Montessa’s Small Cell Lung Cancer Story
Montessa L., Small Cell Lung Cancer
Symptoms: Chest pain, lingering cough
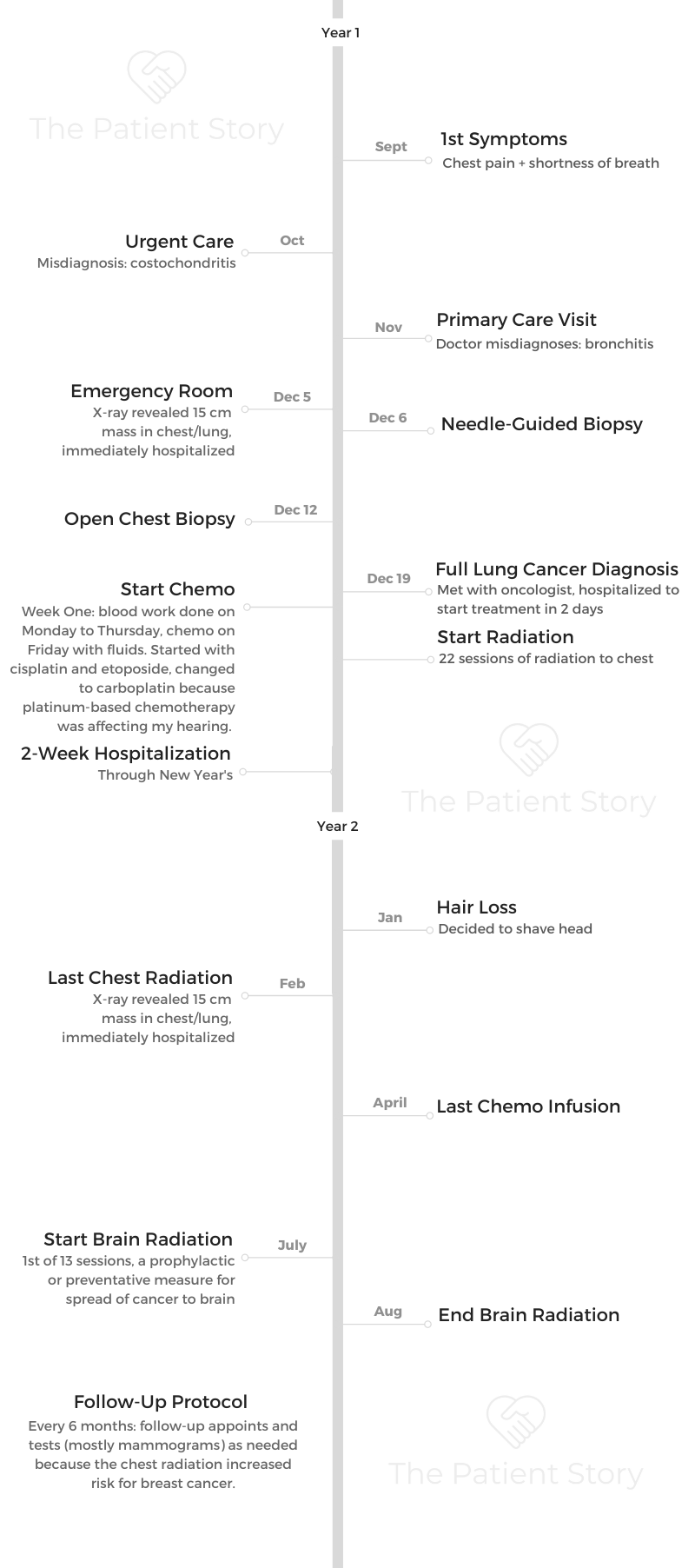
Treatments: Chemotherapy (cisplatin switched to carboplatin, etoposide), chest radiation, brain radiation (prophylactic)

Montessa’s Small Cell Lung Cancer Story
Montessa shares her small cell lung cancer story that started with a diagnosis at 28 years old. She highlights how she got through treatment, from concurrent chemotherapy and radiation to brain radiation, and recovery.
She also talks about how she navigated life with cancer, being a non-smoker blindsided by the lung cancer diagnosis, how she approached work and time off, finding support in a cancer community, and her lung cancer patient advocacy work. Thank you, Montessa!
- Name: Montessa L.
- Diagnosis (DX)
- Lung cancer
- Small cell
- 15 cm mass
- Age at DX: 28 years old
- 1st Symptoms
- Chest pain
- Lingering cough
- Treatment
- Concurrent chemotherapy and radiation
- Chemotherapy:
- Cisplatin & etoposide
- Then substituted cisplatin with carboplatin because of side effects
- Radiation: 22 straight days
- Chemotherapy:
- Brain radiation
- 13 sessions
- Concurrent chemotherapy and radiation
- Videos: Montessa's Story
- First Symptoms
- Diagnostic Tests & Procedures
- Lung Cancer Diagnosis
- Treatment Plan
- Chemotherapy & Side Effects
- Describe the chemotherapy treatment regimen
- What were the chemo side effects?
- Self-advocating to get the regimen changed (because of the fatigue)
- What were other side effects?
- Describe the hair loss and how you handled it
- Any tips on dealing with the hair loss?
- It was hot also because of the hot flashes from hormone therapy (Lupron)
- Radiation Therapy
- What was the radiation treatment regimen?
- Describe the actual radiation treatment
- What were the radiation side effects?
- Making treatment decisions
- Describe the plan with brain radiation
- Describe the brain radiation
- Any guidance to others on getting through this type of radiation?
- How did everything look at the end of treatment (final scan)?
- Navigating Life Through Treatment
- Were you able to drive yourself to the appointments?
- Do you wish you had taken more time off?
- Any guidance for others on how to approach work?
- The stigma of “not looking sick”
- Any guidance on how to deal with the PICC line?
- There are products that help with quality of life with things like PICC lines
- Support, Community & Advocacy
- How did you get through treatment?
- Asking for help is tough but necessary
- Importance of self-advocacy
- What are the top updates that small cell lung cancer patients should pay attention to?
- Find your cancer community
- Small cell lung cancer and new treatments
- The trend toward personalized and precision medicine
- The importance of diversity in research and clinical trials
- You see yourself as the ultimate advocate for others
- Small Cell Lung Cancer Stories
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
Videos: Montessa’s Story
How I Got Diagnosed
Treatment: Chemotherapy & Radiation
Navigating Life with Cancer
First Symptoms
Tell us about yourself outside of cancer
I appreciate that we can’t be defined by a box. Beyond patient advocacy, I’m a mentor teacher. Specifically, I work with novice teachers.
My background is a special educator. I have a master’s in autism and inclusion. I really prefer working in populations in our schools that have autism or any teacher who is working with a large group of children with special needs.
I do work for that, and I’ve turned some of the advocacy work I’ve learned from lung cancer into education. I am currently a doctoral student as well. With all of these things, I don’t know how I could keep my calendar and my mind managed!
What were your first symptoms?
I had chest pain, a cough. I remember because it was a day in September where we were having a going-away party. I have a friend in the military, in the Navy, and she was going to be stationed away.
That’s probably why that date and month stick in my head.
I went to the urgent care clinic. They poked around and said, “Oh, you have costochondritis, inflammation around the rib cage.”
It sounded legitimate because I had been working out that summer pulling weights. I don’t know, you trust the medical professionals.
They gave me Motrin, and I went on about my business. Then I developed a cough that wouldn’t go away. A lingering cough. The chest pain was still there.
Describe the first doctor’s visit
I went to a primary care doctor. This was a new doctor. I had never seen this doctor before going to meet her. They said, “Oh, you have bronchitis.” Never gave me an X-ray.
At the time, I was 28 years old. I didn’t know I was supposed to have an X-ray for bronchitis. I work in a school system with kids. I was like, “Sounds legitimate. Maybe the kids get sick. Maybe I just got sick.”
Then she said, “You have a whopping heart murmur. Anybody tell you that?” I was like, “No, nobody has ever told me this in my life, that I had a heart murmur.”
She was keen to the heart murmur. She sent me to go get an echocardiogram, but never gave me an X-ray and sent me home with an inhaler and antibiotics. November, I remember driving home.
I had back pain. I would have back pain throughout. Even my teachers I was working with would later tell me that I would complain about back pain, but I didn’t connect the two.
Trip to the emergency room (ER)
By the first week in December, I was in grad school for my master’s. The pain came back. I lived with my cousin at the time. I called her and said, “The chest pain came back. You have to take me to the ER.”

She’s like, “Oh no.” She had told me, too, that the cough was still there even after I had finished the antibiotics. I said, “Oh, I made another appointment. Maybe it just lingers. I don’t know how bronchitis works.”
She said, “Shouldn’t that cough be gone?” Red flags are coming out. I went to the ER at the regular hospital this time. I was in so much pain.
Ironically, by the time I got home from the grad square, I’m like “Oh, I have to take a test.” I have no idea even how I made it through the test because I was really in pain.
The pain had subsided, and I wanted to eat something. I was not worried. I said, “Maybe the ER can give me some medicine, so go ahead and take me to the ER.”
She took me, and they immediately hospitalized me after realizing my oxygen level was like 83 or 85.
They did an X-ray and said, ‘We found a mass, and we’re keeping you.’
All I heard was ‘IV,’ which meant needle in my head, and ‘biopsy,’ which meant surgery. I was like, ‘I have to go to work in the morning. No, I can’t stay here.’
I’m sitting in the bed, if you could imagine, sitting in the chair. My cousin’s standing above me, [saying], “They found a mass in your lung. You’re sick.” I’m like, “No.”
In my head, I’m thinking somehow I’m functioning, I’m walking around. I can’t afford these bills. I’m a teacher. Not knowing, the fear of the unknown. Right now, it’s all questions.
They said, “Do you want to see the X-ray?” I said, “Let me see.” I had no idea what I was going to see, but the way I describe it to people is if you have no knowledge of what your lungs are supposed to look like, if you look up in a dark sky with some binoculars, you’ll see dark lobes and maybe some white lines.
Imagine someone taking a paper towel, balling it up, and covering one of those lenses. Three-fourths of my lung on the left side was not visible. Only one-fourth was visible. That’s how large a 15-centimeter mass was by the time they found it.
Processing the gravity of the situation
I looked to my cousin and said, “Oh, I guess I’m staying.” I still had no idea. At that time, they were just whispering things like, “Oh, is it possibly cancer? Possibly not. We don’t know. We’re still going to do some tests.”
Actually, they said they were going to do all this before I saw the scan. Then it made sense. I understood. I visualized in my mind what the mass was that they were talking about.
Things started becoming clear, like why I was having trouble sleeping. Before, I thought it was my pillow [and] everything else.
Describe your mindset as a 28-year old non-smoker facing this diagnosis
My normal temperament would have been pessimistic, like, “Oh, well, it’s me.” Go into a hypochondriac mode.
That’s where my faith comes in and part of the book that I ended up writing.
I heard a voice of life whisper to me and say, ‘This is going to be bad, but it’s not going to kill you. It’s going to be a healing testimony for someone beyond yourself.’
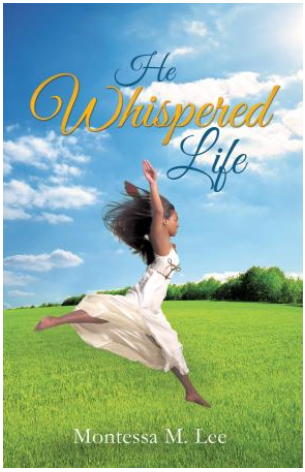
I didn’t know at the time whose story this was for or what journey I was going to go down, but I had to hear that because my normal temperament would have been, “Let me lie on the bed.” I would have been a worrywart, a “negative Nancy,” the whole way through the journey.
Everything happened rapidly. I didn’t have time to process, especially when you’re sick like that. They did immediately hospitalize me.
Diagnostic Tests & Procedures
Describe the needle-guided biopsy
That was the first time I was hospitalized. They did the needle-guided biopsies, where you sit on something like a CT scan or ultrasound. They can visually look at where they’re doing the biopsy. They get a syringe or a needle and take out the tissue. I believe I was awake. It was not as invasive.
I got a call back probably at the end of that week, and they said, “Hey, we didn’t get enough tissue sample. You have to come back in for an open chest biopsy.”
The doctors and surgeons were going back and forth, I think because of the theory of cell spreading. I didn’t know all the science behind what they were explaining at the time. I went back probably a week later.
Dealing with such a large mass
The surgeon at the time was trying to connect me with an oncologist. My cousin, who worked at another hospital, was actually on the call the whole time because he didn’t believe it the first time I was in the hospital with 15-centimeter mass.
He told me, “You must be mistaken. It is not a 15-centimeter mass.” I still had no idea that it was huge. Even though I saw it, I didn’t know it was abnormally huge. I just said, “Okay, it’s the size of a cantaloupe.”

The doctors were very calm telling me these things — until I went later on, and people I met in patient advocacy were like, ‘That was humongous!’
I was the talk of the water cooler probably because everybody would come in and say, “Was anything lighting up? Did you visibly show anything?” That was probably the medical student there.
Describe the open chest biopsy
I did break down and cry that time. I don’t know why they tell patients some things, but they’re like, “We can’t fully sedate you.” In my mind, I was thinking I was going to be awake.
It had something more to do with the intubation or something. They couldn’t do something because of me lying down flat on my back. I wouldn’t have been able to breathe, but I still was out enough that I do not remember anything.
Lung Cancer Diagnosis
What do you remember from getting the diagnosis?
It wasn’t until I met my oncologist that I got the diagnosis, even though they probably knew about the cancer because the surgeon was trying to connect me with an oncologist. I didn’t get the diagnosis until I met my oncologist that next week. The doctor was very, very calm.
I have a large family here. Before my mom came up from North Carolina, my extended family was driving me back and forth. A male cousin and I were in the office, and the oncologist said, “It’s a really stupid name. We used to call it oat cell cancer because it looks like oats in the microscope. Now, it’s small cell lung cancer.”
My cousin and I looked at each other, laughed, and said, “That is a dumb name.” He said, “We’re going to hospitalize you and start X, Y, Z.”
I asked if he could give me one more day because my mom and my aunt were coming in soon. I asked for one day before I had to go back to the hospital.
I don’t know if he willingly did it, but he caved in and let me wait one day until they arrived. I can’t remember the exact day, but it was one day in between. He let me wait, and then immediately I was back in the hospital again.
What were the details of your lung cancer diagnosis?
I started looking up what “small cell” was. I had no reference. My grandfather had died of lung cancer, but I still had really no reference of how deadly the disease was, especially the difference between small cell and non-small cell. I think the paper said “advanced.” It might’ve said “extensive,” because usually it’s extensive or limited.
I know I had limited, but I don’t know if the doctor put “extensive” on there as a call to speed up the process of things or because the tumor was so large at the time. They thought it was in the lung. By the time they found it, it was in the mediastinum area, but it had not metastasized.
I looked at it, thinking, “How could this be right?” Because again, my body wasn’t functioning at 100% by any means, but I was going day-to-day at work, and then immediately, everything stopped.

How did you process how the cancer would impact your life?
Looking back, I couldn’t wrap my head around it.
I took what he said and heard, “You’re going to start chemo. Your hair might fall out, might not. My patients usually don’t get nauseous because I give them X, Y, Z medications.”
I remember him talking about the type of chemo I was on would impact my kidneys and that I should drink a lot of water. I’m surprised I could remember all this, but he was telling me all of these things.
Describe the radiation treatment plan
My oncologist did say we’d start radiation, but the radiation oncologist talked more about that treatment side. I think he said after 6 or 8 cycles of chemo, we would start radiation.
Actually, they started a PICC line first, before I had another surgery, to start the first dose of chemotherapy when I was hospitalized.
»MORE: Read patient PICC line experiences
I didn’t know about some of these other issues, like I had fluid around my heart. I ended up getting a pericardial window when I was hospitalized at that time. They put a mediport in.
I don’t even remember him telling me if I was getting a mediport, but it was the best thing that could have happened when they did that surgery as well, to also put the mediport in.
I was there longer than they thought because the fluid wouldn’t drain off from that pericardial window. I remember him coming in because it was around Christmastime, too, so he was on vacation for some of that time. There were your physician assistants and others coming in during that time.
How did you break the news to loved ones?
That’s a good question, because I don’t even know if I called anyone to tell them. My cousin who was with me at the time, who lived with me, called the doctor. She also called my aunt, and she told her to call my cousin Keith, who’s an interventional radiologist at the hospital, and get us connected.
We got on the ball, and Keith also called over to the hospital to talk to the doctors to get the doctor language and get what was going on. My cousin called my parents and said I was in the hospital. They called another aunt. The chain got passed through.
My dad would always say, “Tell Montessa. Telephone or telegraph. Tell Montessa; it’ll get around.” I lived with some of my close friends from work, so one of them called the others, and they connected with my principal [manager at work]. Three of my really good friends from work ended up coming to the hospital that night.
»MORE: Breaking the news of a diagnosis to loved ones
Did you get a second opinion?
I was very happy with my oncologist. I trusted my family, so I went with him.
But I think people need to get second opinions. I’ve met several people now, all these years later, who all needed to get a second opinion. I have a friend now dealing with a different type of cancer who got a second opinion, because she didn’t want this radical surgery that they had recommended at first.
We patients have to be educated.
All they can do is tell you no or yes if you go get the second opinion. I didn’t go to one — I won’t name the hospital or treatment center — because I had a coworker who said they treated her husband like a specimen or a research project.
They weren’t looking at a holistic approach, and I needed somebody a little bit more personable. I just wanted to stick with my oncologist.
Treatment Plan
Describe the start of treatment (chemo, surgery, radiation)
Originally, because they wanted to start the chemo right away, they started a PICC line.
I won’t forget this either, even though I do say sometimes chemo has affected some of my memory, but they put the PICC line in.
I remember it wasn’t pointed in the right direction. They had to go back down to interventional radiology to get pointed in the right direction, and these things in my mind when they’re like, “We can’t get it.”
Again, I don’t know why they tell patients all these things, but they were like, “If we can’t get it to work through your arm through here, we have to go up through your thigh or something.” I’m like, “Oh no,” but they got it working and started the chemo right away.
I must have had the surgery after that first round. They put the mediport in and did that pericardial window. I started radiation when I was hospitalized as well.

The important role nurses play
I remember one of the nurses saying, “I want it to be there to start the chemo,” which was quite interesting. It shows you that personality and the bedside manner of the nurses. They started the chemo then.
You had to travel between different treatment centers
There was a different little caveat because when I was released from the hospital, my oncologist had me go to an infusion center at another hospital, but the radiation oncologist was at the original hospital. I’ll say hospital A and B. I would have to get picked up, and the church arranged rides for me.
This was just miraculous. They arranged rides for me to be picked up at my house and took me to radiation treatment. Somebody picked me up from the radiation hospital A and took me to B to get the chemotherapy on the days that I had both radiation and chemo.
Chemotherapy & Side Effects
Describe the chemotherapy treatment regimen
The chemo would be cycles of like 3. Week 1, I’d have blood work done on Monday, Tuesday, Wednesday, and Thursday. Then I’d get chemo Friday.
I’d get fluids. They started with cisplatin and etoposide. Eventually, I had to change to carboplatin because I had ringing in my ears. The platinum-based chemotherapy was affecting my hearing.
Somebody would pick me up [and] take me to the hospital every 3 weeks. That week it would be chemo week, and my mom would come up from North Carolina [on] those weekends when I had chemo treatment. Then I would have another week of blood work. It was always blood work, then chemo week.
What were the chemo side effects?
Every 3 weeks, I’d have these chemo weeks. Then it got to April. I was so fatigued that the doctor had to change the regimen a little bit. I had to take a week off of the chemotherapy treatment.
That type of fatigue, I can’t even describe it. Even to walk from my apartment around the corner to a neighbor’s apartment took every bit of energy that I couldn’t muster up.
»MORE: Cancer patients share their treatment side effects
Self-advocating to get the regimen changed (because of the fatigue)
Yes, because in my mind, I didn’t think that my oncologist was going to do anything. I give him credit, too, because from my other little advocacy groups I’ve been a part of, sometimes they say that the doctors don’t even ask them as a whole picture of, “How are you doing? Are you having any insurance problems, money problems? What are your issues? How are you?” Not just the treatment of the disease but, “How are you?”
I just told my oncologist, “Hey, I’m so worn out, very fatigued.” That week (off) actually made a difference. It helped.
What were other side effects?
Like my oncologist stated at the very beginning, a few of his patients get nauseated. I think he tries to get out ahead of that and have patients handle the nausea. He said, “You should drink water.”
The days I was nauseated were the simultaneous days of radiation and chemo. I would go to chemo those next mornings, and I would feel a little queasy. Those mornings, I tried to drink water and tried to stay hydrated.
Describe the hair loss and how you handled it
The hair fell out after I got out of the hospital, and my mom helped me comb my hair. Like a little office trash can — my hair at the time, I had an Afro, and so all of my hair completely filled that trash can, just coming out in clumps. I had little sprigs of hair. I went to my hairdresser and just got it shaved off, and it was bald.
I had come to the resolution before that I wasn’t going to wear a wig, because it was too hot for me. I didn’t know what my head was going to look like underneath, but I just resolved to the fact that I would be bald.
»MORE: Patients describe dealing with hair loss during cancer treatment

Any tips on dealing with the hair loss?
Yes, I just went through this with my friend who was just recently diagnosed with uterine cancer. When an oncologist tells you, “You could lose your hair. It could not. Maybe it’s going to stay in.” Right then is when I decided, “I’m going to get some hats, or I wear some scarves. I’m not going to wear a wig.” In my head, I had already decided.
I didn’t know what my head was going to look like. I still didn’t know for sure what was going to happen. I didn’t know what that process of losing my hair was going to look like.
My scalp became tender, and it hurt when my hair fell out. Who knew?
My hair was braided when I was in the hospital. Then coming back out and having that Afro, the hair was just coming out in clumps. When the hair was scraggly on my head, I said I looked like a cancer patient.
That’s very stereotypical, but my hair looked like little sprigs coming out of it. I said, “It’s better just to get it clean shaven, and maybe it’ll grow back even.”
My mom was there with me at the time. We went over to the hairdresser, and I remember her closing the door to give me some privacy. The hairdresser just cut it off.
Wigs are beautiful. Now I see a lot of very stylish ones. I just didn’t want it because it was so hot. It would feel like it was hot on my head, but you’ll see in some of my other advocacy pictures, I used to wear a wig to chemo, sometimes Afro wigs, and I acted like that was my hair again!
It was hot also because of the hot flashes from hormone therapy (Lupron)
I did have hot flashes. I remember joking with my coworker at the time. She was older, and she would always have a fan on. “It’s always so cold in here.” “Don’t turn this fan off.”
Then I said, “I know what you’re going through now because having these hot flash attacks now, I can’t joke with you anymore.” It’s like, “Now I understand. Now I can walk in your shoes. I understand why you have the little fan on.”
Radiation Therapy
What was the radiation treatment regimen?
The radiation oncologist explained it was going to be 22 days straight of chest radiation. They were going to resize and re-image the area.
They wouldn’t be radiating good tissue, because with small cell lung cancer, it usually responds well to that first round of treatment, but it tends to come back. The goal was, of course, to shrink that tumor with simultaneous radiation and chemo at the same time, so they explained.
Describe the actual radiation treatment
For the radiation treatment, it was very painful initially to lie down flat. It was extremely painful. It was so hard to breathe that I would cough.
All of these tests — MRIs, CAT scans, the radiation treatment — you had to lie down flat. I had to come up with a systematic way of lying there. I closed my eyes, and the machine moved over me.
I would count how many times it moved to know how close the treatment was to being over. I’m counting, like, “One, two,” in my head. I visualized how many times I had to move and get up from the radiation treatment.