t want to say you feel violated, it’s just not that big of a deal. It’s very quick. They feel around, and then you’re done.
Considering the consequences of not doing it, it’s a pretty small price to pay in the small amount of discomfort. I feel way more pain when I’m trying to do my taxes.
Describe the biopsy
The biopsy sounds scarier than it feels. When they describe it to you, it can be terrifying. Going through it, it’s not that bad. You lie on your side and to reach the prostate, they take the needle and go through your rectum, take some tissue samples of your prostate.
Just the idea of a needle going up there sounds terrifying but they numb you up. You do feel a little pinching here and there as they collect the samples, but it wasn’t nearly as bad as I feared.
Recovering from the biopsy
There was a little pain for about a day or so. But the fact that it doesn’t stick in my head as being terrible means that it wasn’t that bad.
Again, someone has stuck a needle in you so it is sore there for a little while. But I was more afraid of infection than anything else, so again, I did everything the doctor said.
They mentioned there could be bleeding. I didn’t encounter much of that. You just take antibiotics and do some cleaning down there.
Issues of infection post-biopsy
There are issues of potential infection after so you have to be very mindful. Through this whole journey, do what the doctor says. That’s really key.
The doctor said do x, y, z, it works when you do what they say. If you do the oftentimes difficult or “male” thing, thinking I can do it myself, just do what the doctor says.
I don’t recall exactly what all the post-biopsy care was but they give you some antibiotics to make sure there are no infections. It has to stay clean.
It took just a few minutes once they got started. You feel some pinching but it’s no worse than someone pinching your skin, it’s a pin-prick type of sensation. When it’s all done, you have a lot more concrete answers.
When did you get the results from the biopsy
Gleason score is probably one of the most confusing aspects of the prostate cancer journey. I was at work at the time, and the doctor had the nurse give me a call.
The nurse called and said she was calling on behalf of the doctor. It was a very busy day for me and she asked if it was okay to give me my results over the phone. I was thinking sure, I had so many things to do, so fire away.
She gave my Gleason score and said the biopsy was positive for cancer. All the cores were positive for prostate cancer and I had a Gleason score of three plus three, and three plus four, measured as a 6/7 score.
That was kind of it. She said they’d be back in touch with me and the doctor would schedule a follow-up appointment. I left it there because she didn’t sound alarmed, so I wasn’t too alarmed.
But when I got home and started doing research, I didn’t really understand what she told me. Then I realized okay, this sounds moderately bad in terms of Gleason scores.
What was your layman’s understanding of the Gleason score
There are two numbers there and they have to do with the aggressiveness of the cancer. What they view in the microscope of how disorganized the cancer seems to be.
So the first number is the most prevalent amount and the second number is the lesser prevalent amount of aggressiveness and disorganization of the cancer cells. That’s my layman’s understanding of it. Then there’s a left side and right side, so you generally get two sets of numbers.
How did you process learning about prostate cancer
I knew it was concerning for my brother, but again, since I didn’t know much about prostate cancer and hadn’t heard much about it, I didn’t think it was a big deal in terms of risk.
Then as I started reading about it, once I was diagnosed, I realized just as many men died a year of prostate cancer as women do of breast cancer. That was really the stunning statistic that hit me.
The other thing is when you look at it, there are two different sides of the story that are equally true, but give different pictures.
On one hand, you hear a lot about prostate cancer not often being fatal and that usually, it’s mild, and most men don’t really have a problem with it. That’s true. It may be for some men.
But the other half of that coin is how many men have it. And when you have that many men have it, it’s very ubiquitous as you get older, the absolute numbers of deaths are very high.
So while on one hand the percentage of men who have serious problems are small, but the sheer number of men who have it drives that number of those with serious problems in real time very high.
It wasn’t until I started reading about that when it really struck me that this could be bad.

How was your conversation with your urologist about prognosis and treatment
That appointment was grim. I had already done some reading. The “seven” score was the part that resonated with me as not a good number to have since it was out of scale of ten. Your six, seven score is moderately aggressive, and your eight, nine, ten scores are bad.
So my wife and I went into the appointment and it was very sobering, if not downright scary. They started showing me these charts. We had this conversation that they’d have to take action on this because it wasn’t good, it was very aggressive, looking at the Gleason score and how fast the PSA was rising.
The urologist said my life depended on this. Those charts showed the survival rate which was very grim and scary. That was a very unsettling meeting. It took about 45 minutes to an hour as we muddled our way through it.
Most of the time, he was speaking to convince me and my wife that we needed to take action, and fast action. He was also trying to explain the range of options available.
At that time, I was still trying to get my head around the first things he was saying, like it was not a good Gleason score number to have.
As frightening as it was, you have to stand back and look at as we contemplate those survival curves, they’re normal bell curves, which means most people are in the middle and you get a few on the extreme ends on the higher and lower ends.
Our strategy was to look at this like there’s a reason some people are falling on one end or the other of the bell curve. It’s a random sampling of the general population.
So we needed to focus on what we could do, what we had control over, that could put us on one part of that curve of another.
That’s where our mental attitude had to be: what is in our power to change that we could have control over?

How did you and your wife process the diagnosis
Coming out of the meeting, we were shell-shocked. I honestly don’t know if the intent was to make sure that we did the treatment, that we didn’t blow it off.
One of the problems they have with the recommendations with the PSA test is the concern of men going out and getting radical treatment, like getting surgery after one test.
That was apparently very prevalent then. Then getting prostates removed that didn’t need to be.
I think part of the motivation behind the PSA recommendations, and they said this much in the study, was to drive that down. But we were on the opposite end. The urologist was trying to make sure that we took action and didn’t take it lightly. He succeeded in convincing us.
It was scary, very scary. Moving from that, it’s about trying to get information. As you try to cram for any test or learn anything, there’s so much information out there. But then I did get a second or third opinion in seeking other advice based on the tests.
»MORE: Patients share how they processed a cancer diagnosis
Treatment Decisions
Tip: get help and support from others from the start
For people who get a high Gleason score and an outcome where the doctor feels it’s very concerning, you don’t necessarily want to do all the research yourself. That’s really a bad idea because as we know, the internet is full of exaggeration one way or the other.
It’s hard to find definitive, scientifically-based information, and so it’s helpful to have a family member, in my case my sister, who did a lot of research for us and helped us out.
She could look at it from a more neutral eye, rather than trying to terrify ourselves by what we were reading and then fundamentally discard the information.
Learning from others who’d been through treatment
One thing I wish I had done earlier was go to a prostate support group of some sort. I didn’t do that until my treatment was well along the way.
I learned things there, hearing things being said, that would have been very helpful before going into surgery and before deciding treatment. The hardest part was trying to decide what treatment to go for.
What were the top tips you wish you had known earlier
The tough part was knowing what to expect. I just wanted to hear other people talk.
I don’t know if this is universal but I went to two different support groups. One was a general cancer support group and one was a prostate cancer support group.
I went to the general one first and there was a lot of emotion, which isn’t bad, but a lot of people going through some rough times. The session I attended, I was the only one with active cancer.
Most of them were people who had survived the cancer and were terrified about it coming back. A lot of talk was the emotional part of it, which has its benefits.
But when I went to the prostate support group, it’s largely a bunch of older men who have time on their hands because most of them are retired. They know a lot about the X-ray machines, the procedures, the topics.
I sat there and they’re bragging about whose is better. I realized I didn’t know enough, sitting in this group. These guys knew their stuff! There was no or little coddling, at first. There was a lot more bravado.
As it moved on, I realized there was a lot to know. One of the things, from my own research and family research, is the outcomes are kind of the same statistically, regardless of treatment. So you’re looking at the extra features to make the decision.
It’s like a car. All the cars on the lot drive and have the same basic, core features. So what are the luxury items or the features you want to live with later? That’s the same way with prostate cancer.
For example. In radiation treatment, it was far less invasive and a lot easier as an initial treatment. But there’s still a chance you have some residue PSA there that you have to keep an eye on.
Certainly some of the radiation treatments now are very focused on the area so there’s less tissue damage around it.
Surgery is more radical in that you’re taking the whole thing out. But I opted for that choice because I knew once it was out, it’s not coming back, if everything worked well.
I was wrong for my own situation, but at least at that point, if there’s PSA, it’s due to cancer and not to anything else.

Weighing pros and cons of surgery vs. radiation
With radiation, a lot of guys I knew opted for that because it was easier for their routine. They didn’t like the idea of someone cutting into them or going in and removing something.
On the other hand, for some men, removing the prostate is not needed necessarily, so a lot of people will say it’s cancer, let’s get rid of it, and be done. So you have both lines of thought.
Most people I knew who opted for radiation was out of convenience for doing it that way. It didn’t really impact their lifestyle very much.
Video: Bruce Talks About Treatment
- Radical prostatectomy (surgery to remove entire prostate) and recovery
- Getting restaged to 4A and Gleason score 8/9 (instead of 6/7)
- Salvage radiation
- Hormone therapy (Casodex and Lupron)
Prostate Surgery (Prostatectomy)
What was important to know heading into surgery
One of the best things, something I didn’t know at that time, wouldn’t impact the surgery too much. But rewinding a little, my PSA had been rising very rapidly. I looked at things I was in control of, what I could mitigate to help save my own life.
After talking to doctors at Johns Hopkins, and looking at materials from Mayo Clinic and the NIH, diet and exercise were things I could control.
There was a study relating to a low incident of prostate cancer in China versus the United States. They tracked immigrants to the U.S. Those men soon had the same rates of prostate cancer as the other people in the U.S.
That takes the genetic part out of the equation, so there’s definitely some environmental part in this. At the time, it was mostly looked at as red meat in the diet.
Changing diet and exercise pre-surgery
I shifted to a complete vegetarian diet and then exercised like a madman. I also dropped out of the workforce.
I took time off of work because after that meeting with my doctor where he gave me the grim results, I was talking to my staff and said I just didn’t feel like coming in.
One of my senior colleagues said then don’t come, we’ve got this, we’ll take care of this. Don’t worry about this. So I researched the options for me on treatment and decided on the surgery, but I exercised every day. I was riding about ten miles a day on the bike.
It flattened my PSA. It didn’t rise anymore after that. In that short period of time, I can say it slowed things down, but as a consequence, I had also lost a fair amount of weight, about ten pounds during that time. My surgery was very quick.
The doctor came out and said the surgery was normally a lot harder to do because of the amount of fat. But with me reducing the amount of fat I had, it made it a lot easier for the surgeons.








