Table of contents:
Facing a leukemia diagnosis—whether yourself or a loved one—can feel overwhelming. It’s natural to have many questions, including what might have caused it.
While no one can say exactly what causes leukemia in adults or children, scientists have uncovered certain factors that may increase the risk of getting leukemia. These factors can be genetic, environmental, or lifestyle related.
Advances in research and treatment have brought hope to countless patients and families, and understanding the risk factors can help empower you with knowledge during a challenging time.
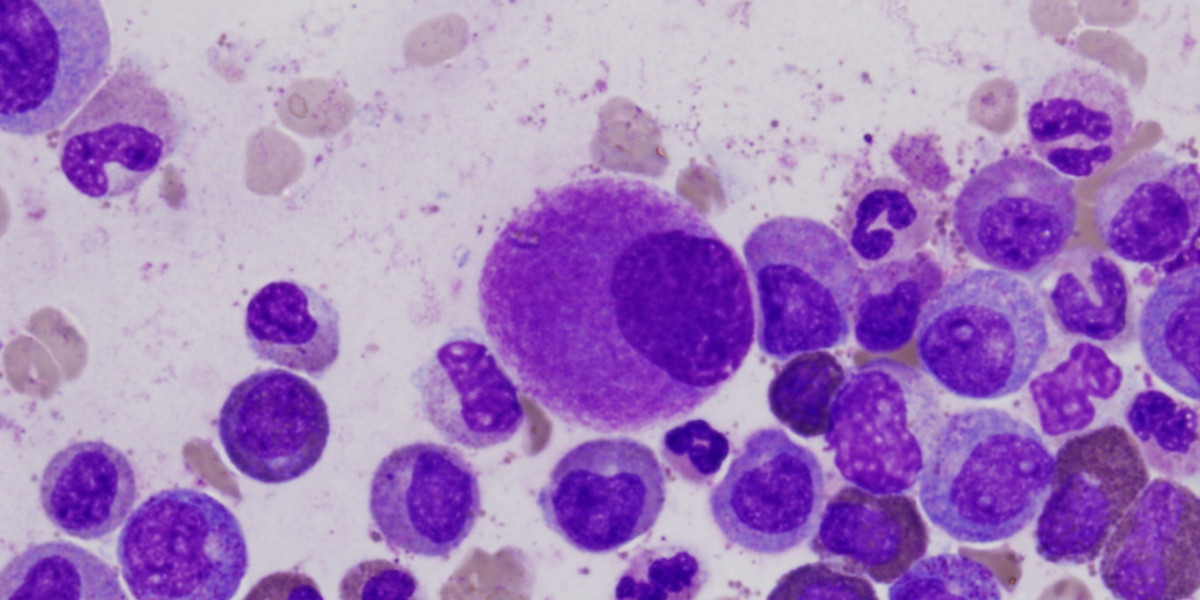
Leukemia is a type of cancer that affects the blood and bone marrow, where blood cells are made . It changes how these cells grow and function. Leukemia doesn’t usually have one clear cause, and for many, this uncertainty can feel frustrating or overwhelming.
Instead, leukemia is often the result of different factors working together. Some of these factors include genetic conditions that may increase the risk of leukemia, or having a first-degree relative with the disease, while others are related to environmental or lifestyle exposures over time. Together, they can affect your blood cells and how they work.
If you or a loved one are facing leukemia, it’s important to remember that this isn’t your fault. Many of these factors are beyond your control, and researchers are working tirelessly to better understand how they interact.
One of the biggest reasons for leukemia is genetic mutations . But what does that mean? Well, inside every cell in your body is DNA, which acts like a set of instructions telling your cells how to grow, divide, and do their jobs. Sometimes, something damages these instructions (the effects of aging or smoking, for example). This damage is called a mutation.
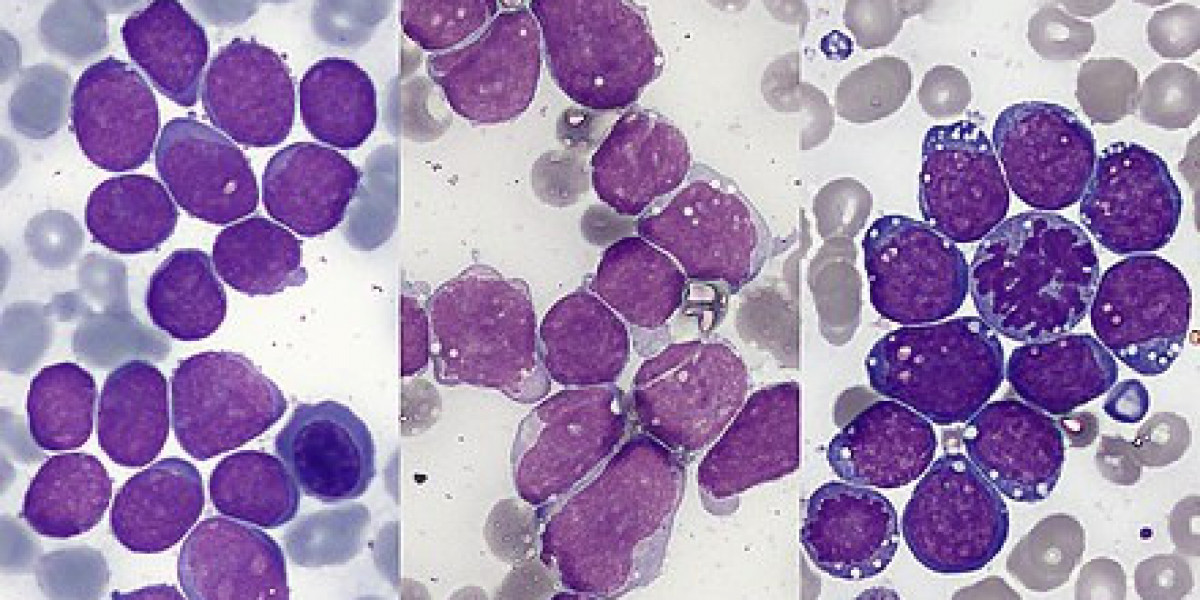
In leukemia, mutations happen in the cells that make your blood. These cells live in the bone marrow, the soft, spongy center of your bones where blood cells are created. When a mutation happens, it can cause blood cells to:
Over time, these abnormal cells crowd out the healthy blood cells your body needs to function (Leukemia 2022). This leads to many of the signs of leukemia, like feeling very tired, frequent infections, or bruising easily.
You might wonder, "If it’s related to DNA, does that mean leukemia is hereditary?"
For most people, leukemia is not inherited, meaning it doesn’t run in families. The genetic mutations that lead to leukemia usually happen during a person’s life because of other factors, like exposure to chemicals or natural changes as they age. As people grow older, their cells may not function as efficiently, and the likelihood of genetic errors increases. This is one reason why many diseases, including most forms of blood cancer, are more common in older individuals.
However, some people are born with certain genetic conditions that increase their risk of leukemia. For example:
If most leukemia isn’t inherited, then what leads to leukemia? What causes leukemia in adults? Scientists believe it’s often a mix of genetic mutations and environmental triggers. Here are some possible reasons (Chennamadhavuni et al. 2023):
It’s important to remember that just because someone has one of these risk factors, it doesn’t mean they’ll get leukemia. Many people develop leukemia without any clear reason.
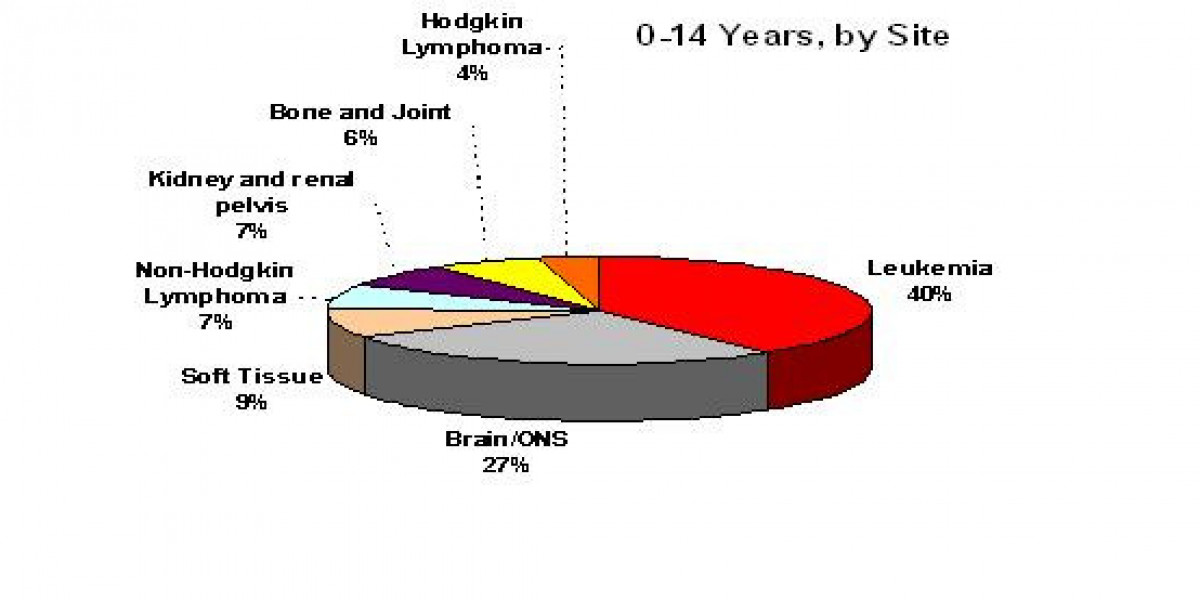
Leukemia is the most common type of cancer in children, but as with adults, the causes that lead to a diagnosis of leukemia in kids are still not fully understood. For some children, leukemia may be linked to genetic or environmental factors, while for others, it may happen for no known reason.
Hereditary conditions
Certain genetic and hereditary conditions can make children more likely to develop leukemia. For example (National Cancer Institute (US) 2024):
These conditions might change how a child’s blood-forming cells work, making them more prone to developing cancer.
Environmental factors
For some children, environmental exposures may play a role in developing leukemia. For example:
Kids with leukemia often show symptoms that may seem common at first but don’t go away. These can include:
If these symptoms persist, it’s important to talk to a doctor. While these symptoms can have other causes, it’s better to be safe and check.
When we talk about diseases like leukemia, you’ll often hear the term risk factor. But what does it actually mean?
A risk factor is something that increases the chances of getting a disease. Risk factors aren’t guarantees—they don’t mean you will get the disease, only that the likelihood is higher.
For leukemia, there are many risk factors, some you can control and others you can’t. Understanding these factors helps doctors and researchers learn more about what triggers leukemia and how to prevent or treat it.
Now, let’s look at the different leukemia risk factors. Some are tied to lifestyle choices, while others are things you can’t change, like your genetics or age (Chennamadhavuni et al. 2023).
Some risk factors of leukemia are tied to habits or exposures that we can manage or avoid. While controlling these risk factors won’t guarantee you won’t get leukemia, it may help lower your chances.
Smoking Smoking is a major leukemia cancer risk factor, especially for acute myeloid leukemia (AML). Cigarette smoke contains harmful chemicals that can damage your DNA, increasing the chances of mutations in your blood-forming cells. These mutations can sometimes lead to leukemia. Quitting smoking is one way to reduce this risk.
Exposure to cancer-causing agents Some chemicals, like benzene, are known to increase the risk of leukemia. Benzene is found in certain industrial settings and even in cigarette smoke. Long-term exposure to high levels of benzene can damage the cells in your bone marrow, where blood is made.
Other cancer-causing agents, like pesticides, are also linked to leukemia. Limiting your exposure to these chemicals—whether at work or in the environment—can help reduce your risk.
History of radiation therapy or chemotherapy If someone has undergone treatments like radiation therapy or chemotherapy for other cancers, they might have a higher risk of developing leukemia later. These treatments, while effective and often essential to fight cancer, can sometimes damage healthy cells in the bone marrow, leading to leukemia down the line. While this elevated risk is real, the benefits of life-saving treatments, such as CAR T-cell therapy or other cancer therapies, often far outweigh the potential risks. In many cases, these treatments are crucial for improving survival and quality of life.
Some risk factors for leukemia are things you can’t change. These are often tied to genetics, medical conditions, or your personal history. While you can’t do anything to change these factors, knowing about them can help doctors monitor your health more closely.
Myelodysplastic syndromes Myelodysplastic syndromes (MDS) are a group of disorders where the bone marrow doesn’t make enough healthy blood cells. Over time, these disorders can develop into leukemia, particularly acute myeloid leukemia (AML) (Dotson and Lebowicz 2022). People with MDS are already at a higher risk of leukemia and need careful monitoring by their doctors.
Rare genetic syndromes Certain genetic conditions can act as predisposing factors to leukemia, meaning they make someone more likely to develop it. These include:
Family history Having a close relative with leukemia—like a parent or sibling—may slightly increase your chances of developing the disease. However, most leukemia cases are not inherited. Scientists are still researching exactly how family history influences leukemia risk.
Certain viral infections While rare, some viral infections are linked to leukemia. For example, the human T-cell leukemia virus-1 (HTLV-1) is associated with a specific type of leukemia called adult T-cell leukemia (Durer and Babiker 2023).
Research shows that leukemia tends to be slightly more common in men than in women (“Leukemia - Cancer Stat Facts,” n.d.). Scientists aren’t entirely sure why this happens, but hormones, genetics, or environmental exposures could all play a role.
Leukemia isn’t just one disease—it comes in different forms, and each type has its own unique set of leukemia cancer risk factors. Leukemia fits broadly into four groups based on where it starts (lymphoid or myeloid cells) and whether it is fast (acute) or slow growing (chronic). This diversity in types means that the causes, progression, and treatments can vary significantly depending on the specific form of leukemia.
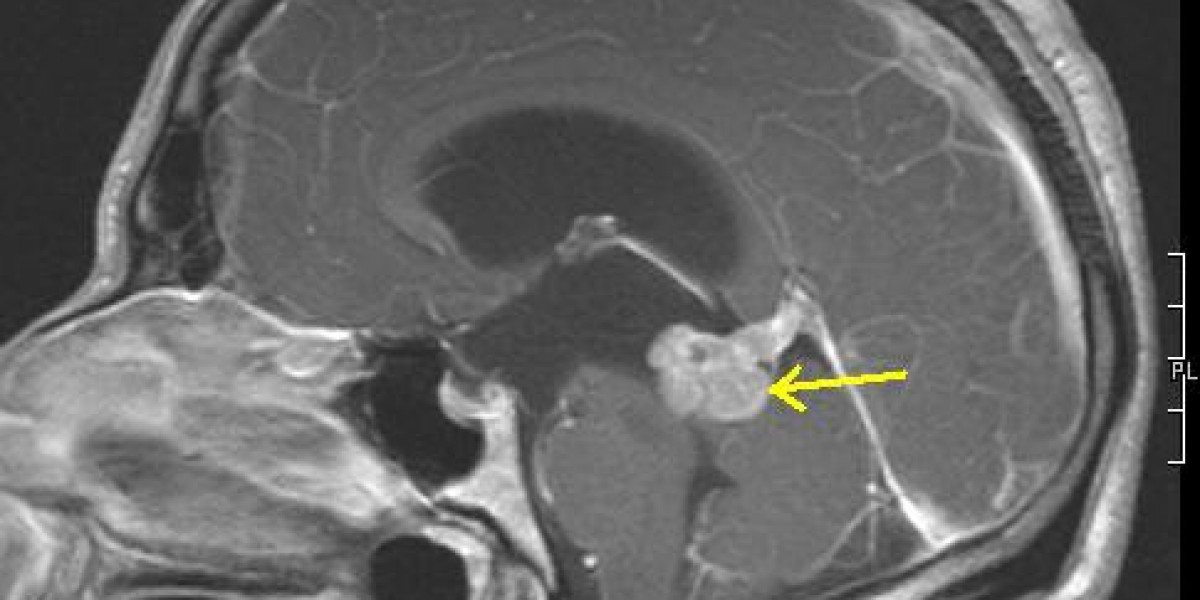
Acute lymphoblastic leukemia (ALL) Acute lymphoblastic leukemia (ALL) is the most common type of leukemia in children, with more than half of all cases occurring in this age group. Risk factors for acute leukemia, like ALL, include (Alaggio et al. 2022) things like exposure to high doses of radiation, such as from nuclear accidents or medical treatments.
Acute myeloid leukemia (AML) Acute myeloid leukemia (AML) is one of the most common types of leukemia in adults. Key risk factors include (Arber et al. 2022):
Chronic lymphoblastic leukemia (CLL) Chronic lymphoblastic leukemia (CLL) mostly affects adults and is more common in males than females. It’s not usually linked to lifestyle or environmental factors, but having a family history of CLL can slightly increase the risk (National Comprehensive Cancer Network, 2023).
Chronic myeloid leukemia (CML) Chronic myeloid leukemia (CML) is another type that typically develops in adults. It’s strongly associated with a specific genetic mutation called the Philadelphia chromosome, which changes how bone marrow cells grow (National Comprehensive Cancer Network, 2023b).
In addition to these risk factors, genetic and hereditary conditions including Down Syndrome, Bloom Syndrome, Li-Fraumeni Syndrome, and Fanconi anemia all increase the risk of various forms of blood cancer.
Leukemia, like many other cancers, cannot be prevented, and there’s no surefire way to stop it from developing. However, adopting healthy habits may lower your chances of developing leukemia or other health problems.
Many treatments help people achieve remission (when cancer is no longer detectable), and in some cases, long-term survival or even cure is possible. For example, pediatric acute lymphoblastic leukemia (ALL) has cure rates of over 85% with modern treatments, and most patients with chronic lymphocytic leukemia (CLL) and chronic myeloid leukemia (CML) can expect to live long, healthy lives due to advancements in targeted therapies. Thanks to research funded by LLS and others, treatment options are expanding and improving every day.
If someone you care about has been diagnosed with leukemia, your support can make a big difference.
The Leukemia & Lymphoma Society is changing the future of leukemia care. Thanks to donor support, LLS:
By donating to LLS, you’re helping families affected by blood cancer and contributing to life-saving research.
Leukemia is a challenging disease, but knowledge is power. Understanding the risk factors for leukemia, its causes, and the treatments available can help you or your loved ones navigate this journey. Remember, you’re not alone. The Leukemia & Lymphoma Society is here to support you every step of the way.
Consider making a donation today to help LLS fund critical research and support services.
Leukemia. 2022. Exon Publications eBooks. https://doi.org/10.36255/exon-publications-leukemia. ;
Chennamadhavuni, Adithya, Varun Lyengar, Shiva Kumar R. Mukkamalla, and Alex Shimanovsky. 2023. “Leukemia.” StatPearls - NCBI Bookshelf. January 17, 2023. https://www.ncbi.nlm.nih.gov/books/NBK560490. ;
National Cancer Institute (US). 2024. “Childhood Acute Lymphoblastic Leukemia Treatment (PDQ®).” PDQ Cancer Information Summaries - NCBI Bookshelf. October 7, 2024. https://www.ncbi.nlm.nih.gov/books/NBK65763. ;
Dotson, Jennifer L., and Yehuda Lebowicz. 2022. “Myelodysplastic Syndrome.” StatPearls - NCBI Bookshelf. July 18, 2022. https://www.ncbi.nlm.nih.gov/books/NBK534126. ;
Durer, Ceren, and Hani M. Babiker. 2023. “Adult T-Cell Leukemia.” StatPearls - NCBI Bookshelf. June 26, 2023. https://www.ncbi.nlm.nih.gov/books/NBK558968. ;
“Leukemia - Cancer Stat Facts.” n.d. SEER. https://seer.cancer.gov/statfacts/html/leuks.html. ;
Alaggio, Rita, Catalina Amador, Ioannis Anagnostopoulos, Ayoma D. Attygalle, Iguaracyra Barreto De Oliveira Araujo, Emilio Berti, Govind Bhagat, et al. 2022. “The 5th edition of the World Health Organization Classification of Haematolymphoid Tumours: Lymphoid Neoplasms.” Leukemia 36 (7): 1720–48. https://doi.org/10.1038/s41375-022-01620-2. ;
Arber, Daniel A., Attilio Orazi, Robert P. Hasserjian, Michael J. Borowitz, Katherine R. Calvo, Hans-Michael Kvasnicka, Sa A. Wang, et al. 2022. “International Consensus Classification of Myeloid Neoplasms and Acute Leukemias: integrating morphologic, clinical, and genomic data.” Blood 140 (11): 1200–1228. https://doi.org/10.1182/blood.2022015850. ;
National Comprehensive Cancer Network. NCCN Clinical Practice Guidelines in Oncology: Chronic lymphoblastic Leukemia/Small lymphoblastic Lymphoma. 2023.
National Comprehensive Cancer Network. NCCN Clinical Practice Guidelines in Oncology: Chronic Myeloid Leukemia. 2023b.
Originally published on The Cancer Research Institute: https://www.lls.org/blog/predisposing-factors-leukemia#can-leukemia-be-cured