Blogs>Taking charge and finding new treatment options for MBC: Tammy Uhl
With the right medical team, Tammy Uhl found hope and a game changer in breast cancer treatment
On Labor Day weekend 2020, just months after the start of the COVID-19 pandemic, Tammy Uhl of Green Bay, Wisconsin, learned she hadstage IV breast cancer.
Originally diagnosed in 2014 at age 42 withstageIIB,estrogen receptor-positive, HER2-negative breast cancer, Tammy had undergonesurgery,radiation, andchemotherapy. She thought she was in the clear and resumed her active life. She juggled her roles as a court reporter and closed captioner for the deaf and a mom to three school-aged children, all while maintaining her passion for distance running.
A few years later, Tammy had some back pain, which aradiologistdiagnosed as a benign growth in her spine. In 2020, she experienced worsening knee pain. Given her active lifestyle, she chalked it up to the wear and tear of exercise and sought help throughphysical therapy. Eventually, anMRIof her knee revealed that she had cancer throughout her femur (thigh bone).
After a series of orthopedic procedures to stabilize her spine and femur, as well as radiation to those areas and her hip, Tammy started on the CDK 4/6 inhibitor abemaciclib (Verzenio) and theendocrine therapyfulvestrant(Faslodex)—due to the cancer’s estrogen receptor-positive status—anddenosumab(Xgeva) to prevent bone fractures.
By early 2022, an MRI revealed yet another possibleprogression, this time in the hip. Tammy’s orthopediconcologistperformed a hip replacement and said he couldbiopsyany cancer found at that time.
Because Tammy’s family had moved to a new community near Green Bay in 2020, she was working with a newmedical oncologist. Even before the biopsy results came back, she recalls, “His attitude was, ‘enjoy the time you have left, there are no other options for you.’” He prescribed weeklyintravenouschemotherapy and told her it was “unlikely” she would live to see her son’s high school graduation in 2024. Her doctor also recommended that she quit her job and go on disability—which she did.
The silver lining of leaving her job was that it gave her more time to do research, join online breast cancer communities, and advocate for awareness. “I have thrown my life into advocacy and sharing my story,” Tammy says. “That's how I fill my days.”
But her oncologist’s words also sent her into what she calls “a very dark spiral.” Tammy had consulted with a breastspecialistat the University of Wisconsin Carbone Cancer Center (UW-Carbone), who suggested a liquid biopsy: a test that analyzes the blood sample for specificgeneticmutations that could influence treatment decisions. The results might indicate which existing therapies are most effective for her cancer or if she is eligible for aclinical trial. But Tammy’s medical oncologist dismissed the idea.
It was time for a change.
Determined to be an active participant in her treatment decisions, Tammy delved deeper into research. As she says, “It helps me to have information and stay on top of the knowledge of what’s coming.” She discovered she had options besides chemotherapy.
Tammy sought areferralfrom the UW-Carbone breast specialist and switched to another medical oncologist in her community, who was a much better fit. “His attitude was, ‘I will never take away your hope,’” Tammy recalls. “Hope is everything; this is what this whole process is about. It’s not that we aren’t going to face hard decisions. But we hope to get more time.”
Tammy also consulted with oncologists at M.D. Anderson Cancer Center in Houston, Texas, and the Mayo Clinic in Rochester, Minnesota. Because Mayo was within driving distance, she decided to continue there while also working with her local oncologist and the breast specialist at UW-Carbone.
Getting multiple opinions felt especially critical because the biopsy of Tammy’s hipmetastasistested negative forestrogenreceptors, a significant shift from her originalER-positivediagnosis. This change, sometimes known as “flipping” from ER-positive to ER-negative, could impact her treatment options significantly. But, as Tammy says, “Bone biopsies aren’t the most reliable,” especially after radiation, which can affect the bonetissueand therefore muddle the accuracy of readings.
Tammy also had done two liquid biopsy tests, neither of which showed any actionable mutations, leaving her team without the information they needed for treatment options that would be based on her cancer’s genetic makeup.
Without clear answers, she and her team decided to continue her ER-targetedregimen. When another progression occurred a year later, Tammy started oncapecitabine(Xeloda), a type of chemotherapy. Still, the question remained: “Are we treating estrogen receptor-positive cancer, or aren’t we? It wasn't possible to biopsy the most recent progression.”
"Hope is everything; this is what this whole process is about. It’s not that we aren’t going to face hard decisions. But we hope to get more time."
Tammy Uhl
To get the answer, Tammy’s Mayo Clinic doctor suggested they consider a newer type ofPET scan, called FES PET, also known by the brand name Cerianna. Traditional PET scans use theradioactivetracerFDG, or fluorodeoxyglucose, to “light up” cancer cells based on how they take up glucose (sugar) more rapidly than normal cells. FES PET uses aninjectionof a radioactive tracer called fluoroestradiol F18 (FES), which specifically targets estrogen receptors so that doctors can see whether areas of metastasis are ER-positive or ER-negative.
In 2023, National Comprehensive Cancer Network guidelines stated that Cerianna could be used to determine ER status in people with recurrent ormetastaticbreast cancer.
Although Cerianna isn’t available everywhere, Tammy was fortunate that UW-Carbone offered it. She had the FES PET scan in March 2024, and her health insurance covered it. She says the experience was much like having a traditional PET scan: about an hour wait after the injection to allow the tracer to move through the body, and an hour for thescanitself.
“Once the results came back, they showed I have a mixture: Some areas were estrogen receptor-positive, but some were clearly ER-negative,” Tammy says. The cancer had always been classified as HER2-negative as well, but her past scores on that test had been 1—suggesting that it was actually HER2-low. This mixed status suggested that continuing with ER-targeted therapies alone might not be effective.
Based on that information, her team started her ontrastuzumabderuxtecan (Enhertu), an antibody drug conjugate that targets HER2-low cancer cells more precisely.
“[Cerianna] made a huge difference in which route we were going to take,” she says. “Without it, I guarantee I would have gone on to try another CDK 4/6 inhibitor—and that would not have been good for me. There was no other way for me to have the right information.
“I’ve had two treatments so far,” Tammy adds. “There are a couple of challenging days, but I can still do what I want to do. So far, mytumormarkers are decreasing, so that is positive news.”
As a Hear My Voice advocate with LBBC, Tammy continues to share her story and learn as much as she can. “There are just so many opportunities for online learning. I was really focused on ER-positive treatment options before, but now I’m also focused on HER2-targeted options,” she says.
She’s planning a summer RV trip to Niagara Falls and New York City with her husband, her two daughters, now in their early 20s, and her 18-year-old son. In June, she was there when her son graduated from high school. And she can’t help but think of the oncologist who told her she wouldn’t reach that milestone.
“By him saying what he said, it really led me down this path of getting other opinions, including access to FES PET,” she says. “He really set a lot of things in motion once I stopped myself from the downward spiral.”
Because the areas of metastases are too difficult to biopsy, Tammy is glad to have Cerianna as an option for future treatment planning. And being an advocate remains important to her: “If my story touches just one person, to me, it’s worth it.”
DISCLAIMER:
The views and opinions of our bloggers represent the views and opinions of the bloggers alone and not those of Living Beyond Breast Cancer. Also understand that Living Beyond Breast Cancer does not medically review any information or content contained on, or distributed through, its blog and therefore does not endorse the accuracy or reliability of any such information or content. Through our blog, we merely seek to give individuals creative freedom to tell their stories. It is not a substitute for professional counseling or medical advice.
Metastatic
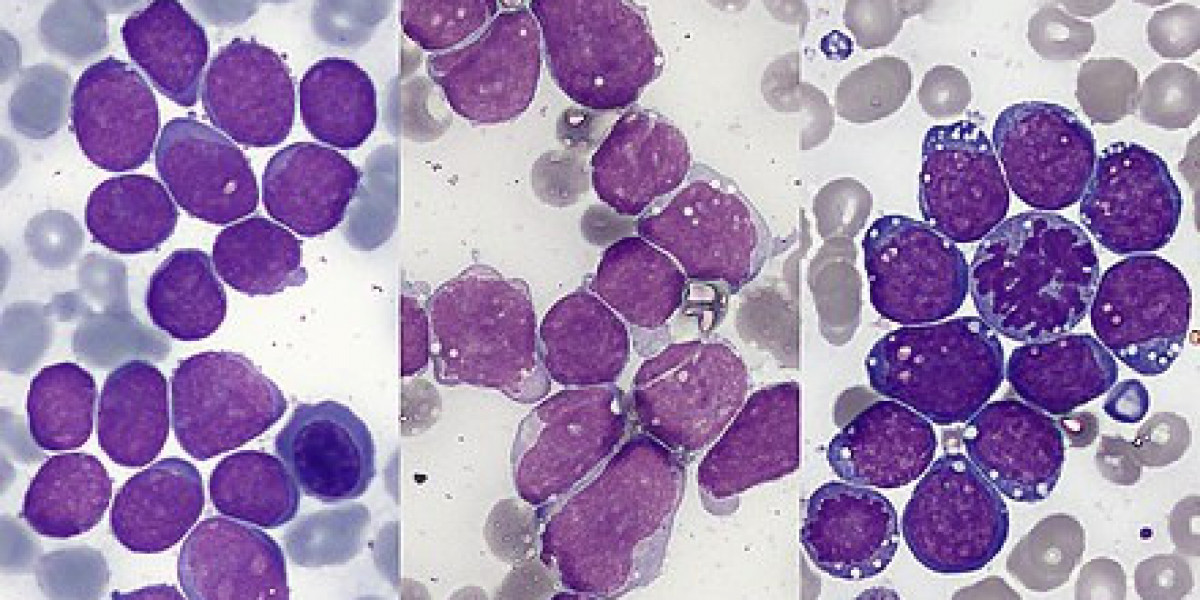
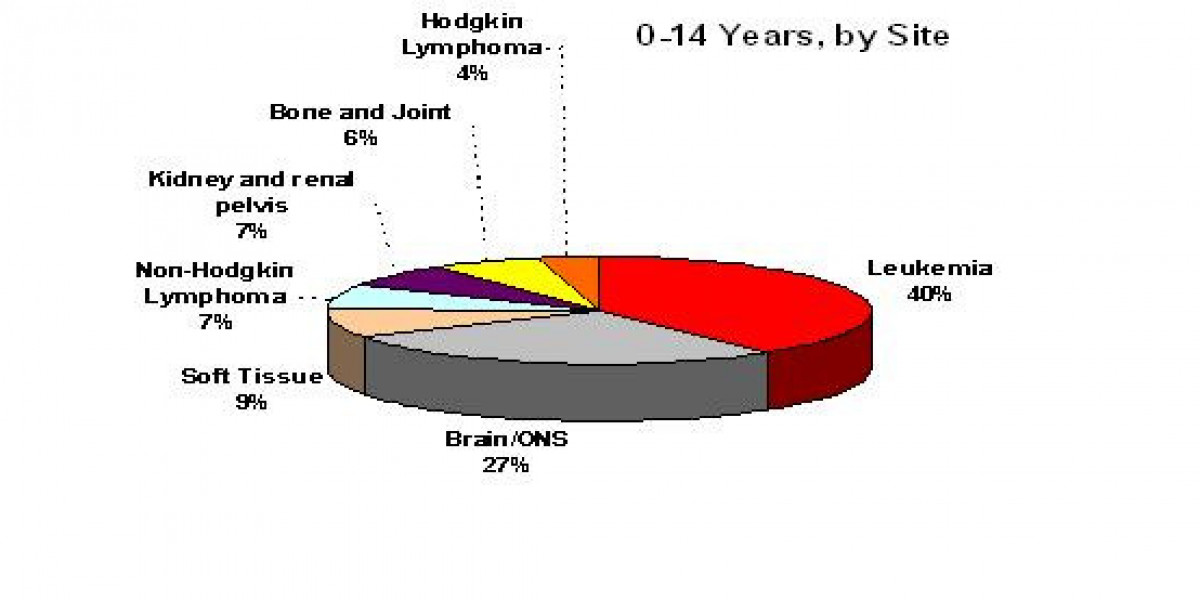
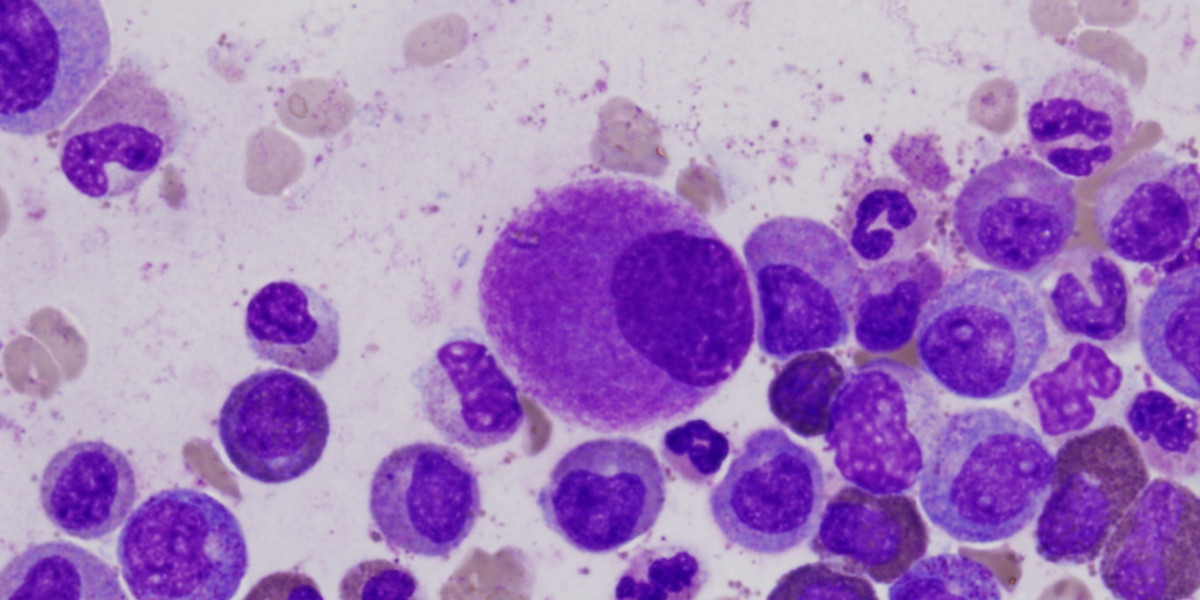
Metastatic breast cancer describes a type of breast cancer in which the cells have broken away from their original location to form a new tumor in different tissue or a different organ.
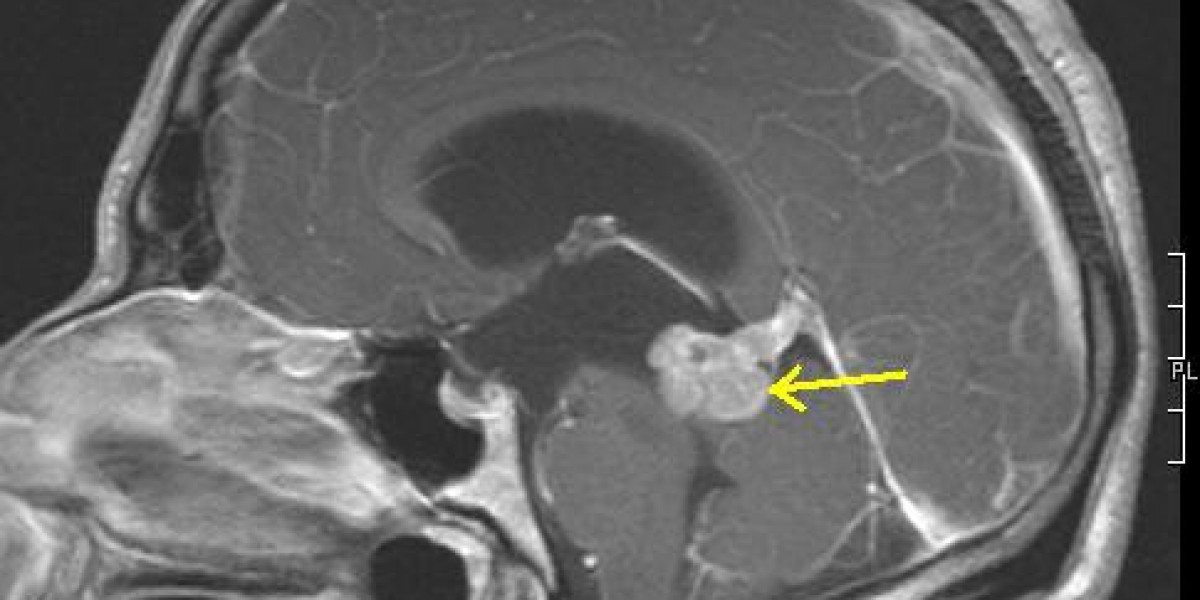
Metastatic breast cancer to the brain
Metastatic breast cancer to the brain is one of the most common locations breast cancer can spread to.
Living with Metastatic Breast Cancer
Living with a metastatic breast cancer diagnosis can be overwhelming, but there are many ways to adapt to your situation and find the support you need.
Living well with metastatic breast cancer
A metastatic breast cancer diagnosis can be one of the biggest challenges of your life, but there are many ways to continue living well emotionally and physically.
Tests for metastatic breast cancer
Many different tests can be involved in a metastatic breast cancer diagnosis. These tests can confirm the extent of the cancer and determine the most effective treatments.
Diagnosed with metastatic breast cancer
Hearing the words “You have metastatic breast cancer, and you will need ongoing treatment” can be traumatic. On this page, we’ll help you begin to make sense of your diagnosis, treatment options, and sources of support.
Hormone receptor-positive MBC
Learn more about hormone receptor-positive metastatic breast cancer, which means the stage IV breast cancer is hormone-sensitive.
Metastatic breast cancer and the workplace
Your job and your career path may be very important to you for financial and personal reasons. It’s normal to worry that a metastatic breast cancer diagnosis could affect your ability to work and earn a living.
Understanding health insurance with metastatic breast cancer
Understanding your health insurance options and what they cover is an important part of managing the costs of any long-term illness.
Financial matters and metastatic breast cancer
With a diagnosis of metastatic breast cancer, there are enough changes to navigate without the stress of financial uncertainty.
Sign up to receive emotional support, medical insight, personal stories, and more, delivered to your inbox weekly.
We'll send support straight to your inbox.
Kris Conner
Tagged:
Was this page helpful?
Living Beyond Breast Cancer is a national nonprofit organization that seeks to create a world that understands there is more than one way to have breast cancer. To fulfill its mission of providing trusted information and a community of support to those impacted by the disease, Living Beyond Breast Cancer offers on-demand emotional, practical, and evidence-based content. For over 30 years, the organization has remained committed to creating a culture of acceptance — where sharing the diversity of the lived experience of breast cancer fosters self-advocacy and hope. For more information,learn more about our programs and services.
Living Beyond Breast Cancer
40 Monument Road, Suite 104
Bala Cynwyd, PA 19004
©2025 Living Beyond Breast Cancer
Originally published on The Patient Story: https://www.lbbc.org/blog/taking-charge-and-finding-new-treatment-options-for-mbc-tammy-uhl